Search
- Page Path
- HOME > Search
- Miscellaneous
- Incidence of Endocrine-Related Dysfunction in Patients Treated with New Immune Checkpoint Inhibitors: A Meta-Analysis and Comprehensive Review
- Won Sang Yoo, Eu Jeong Ku, Eun Kyung Lee, Hwa Young Ahn
- Endocrinol Metab. 2023;38(6):750-759. Published online November 13, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1785
- 1,431 View
- 120 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
This study investigated the incidence of endocrine immune-related adverse events (irAEs) for recently developed immune checkpoint inhibitor (ICI) drugs.
Methods
We collected studies on newly developed ICI drugs using PubMed/Medline, Embase, and Cochrane Library from inception through January 31, 2023. Among ICI drugs, nivolumab, pembrolizumab, and ipilimumab were excluded from the new ICI drugs because many papers on endocrine-related side effects have already been published.
Results
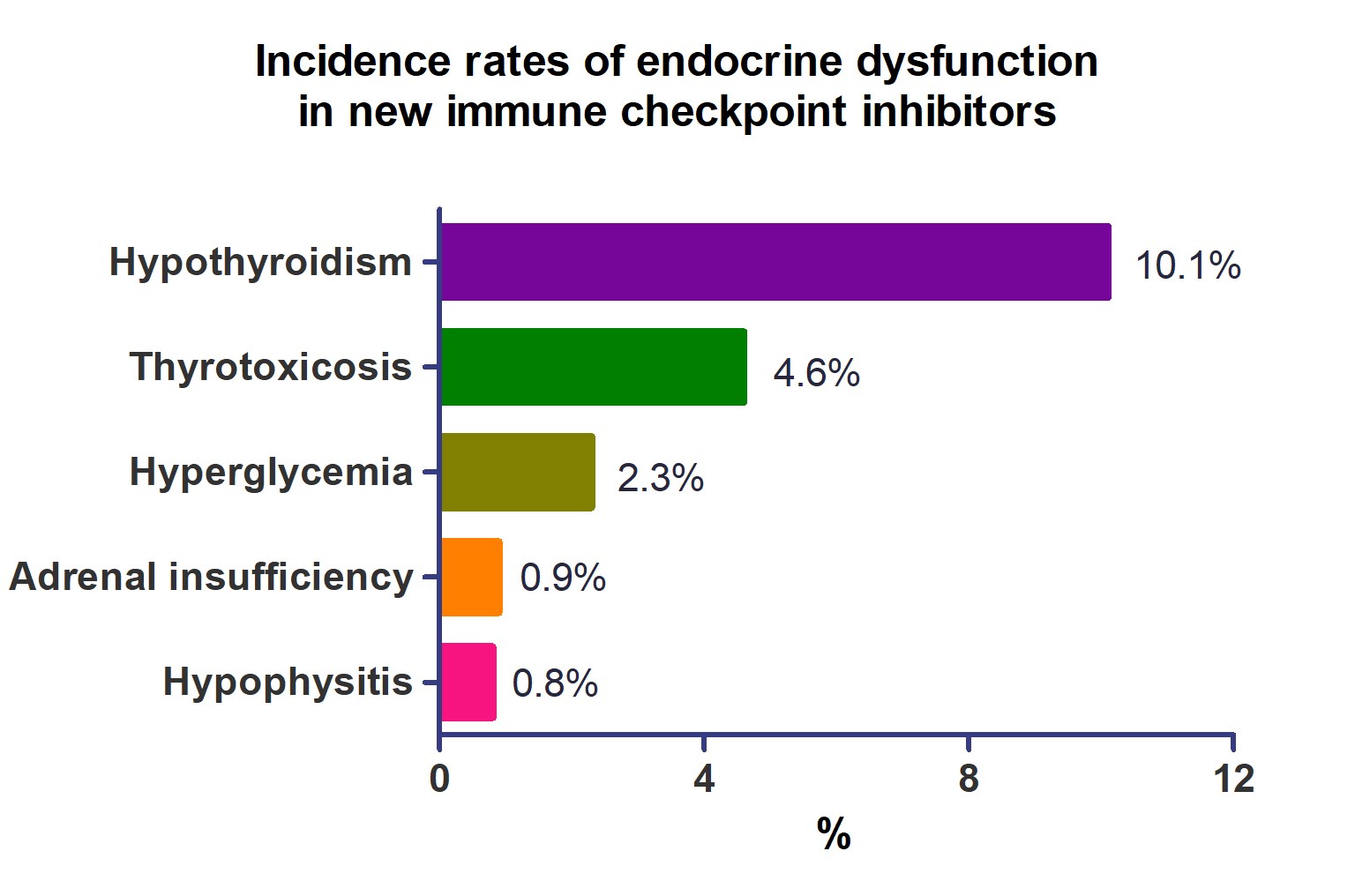
A total of 44,595 patients from 177 studies were included in this analysis. The incidence of hypothyroidism was 10.1% (95% confidence interval [CI], 8.9% to 11.4%), thyrotoxicosis was 4.6% (95% CI, 3.8% to 5.7%), hypophysitis was 0.8% (95% CI, 0.5% to 1.1%), adrenal insufficiency was 0.9% (95% CI, 0.7% to 1.1%), and hyperglycemia was 2.3% (95% CI, 1.6% to 3.4%). Hypothyroidism and thyrotoxicosis occurred most frequently with programmed cell death protein-1 (PD-1) inhibitors (13.7% and 7.5%, respectively). The rate of endocrine side effects for the combination of a programmed death-ligand 1 inhibitor (durvalumab) and cytotoxic T lymphocyte-associated antigen 4 inhibitor (tremelimumab) was higher than that of monotherapy. In a meta-analysis, the combination of tremelimumab and durvalumab had a 9- to 10-fold higher risk of pituitary and adrenal-related side effects than durvalumab alone.
