Search
- Page Path
- HOME > Search
- Glucocorticoid-Induced Hyperglycemia: A Neglected Problem
- Jung-Hwan Cho, Sunghwan Suh
- Received February 1, 2024 Accepted February 20, 2024 Published online March 27, 2024
- DOI: https://doi.org/10.3803/EnM.2024.1951 [Epub ahead of print]
- 306 View
- 42 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Glucocorticoids provide a potent therapeutic response and are widely used to treat a variety of diseases, including coronavirus disease 2019 (COVID-19) infection. However, the issue of glucocorticoid-induced hyperglycemia (GIH), which is observed in over one-third of patients treated with glucocorticoids, is often neglected. To improve the clinical course and prognosis of diseases that necessitate glucocorticoid therapy, proper management of GIH is essential. The key pathophysiology of GIH includes systemic insulin resistance, which exacerbates hepatic steatosis and visceral obesity, as well as proteolysis and lipolysis of muscle and adipose tissue, coupled with β-cell dysfunction. For patients on glucocorticoid therapy, risk stratification should be conducted through a detailed baseline evaluation, and frequent glucose monitoring is recommended to detect the onset of GIH, particularly in high-risk individuals. Patients with confirmed GIH who require treatment should follow an insulin-centered regimen that varies depending on whether they are inpatients or outpatients, as well as the type and dosage of glucocorticoid used. The ideal strategy to maintain normoglycemia while preventing hypoglycemia is to combine basal-bolus insulin and correction doses with a continuous glucose monitoring system. This review focuses on the current understanding and latest evidence concerning GIH, incorporating insights gained from the COVID-19 pandemic.

- Diabetes, Obesity and Metabolism
- Effect of the Concomitant Use of Subcutaneous Basal Insulin and Intravenous Insulin Infusion in the Treatment of Severe Hyperglycemic Patients