Conclusion
Newly developed PD-1 inhibitors had a high incidence of thyroid-related irAEs, and combined treatment with durvalumab and tremelimumab increased the risk of pituitary- and adrenal-related irAEs. Based on these facts, it is necessary to predict the endocrine side effects corresponding to each ICI drug, diagnose and treat them appropriately, and try to reduce the morbidity and mortality of patients.

- Miscellaneous
- Clinical Characteristics, Management, and Potential Biomarkers of Endocrine Dysfunction Induced by Immune Checkpoint Inhibitors
- Shintaro Iwama, Tomoko Kobayashi, Hiroshi Arima
- Endocrinol Metab. 2021;36(2):312-321. Published online April 27, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1007
- 5,459 View
- 266 Download
- 15 Web of Science
- 14 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
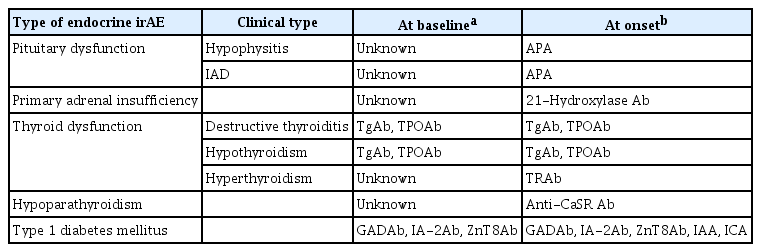
ePub - Immune-related adverse events (irAEs) affecting the endocrine glands are among the most frequent irAEs induced by immune checkpoint inhibitors (ICIs) and include hypopituitarism, primary adrenal insufficiency, thyrotoxicosis, hypothyroidism, hypoparathyroidism, and type 1 diabetes mellitus. Since the incidence and clinical features of endocrine irAEs vary according to the ICI used, it is important to understand the characteristics of these irAEs and to manage each one appropriately. Since some endocrine irAEs, including adrenal crisis and diabetic ketoacidosis, are potentially life-threatening, predicting the risk of endocrine irAEs before their onset is critical. Several autoantibodies have been detected in patients who develop endocrine irAEs, among which anti-thyroid antibodies may be predictive biomarkers of thyroid dysfunction. In this review, we describe the clinical features of each endocrine irAE induced by ICIs and discuss their potential biomarkers, including autoantibodies.
-
Citations
Citations to this article as recorded by- Clinical characteristics and potential biomarkers of thyroid and pituitary immune-related adverse events
Tomoko Kobayashi, Shintaro Iwama, Hiroshi Arima
Endocrine Journal.2024; 71(1): 23. CrossRef - A case of rapidly progressive insulin-dependent diabetes mellitus without islet autoantibodies developed over two years after the first dose of nivolumab
Kota Nishihama, Yuko Okano, Chisa Inoue, Kanako Maki, Kazuhito Eguchi, Soichiro Tanaka, Atsuro Takeshita, Mei Uemura, Taro Yasuma, Toshinari Suzuki, Esteban C. Gabazza, Yutaka Yano
Diabetology International.2024;[Epub] CrossRef - Endocrinopathies Associated With Immune Checkpoint Inhibitor Use
Anupam Kotwal, Randol Kennedy, Nupur Kikani, Sonali Thosani, Whitney Goldner, Afreen Shariff
Endocrine Practice.2024;[Epub] CrossRef - Recovery from insulin dependence in immune checkpoint inhibitor‐associated diabetes mellitus: A case report
Marie Okubo, Yuji Hataya, Kanta Fujimoto, Toshio Iwakura, Naoki Matsuoka
Journal of Diabetes Investigation.2023; 14(1): 147. CrossRef - Case Report: A Rising Cause of New-Onset Endocrinopathies After Immunotherapy
Charity Tan, Sarah Hendricks, Kristina Hernandez, Martha Benavides, Rupinderjit Samra
The Journal for Nurse Practitioners.2023; 19(5): 104582. CrossRef - Risk of Thyroid Dysfunction in PD-1 Blockade Is Stratified by the Pattern of TgAb and TPOAb Positivity at Baseline
Xin Zhou, Shintaro Iwama, Tomoko Kobayashi, Masahiko Ando, Hiroshi Arima
The Journal of Clinical Endocrinology & Metabolism.2023; 108(10): e1056. CrossRef - Severe thyrotoxicosis induced by tislelizumab: a case report and literature review
Liman Huo, Chao Wang, Haixia Ding, Xuelian Shi, Bin Shan, Ruoying Zhou, Ping Liang, Juan Hou
Frontiers in Oncology.2023;[Epub] CrossRef - Life-Threatening Endocrinological Immune-Related Adverse Events of Immune Checkpoint Inhibitor Therapy
Aleksandra Basek, Grzegorz K. Jakubiak, Grzegorz Cieślar, Agata Stanek
Cancers.2023; 15(24): 5786. CrossRef - Increased Risk of Thyroid Dysfunction by PD-1 and CTLA-4 Blockade in Patients Without Thyroid Autoantibodies at Baseline
Shintaro Iwama, Tomoko Kobayashi, Yoshinori Yasuda, Takayuki Okuji, Masaaki Ito, Masahiko Ando, Xin Zhou, Ayana Yamagami, Takeshi Onoue, Yohei Kawaguchi, Takashi Miyata, Mariko Sugiyama, Hiroshi Takagi, Daisuke Hagiwara, Hidetaka Suga, Ryoichi Banno, Tets
The Journal of Clinical Endocrinology & Metabolism.2022; 107(4): e1620. CrossRef - Biomarkers and risk factors for the early prediction of immune-related adverse events: a review
Ying Zhang, Xiaoling Zhang, Weiling Li, Yunyi Du, Wenqing Hu, Jun Zhao
Human Vaccines & Immunotherapeutics.2022;[Epub] CrossRef - Immune Checkpoint Inhibitors as a Threat to the Hypothalamus–Pituitary Axis: A Completed Puzzle
Agnese Barnabei, Andrea Corsello, Rosa Maria Paragliola, Giovanni Maria Iannantuono, Luca Falzone, Salvatore Maria Corsello, Francesco Torino
Cancers.2022; 14(4): 1057. CrossRef - Elevated TSH Level, TgAb, and Prior Use of Ramucirumab or TKIs as Risk Factors for Thyroid Dysfunction in PD-L1 Blockade
Tomoko Kobayashi, Shintaro Iwama, Ayana Yamagami, Yoshinori Yasuda, Takayuki Okuji, Masaaki Ito, Xin Zhou, Masahiko Ando, Takeshi Onoue, Takashi Miyata, Mariko Sugiyama, Daisuke Hagiwara, Hidetaka Suga, Ryoichi Banno, Tetsunari Hase, Masahiro Morise, Taka
The Journal of Clinical Endocrinology & Metabolism.2022; 107(10): e4115. CrossRef - Preconditioning of the immune system modulates the response of papillary thyroid cancer to immune checkpoint inhibitors
Fabiana Pani, Yoshinori Yasuda, Sylvie T Rousseau, Kevin C Bermea, Solmaz Roshanmehr, Rulin Wang, Srinivasan Yegnasubramanian, Patrizio Caturegli, Luigi Adamo
Journal for ImmunoTherapy of Cancer.2022; 10(12): e005538. CrossRef - Survival benefit of endocrine dysfunction following immune checkpoint inhibitors for nonthyroidal cancers
Anupam Kotwal, Mabel Ryder
Current Opinion in Endocrinology, Diabetes & Obesity.2021; 28(5): 517. CrossRef
- Clinical characteristics and potential biomarkers of thyroid and pituitary immune-related adverse events

- Adrenal gland
- Clinical Characteristics, Management, and Outcome of 22 Cases of Primary Hypophysitis
- Sun Mi Park, Ji Cheol Bae, Ji Young Joung, Yoon Young Cho, Tae Hun Kim, Sang-Man Jin, Sunghwan Suh, Kyu Yeon Hur, Kwang-Won Kim
- Endocrinol Metab. 2014;29(4):470-478. Published online December 29, 2014
- DOI: https://doi.org/10.3803/EnM.2014.29.4.470
- 4,231 View
- 41 Download
- 26 Web of Science
- 24 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Primary hypophysitis causes varying degrees of endocrine dysfunction and mass effect. The natural course and best treatment have not been well established.
Methods Medical records of 22 patients who had been diagnosed with primary hypophysitis between January 2001 and March 2013 were retrospectively reviewed. Based on the anatomical location, we classified the cases as adenohypophysitis (AH), infundibuloneurohypophysitis (INH), and panhypophysitis (PH). Clinical presentation, endocrine function, pathologic findings, magnetic resonance imaging findings, and treatment courses were reviewed.