- Yejee Lim, Jung Hun Ohn, Joo Jeong, Jiwon Ryu, Sun-wook Kim, Jae Ho Cho, Hee-Sun Park, Hye Won Kim, Jongchan Lee, Eun Sun Kim, Nak-Hyun Kim, You Hwan Jo, Hak Chul Jang
- Endocrinol Metab. 2022;37(3):444-454. Published online June 3, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1341
- 59,006 View
- 239 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
No consensus exists regarding the early use of subcutaneous (SC) basal insulin facilitating the transition from continuous intravenous insulin infusion (CIII) to multiple SC insulin injections in patients with severe hyperglycemia other than diabetic ketoacidosis. This study evaluated the effect of early co-administration of SC basal insulin with CIII on glucose control in patients with severe hyperglycemia.
Methods
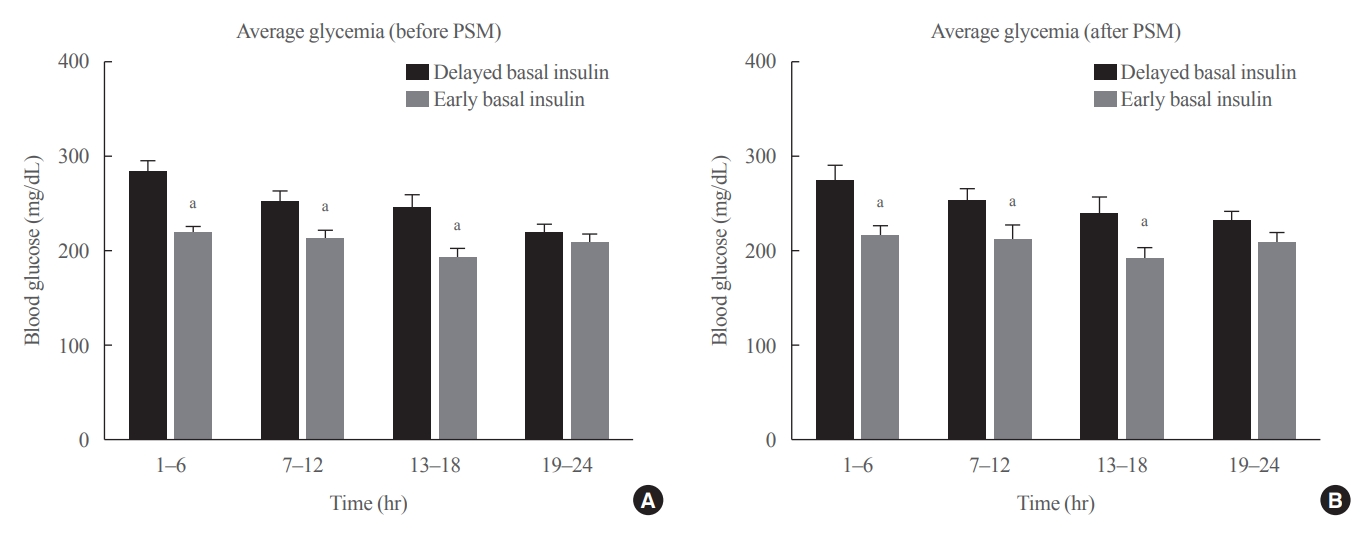
Patients who received CIII for the management of severe hyperglycemia were divided into two groups: the early basal insulin group (n=86) if they received the first SC basal insulin 0.25 U/kg body weight within 24 hours of CIII initiation and ≥4 hours before discontinuation, and the delayed basal insulin group (n=79) if they were not classified as the early basal insulin group. Rebound hyperglycemia was defined as blood glucose level of >250 mg/dL in 24 hours following CIII discontinuation. Propensity score matching (PSM) methods were additionally employed for adjusting the confounding factors (n=108).
Results
The rebound hyperglycemia incidence was significantly lower in the early basal insulin group than in the delayed basal insulin group (54.7% vs. 86.1%), despite using PSM methods (51.9%, 85.2%). The length of hospital stay was shorter in the early basal insulin group than in the delayed basal insulin group (8.5 days vs. 9.6 days, P=0.027). The hypoglycemia incidence did not differ between the groups.
Conclusion