Results Among 22 patients with primary hypophysitis, 81.8% (18/22) had involvement of the posterior pituitary lobe. Two patients of the AH (2/3, 66.6%) and three patients of the PH (3/10, 30%) groups initially underwent surgical mass reduction. Five patients, including three of the PH (3/10, 33.3%) group and one from each of the AH (1/3, 33.3%) and INH (1/9, 11.1%) groups, initially received high-dose glucocorticoid treatment. Nearly all of the patients treated with surgery or high-dose steroid treatment (9/11, 82%) required continuous hormone replacement during the follow-up period. Twelve patients received no treatment for mass reduction due to the absence of acute symptoms and signs related to a compressive mass effect. Most of them (11/12, 92%) did not show disease progression, and three patients recovered partially from hormone deficiency.
Conclusion Deficits of the posterior pituitary were the most common features in our cases of primary hypophysitis. Pituitary endocrine defects responded less favorably to glucocorticoid treatment and surgery. In the absence of symptoms related to mass effect and with the mild defect of endocrine function, it may not require treatment to reduce mass except hormone replacement.
-
Citations
Citations to this article as recorded by- Secondary xanthogranulomatous hypophysitis mimicking a pituitary macroadenoma: a case report
Salma Salhi, Ibtissem Oueslati, Yasmine Mouelhi, Alia Zehani, Nidhameddine Kchir, Elyes Kamoun, Meriem Yazidi, Melika Chihaoui
Journal of International Medical Research.2024;[Epub] CrossRef - Glucocorticoid therapy as first-line treatment in primary hypophysitis: a systematic review and individual patient data meta-analysis
Brijesh Krishnappa, Ravikumar Shah, Saba Samad Memon, Chakra Diwaker, Anurag R Lila, Virendra A Patil, Nalini S Shah, Tushar R Bandgar
Endocrine Connections.2023;[Epub] CrossRef - Hypophysitis, the Growing Spectrum of a Rare Pituitary Disease
Fabienne Langlois, Elena V Varlamov, Maria Fleseriu
The Journal of Clinical Endocrinology & Metabolism.2022; 107(1): 10. CrossRef - Outcomes of Initial Management Strategies in Patients With Autoimmune Lymphocytic Hypophysitis: A Systematic Review and Meta-analysis
Diane Donegan, Zeb Saeed, Danae A Delivanis, Mohammad Hassan Murad, Juergen Honegger, Felix Amereller, Seda Hanife Oguz, Dana Erickson, Irina Bancos
The Journal of Clinical Endocrinology & Metabolism.2022; 107(4): 1170. CrossRef - Early Pulse Glucocorticoid Therapy and Improved Hormonal Outcomes in Primary Hypophysitis
Brijesh Krishnappa, Ravikumar Shah, Vijaya Sarathi, Anurag Ranjan Lila, Manjeet Kaur Sehemby, Virendra A. Patil, Shilpa Sankhe, Nalini Shah, Tushar Bandgar
Neuroendocrinology.2022; 112(2): 186. CrossRef - Preoperative differentiation of hypophysitis and pituitary adenomas using a novel clinicoradiologic scoring system
Kyla Wright, Hyon Kim, Travis Hill, Matthew Lee, Cordelia Orillac, Nikita Mogar, Donato Pacione, Nidhi Agrawal
Pituitary.2022; 25(4): 602. CrossRef - Hypophysitis
Diane Donegan, Jürgen Honegger
Endocrine Practice.2022; 28(9): 901. CrossRef - Rare Case of a Disappearing Pituitary Adenoma During the Coronavirus Disease 2019 (COVID-19) Pandemic
David P. Bray, C. Arturo Solares, Nelson M. Oyesiku
World Neurosurgery.2021; 146: 148. CrossRef - Diabetes insipidus secondary to sellar/parasellar lesions
Anna Angelousi, Chrysoula Mytareli, Paraskevi Xekouki, Eva Kassi, Konstantinos Barkas, Ashley Grossman, Gregory Kaltsas
Journal of Neuroendocrinology.2021;[Epub] CrossRef - Clinical presentation and management of hypophysitis: An observational study of case series
Marouan Karrou, Salma Benyakhlef, Achwak Alla, Najoua Messaoudi, Asmae Oulad Amar, Siham Rouf, Imane Kamaoui, Noureddine Oulali, Faycal Moufid, Naima Abda, Hanane Latrech
Surgical Neurology International.2021; 12: 304. CrossRef - Clinical aspects of autoimmune hypothalamitis, a variant of autoimmune hypophysitis: Experience from one center
Qian Wei, Guoqing Yang, Zhaohui Lue, Jingtao Dou, Li Zang, Yijun Li, Jin Du, Weijun Gu, Yiming Mu
Journal of International Medical Research.2020; 48(3): 030006051988783. CrossRef - Primary and Ipilimumab-induced Hypophysitis: A Single-center Case Series
Paul Atkins, Ehud Ur
Endocrine Research.2020; 45(4): 246. CrossRef - Hypophysitis (Including IgG4 and Immunotherapy)
Anna Angelousi, Krystallenia Alexandraki, Marina Tsoli, Gregory Kaltsas, Eva Kassi
Neuroendocrinology.2020; 110(9-10): 822. CrossRef - Hypophysitis in the era of immune checkpoint inhibitors and immunoglobulin G4-related disease