Early co-administration of basal insulin with CIII prevents rebound hyperglycemia and shorten hospital stay without increasing the hypoglycemic events in patients with severe hyperglycemia. -
Citations
Citations to this article as recorded by- 16. Diabetes Care in the Hospital: Standards of Care in Diabetes—2024
Nuha A. ElSayed, Grazia Aleppo, Raveendhara R. Bannuru, Dennis Bruemmer, Billy S. Collins, Laya Ekhlaspour, Rodolfo J. Galindo, Marisa E. Hilliard, Eric L. Johnson, Kamlesh Khunti, Ildiko Lingvay, Glenn Matfin, Rozalina G. McCoy, Mary Lou Perry, Scott J.
Diabetes Care.2024; 47(Supplement): S295. CrossRef - 16. Diabetes Care in the Hospital: Standards of Care in Diabetes—2023
Nuha A. ElSayed, Grazia Aleppo, Vanita R. Aroda, Raveendhara R. Bannuru, Florence M. Brown, Dennis Bruemmer, Billy S. Collins, Marisa E. Hilliard, Diana Isaacs, Eric L. Johnson, Scott Kahan, Kamlesh Khunti, Jose Leon, Sarah K. Lyons, Mary Lou Perry, Priya
Diabetes Care.2023; 46(Supplement): S267. CrossRef - Effectiveness and safety of early insulin glargine administration in combination with continuous intravenous insulin infusion in the management of diabetic ketoacidosis: A randomized controlled trial
Kitti Thammakosol, Chutintorn Sriphrapradang
Diabetes, Obesity and Metabolism.2023; 25(3): 815. CrossRef
- 16. Diabetes Care in the Hospital: Standards of Care in Diabetes—2024

- Clinical Study
- Fasting and Postprandial Hyperglycemia: Their Predictors and Contributions to Overall Hyperglycemia in Korean Patients with Type 2 Diabetes
- Jaecheol Moon, Ji Young Kim, Soyeon Yoo, Gwanpyo Koh
- Endocrinol Metab. 2020;35(2):290-297. Published online June 24, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.2.290
- 6,868 View
- 201 Download
- 5 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
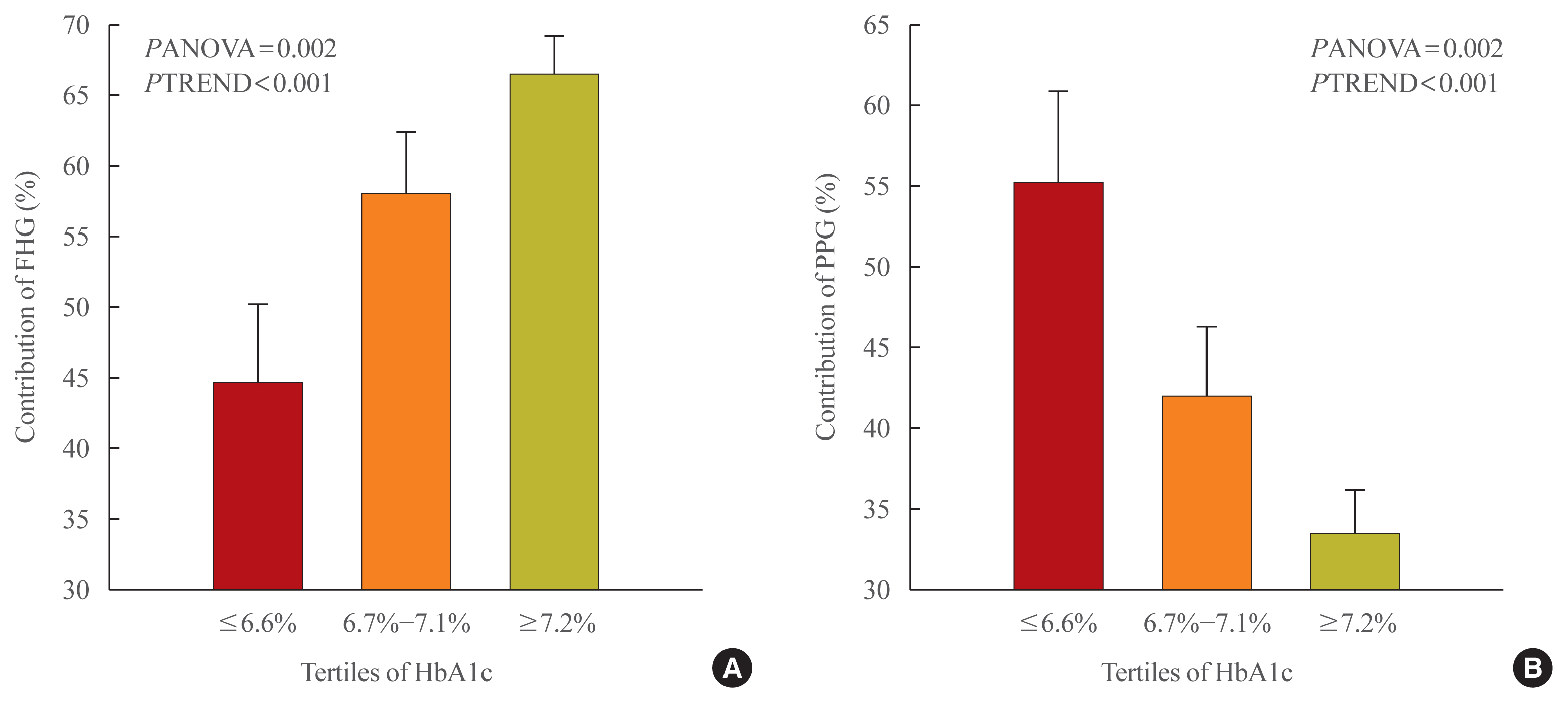
This study aimed to identify factors that affect fasting hyperglycemia (FHG) and postprandial hyperglycemia (PPG) and their contributions to overall hyperglycemia in Korean patients with type 2 diabetes mellitus (T2DM).