Leen Wehbeh, Sama Alreddawi, Roberto Salvatori
Expert Review of Endocrinology & Metabolism.2019; 14(3): 167. CrossRef - Immune check point inhibitors-induced hypophysitis: a retrospective analysis of the French Pharmacovigilance database
Julie Garon-Czmil, Nadine Petitpain, Franck Rouby, Marion Sassier, Samy Babai, Mélissa Yéléhé-Okouma, Georges Weryha, Marc Klein, Pierre Gillet
Scientific Reports.2019;[Epub] CrossRef - Clinical Features, Magnetic Resonance Imaging, and Treatment Experience of 20 Patients with Lymphocytic Hypophysitis in a Single Center
Qiang Zhu, Ke Qian, Guijun Jia, Gang Lv, Jisheng Wang, Liyong Zhong, Shuqing Yu
World Neurosurgery.2019; 127: e22. CrossRef - Idiopathic granulomatous hypophysitis presenting with galactorrhea, headache, and nausea in a woman: a case report and review of the literature
Guive Sharifi, Mohammad Reza Mohajeri-Tehrani, Behrouz Navabakhsh, Bagher Larijani, Touraj Valeh
Journal of Medical Case Reports.2019;[Epub] CrossRef - Paciente de 31 años con polidipsia
A.R. Benavides Aramburu, M. Seguí Díaz
Medicina de Familia. SEMERGEN.2018; 44(2): e77. CrossRef - Primary hypophysitis and other autoimmune disorders of the sellar and suprasellar regions
Sriram Gubbi, Fady Hannah-Shmouni, Constantine A. Stratakis, Christian A. Koch
Reviews in Endocrine and Metabolic Disorders.2018; 19(4): 335. CrossRef - Primary lymphocytic hypophysitis: Clinical characteristics and treatment of 50 cases in a single centre in China over 18 years
Shuchang Wang, Linjie Wang, Yong Yao, Feng Feng, Hongbo Yang, Zhiyong Liang, Kan Deng, Hui You, Jian Sun, Bing Xing, Zimeng Jin, Renzhi Wang, Hui Pan, Huijuan Zhu
Clinical Endocrinology.2017; 87(2): 177. CrossRef - Clinical presentation and outcome of children with central diabetes insipidus associated with a self‐limited or transient pituitary stalk thickening, diagnosed as infundibuloneurohypophysitis
J. Schaefers, M. Cools, K. De Waele, I. Gies, V. Beauloye, P. Lysy, I. Francois, D. Beckers, J. De Schepper
Clinical Endocrinology.2017; 87(2): 171. CrossRef - Intrachiasmatic abscess caused by IgG4-related hypophysitis
Georgios F. Hadjigeorgiou, Eva Løbner Lund, Lars Poulsgaard, Ulla Feldt-Rasmussen, Åse Krogh Rasmussen, Marianne Wegener, Kåre Fugleholm
Acta Neurochirurgica.2017; 159(11): 2229. CrossRef - Granulomatous and lymphocytic hypophysitis – are they immunologically distinct?
Shilpa Rao, Anita Mahadevan, Tanmoy Maiti, Manish Ranjan, Shivayogi Durgad Shwetha, Arimappamagan Arivazhagan, Jitender Saini
APMIS.2016; 124(12): 1072. CrossRef - Articles in 'Endocrinology and Metabolism' in 2014
Won-Young Lee
Endocrinology and Metabolism.2015; 30(1): 47. CrossRef
- Secondary xanthogranulomatous hypophysitis mimicking a pituitary macroadenoma: a case report

- Thyroid
- Steroid Responsive Xanthomatous Hypophysitis Associated with Autoimmune Thyroiditis: A Case Report
- Ji Young Joung, Hyemin Jeong, Yoon Young Cho, Kyoungmin Huh, Yeon-Lim Suh, Kwang-Won Kim, Ji Cheol Bae
- Endocrinol Metab. 2013;28(1):65-69. Published online March 25, 2013
- DOI: https://doi.org/10.3803/EnM.2013.28.1.65
- 3,470 View
- 30 Download
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader We report the case of a 36-year-old woman who presented with headache, fever, and amenorrhea. Laboratory analysis revealed hypopituitarism and autoimmune thyroiditis, while a cerebrospinal fluid study suggested concurrent aseptic meningitis. A magnetic resonance image (MRI) scan revealed a 1.0×0.9 cm cystic mass enlarging the sella turcica. Surgical resection via an endoscopic transsphenoidal route was performed. The histological finding of the excised tissue revealed foamy histiocytes with vacuolated cytoplasm, supporting the diagnosis of xanthomatous hypophysitis. Although a residual soft lesion was observed on the MRI image postoperatively, the patient's headache and fever improved. Ten months after surgery, the patient complained of visual impairment and headache, and the residual mass had enlarged into the suprasellar area. High dose (500 mg intravenous) methylprednisolone was administered for 3 days. During the methylprednisolone pulse therapy, the patient's visual acuity and headache improved. A follow-up MRI taken after methylprednisolone therapy showed a marked mass reduction. Our case supports an autoimmune pathophysiology for xanthomatous hypophysitis and suggests that high dose glucocorticoid therapy as a treatment option.
-
Citations
Citations to this article as recorded by- Xanthomatous hypophysitis causing hypogonadotropic hypogonadism resulting in delayed presentation of slipped capital femoral epiphysis
Kirit Singh, Avinash Kumar Kanodia, Peter Ross, Antonia Torgersen, Jamie Maclean, Graham Leese, Kismet Hossain-Ibrahim
British Journal of Neurosurgery.2022; 36(2): 286. CrossRef - Full recovery from chronic headache and hypopituitarism caused by lymphocytic hypophysitis: A case report
Mao-Guang Yang, Han-Qing Cai, Si-Si Wang, Lin Liu, Chun-Mei Wang
World Journal of Clinical Cases.2022; 10(3): 1041. CrossRef - Xanthomatous Hypophysitis Secondary to a Ruptured Rathke’s Cleft Cyst: A Case Report
Emre Gezer, Burak Çabuk, Büşra Yaprak Bayrak, Zeynep Cantürk, Berrin Çetinarslan, Alev Selek, Mehmet Sözen, Damla Köksalan, Savaş Ceylan
Brain Tumor Research and Treatment.2022; 10(1): 48. CrossRef - Successful immunomodulatory treatment for recurrent xanthogranulomatous hypophysitis in an adolescent: illustrative case
Sarah DeCou, Pablo F. Recinos, Richard A. Prayson, Christopher Karakasis, Anzar Haider, Neha Patel
Journal of Neurosurgery: Case Lessons.2022;[Epub] CrossRef - Xanthogranulomatous hypophysitis: A rare presentation in a young female patient
Mohammad Ali Yaghoubi, Samira Zabihyan, Amin Saeidinia, Masoumeh Gharib, Ramin Ghiyasi Moghaddam
Clinical Case Reports.2022;[Epub] CrossRef - Xanthomatous Hypophysitis Presenting in an Adolescent Girl: A Long-Term Follow-Up of a Rare Case and Review of the Literature
Jeanne Sze Lyn Wong, Azraai Bahari Nasruddin, Nalini M. Selveindran, Kartikasalwah Abd Latif, Fauziah Kassim, Sukanya Banerjee Nair, Janet Y.H. Hong
AACE Clinical Case Reports.2021; 7(3): 220. CrossRef - Xanthomatous Hypophysitis: A Case Report and Comprehensive Literature Review
Jianyu Zhu, Zhicheng Wang, Wenze Wang, Jinghua Fan, Yi Zhang, Xiaoxu Li, Jie Liu, Shenzhong Jiang, Kan Deng, Lian Duan, Yong Yao, Huijuan Zhu
Frontiers in Endocrinology.2021;[Epub] CrossRef - Recurring Primary Xanthomatous Hypophysitis Behaving Like Pituitary Adenoma: Additional Case and Literature Review
Mansour Mathkour, Tyler Zeoli, Cassidy Werner, Tyler Scullen, Juanita Garces, Joseph Keen, Marcus Ware
World Neurosurgery.2020; 138: 27. CrossRef - Imaging findings in hypophysitis: a review
Ferdinando Caranci, Giuseppe Leone, Andrea Ponsiglione, Massimo Muto, Fabio Tortora, Mario Muto, Sossio Cirillo, Luca Brunese, Alfonso Cerase
La radiologia medica.2020; 125(3): 319. CrossRef - Hypophysitis in the era of immune checkpoint inhibitors and immunoglobulin G4-related disease
Leen Wehbeh, Sama Alreddawi, Roberto Salvatori
Expert Review of Endocrinology & Metabolism.2019; 14(3): 167. CrossRef - Xanthomatous Hypophysitis Is Associated with Ruptured Rathke’s Cleft Cyst
Kai Duan, Sylvia L. Asa, Daniel Winer, Zadeh Gelareh, Fred Gentili, Ozgur Mete
Endocrine Pathology.2017; 28(1): 83. CrossRef - Xanthomatous Hypophysitis Presenting with Diabetes Insipidus Completely Cured Through Transsphenoidal Surgery: Case Report and Literature Review
Wei Lin, Lu Gao, Xiaopeng Guo, Wenze Wang, Bing Xing
World Neurosurgery.2017; 104: 1051.e7. CrossRef - Review of xanthomatous lesions of the sella
B.K. Kleinschmidt‐DeMasters, Kevin O. Lillehei, Todd C. Hankinson
Brain Pathology.2017; 27(3): 377. CrossRef - Xanthomatous hypophysitis
Bishoy Hanna, Yan M. Li, Timothy Beutler, Parul Goyal, Walter A. Hall
Journal of Clinical Neuroscience.2015; 22(7): 1091. CrossRef - Clinical Characteristics, Management, and Outcome of 22 Cases of Primary Hypophysitis
Sun Mi Park, Ji Cheol Bae, Ji Young Joung, Yoon Young Cho, Tae Hun Kim, Sang-Man Jin, Sunghwan Suh, Kyu Yeon Hur, Kwang-Won Kim
Endocrinology and Metabolism.2014; 29(4): 470. CrossRef - Brief Review of Articles in 'Endocrinology and Metabolism' in 2013
Won-Young Lee
Endocrinology and Metabolism.2014; 29(3): 251. CrossRef
- Xanthomatous hypophysitis causing hypogonadotropic hypogonadism resulting in delayed presentation of slipped capital femoral epiphysis

- A Case of Giant Cell Granulomatous Hypophysitis with Recurrent Hypoosmolar Hyponatremia.
- Yun Hyeong Lee, Yong Bum Kim, Ju Hee Lee, Kyoung Hye Jeong, Min Kyeong Kim, Kyu Sang Song, Young Suk Jo
- Endocrinol Metab. 2010;25(4):347-353. Published online December 1, 2010
- DOI: https://doi.org/10.3803/EnM.2010.25.4.347
- 2,041 View
- 24 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - A 39-year-old woman presented with a 20 day history of recurrent hypoosmolar hyponatremia. Because her volume status seemed to be normal, the most suspected causes of her hyponatremia were adrenal insufficiency and hypothyroidism. Endocrinologic examination, including a combined pituitary function test, showed TSH and ACTH deficiency without GH deficiency, and hyperprolactinemia was also present. Sella MRI showed a pituitary mass, stalk thickening and loss of the normal neurohypophysial hyperintense signal on the T1 weighted image. Pathologic exam demonstrated granulomatous lesions and Langhans' multinucleated giant cells with inflammatory cell infiltration. After high dose methylprednisolone pulse therapy (1 g/day for 3 days) with subsequent prednisolone and levothyoxine replacement, there was no more recurrence of the hyponatremia. The sella MRI on the 6th month showed decreased mass size, narrowed stalk thickening and the reappearance of the normal neurohyphophysial hyperintense signal. She is currently in a good general condition and is receiving hormone replacement therapy.
-
Citations
Citations to this article as recorded by- Primary Granulomatous Hypophysitis Presenting with Panhypopituitarism and Central Diabetes Insipidus
Hyun Jin Oh, Ji Young Mok, Ji Eun Kim, Sung Bae Cho, Sang Ah Chang, Ji Hyun Kim, Jung Min Lee
Korean Journal of Medicine.2015; 88(5): 581. CrossRef - Idiopathic granulomatous hypophysitis: a systematic review of 82 cases in the literature
Benjamin H. M. Hunn, William G. Martin, Steven Simpson, Catriona A. Mclean
Pituitary.2014; 17(4): 357. CrossRef
- Primary Granulomatous Hypophysitis Presenting with Panhypopituitarism and Central Diabetes Insipidus

- A Case of Lymphocytic Infundibuloneurohypophysitis Along with Central Diabetes Insipidus, and this Improved with Conservative Care.
- Ji Myoung Lee, Sang Mi Park, Byung Hee Hwang, Hyun Sook Choi, Seong Su Lee, Jee Young Kim, Sung Rae Kim, Kwang Woo Lee, Ho Young Son, Sung Koo Kang, Soon Jib Yoo
- J Korean Endocr Soc. 2008;23(2):142-147. Published online April 1, 2008
- DOI: https://doi.org/10.3803/jkes.2008.23.2.142
- 1,836 View
- 21 Download
-
 Abstract
Abstract
 PDF
PDF - Idiopathic central diabetes insipidus is most likely to occur in young patients who have a clinical history of autoimmune disease. The presentation of clinical findings such as central diabetes insipidus and pituitary stalk thickening on sellar magnetic resonance imaging (MRI) in a young women would strongly suggest lymphocytic hypophysitis, which is a rare inflammatory process involving the pituitary stalk and the pituitary gland, yet this disease can sometimes regress.

- A Case of Lymphocytic Hypophysitis Presented with Hypoglycemia after Delivery.
- Jang Myung Son, Seung Hyun Ko, Yu Bae Ahn, Kang Ju, Jeong Rok Lee, Seong Eun Yang, Ki Ho Song, Ho Young Son, Jeong Su Jun
- J Korean Endocr Soc. 2003;18(3):325-331. Published online June 1, 2003
- 1,074 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - Lymphocytic hypophysitis, an inflammatory disease of the pituitary gland that is often associated with pregnancy, is caused by autoimmune destruction of the pituitary gland evidenced by diffuse inflammatory cell infiltration of the pituitary gland and some kinds of detectable autoantibodies. We report a case of lymphocytic hypophysitis in a 31-year-old woman presenting with severe hypoglycemia and hyponatremia after delivery. Hormonal study revealed panhypopituitarism and magnetic resonance imaging with enhancement showed the bulging contour of the right side pituitary gland with an ill-defined mass-like lesion and nodular thickening of the stalk. The patient's symptoms and biochemical data improved greatly with replacement of L-thyroxine and glucocorticoid. Partial recovery of panhypopituitarism was also seen. The follow-up tests revealed dramatic resolution of the pituitary lesion.

- A Case of Lymphocytic Hypophysitis in a Postmenopausal Woman.
- Sang Hyun Baik, Dong Sun Kim, Yoon Kyoung Sung, Jong Pyo Kim, Chang Beom Lee, Yong Soo Park, Woong Hwan Choi, You Hern Ahn, Tae Wha Kim, Yong Ko, Moon Hyang Park
- J Korean Endocr Soc. 2002;17(5):713-719. Published online October 1, 2002
- 1,083 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - A 64-year-old Korean woman presented with a 3-week history of severe headache and ocular pain. Her brain MRI showed a cystic pituitary mass compressing the optic chiasm. A hormonal study revealed anterior pituitary insufficiency and a slightly increased prolactin level. We performed a transsphenoidal resection of the pituitary mass. A pathological examination revealed the presence of a heavy inflammatory infiltrate, composed of lymphocytes and plasma cells, and destruction of the adenohypophysial structures. Five months after surgery, her hormonal levels had nearly normalized, without hormone replacement therapy. A follow-up MRI showed no recurrence. We conclude that lymphocytic hypophysitis should be included in the differential diagnosis of pituitary mass at any age. We discuss the features that can help to make a preoperative differential diagnosis, and selection of the appropriate treatment.

- Lymphocytic Hypophysitis associated with Pregnancy.
- Seong Jin Lee, Hyang Lim Lee, In Kyung Chung, Eun Gyung Hong, Cheol Soo Choi, Hyeon Kyu Kim, Doo Man Kim, Jae Myung Yoo, Sung Hee Ihm, Moon Gi Choi, Hyung Joon Yoo, Sung Woo Park
- J Korean Endocr Soc. 2002;17(5):705-712. Published online October 1, 2002
- 1,236 View
- 45 Download
-
 Abstract
Abstract
 PDF
PDF - Lymphocytic hypophysitis is a rare inflammatory disease of the pituitary gland that is often recognized as a cause of hypopituitarism and may be due to the autoimmune pituitary destruction that usually occurs in women in the peripartum period. We report a rare case of lymphocytic hypophysitis in a 26 year-old woman presenting with nausea and headaches for 2 months after an artificial abortion of her second pregnancy. Magnetic resonance imaging, with enhancement, showed an expanding 1.0x1.0 cm sized sellar mass. The patient underwent transsphenoidal surgery with a preoperative diagnosis of pituitary macroadenoma. A histological examination revealed diffuse lymphocytes and plasma cells infiltration which are characteristic of lymphocytic hypophysitis. Here, we present the first reported case of a pregnant woman with lymphocytic hypophysitis with a review of the literature on this increasingly recognized condition.

- Clinical and Ultrasonographic Characteristics of Malignant Thyroid Incidentalomas.
- Hahn Wook Kang, Kwang Won Kim, Byung Wan Lee, Bo Hyun Kang, Hyung Hoon Kim, Bum Jin Kim, Jae Hoon Chung, Yong Ki Min, Myung Shik Lee, Moon Kyu Lee
- J Korean Endocr Soc. 2002;17(5):649-656. Published online October 1, 2002
- 1,045 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
High-resolution ultrasonography has made the detection of asymptomatic small thyroid possible. Recent increases in the detection of incidentalomas have created a clinical dilemma on how to properly manage such incidental nodules. We investigated the prevalence, clinical and ultrasonographic characteristics, and optimal diagnostic approach toward incidentally detected benign and malignant thyroid nodules of less than 1.5 cm in size. METHODS: A retrospective review was undertaken on the 1,475 patients who had visited Samsung Medical Center, Seoul Korea between January 1999 and December 2000. The review consisted of a physical examination of the thyroid gland, thyroid function test, antithyroid antibodies, thyroid ultrasonography, fine-needle aspiration biopsy, pathology and TNM staging of the incidentally detected thyroid nodules of less than 1.5 cm in size. RESULTS: The prevalence of thyroid incidentalomas was 13.4% and the malignancy rate within them was 28.8%. There were no significant differences in age, sex, thyroid function test and size between the benign and malignant incidentalomas. Ultrasonographic characteristics showed meaningful diagnostic value for the detection of malignancy in incidentalomas. Most malignant incidentalomas were of a low stage. CONCLUSION: Occult thyroid cancers are fairly common finding. There are no clinical difference between benign and malignant thyroid nodules less than 1.5 cm ; however, ultrasonographic fingings can be used to decision of optimal management strategies.


 KES
KES

 First
First Prev
Prev