Methods
This was a retrospective study conducted on 194 Korean T2DM patients with 7-point self-monitoring blood glucose (SMBG) profiles plotted in 4 days in 3 consecutive months. We calculated the areas corresponding to FHG and PPG (area under the curve [AUC]FHG and AUCPPG) and contributions (%) in the graph of the 7-point SMBG data. The levels of glycated hemoglobin (HbA1c) were categorized by tertiles, and the contributions of FHG and PPG were compared.
Results
The relative contribution of FHG increased (44.7%±5.6%, 58.0%±4.4%, 66.5%±2.8%; PANOVA=0.002, PTREND <0.001), while that of PPG decreased (55.3%±5.5%, 42.0%±4.4%, 33.5%±2.8%; PANOVA=0.002, PTREND <0.001) with the elevated HbA1c. Multivariate analysis showed that HbA1c (β=0.615, P<0.001), waist circumference (β=0.216, P=0.042), and triglyceride (β=0.121, P=0.048) had a significant association with AUCFHG. Only HbA1c (β=0.231, P=0.002) and age (β=0.196, P=0.009) was significantly associated with AUCPPG.
Conclusion
The data suggested that in Korean T2DM patients, FHG predominantly contributed to overall hyperglycemia at higher HbA1c levels, whereas it contributed to PPG at lower HbA1c levels. It is recommended that certain factors, namely age, degree of glycemic control, obesity, or triglyceride levels, should be considered when prescribing medications for T2DM patients. -
Citations
Citations to this article as recorded by- Prospective study of the association between chronotype and cardiometabolic risk among Chinese young adults
Tingting Li, Yang Xie, Shuman Tao, Liwei Zou, Yajuan Yang, Fangbiao Tao, Xiaoyan Wu
BMC Public Health.2023;[Epub] CrossRef - Effects of mulberry twig alkaloids(Sangzhi alkaloids) and metformin on blood glucose fluctuations in combination with premixed insulin-treated patients with type 2 diabetes
Ziyu Meng, Chengye Xu, Haoling Liu, Xinyuan Gao, Xinyu Li, Wenjian Lin, Xuefei Ma, Changwei Yang, Ming Hao, Kangqi Zhao, Yuxin Hu, Yi Wang, Hongyu Kuang
Frontiers in Endocrinology.2023;[Epub] CrossRef - Evaluating Triglyceride and Glucose Index as a Simple and Easy-to-Calculate Marker for All-Cause and Cardiovascular Mortality
Kyung-Soo Kim, Sangmo Hong, You-Cheol Hwang, Hong-Yup Ahn, Cheol-Young Park
Journal of General Internal Medicine.2022; 37(16): 4153. CrossRef - A new approach for investigating the relative contribution of basal glucose and postprandial glucose to HbA1C
Jing Ma, Hua He, Xiaojie Yang, Dawei Chen, Cuixia Tan, Li Zhong, Qiling Du, Xiaohua Wu, Yunyi Gao, Guanjian Liu, Chun Wang, Xingwu Ran
Nutrition & Diabetes.2021;[Epub] CrossRef - The Clinical Characteristics of Gestational Diabetes Mellitus in Korea: A National Health Information Database Study
Kyung-Soo Kim, Sangmo Hong, Kyungdo Han, Cheol-Young Park
Endocrinology and Metabolism.2021; 36(3): 628. CrossRef
- Prospective study of the association between chronotype and cardiometabolic risk among Chinese young adults

- Clinical Study
- Comparison of the Efficacy and Safety of Insulin Detemir Administered Once Daily According to Two Titration Algorithms (3-0-3 and 2-4-6-8) in Patients with Type 2 Diabetes Mellitus
- Hea Min Yu, Kang Seo Park, Jun Hwa Hong, Keun Yong Park, Jong Min Lee, Bon Jeong Ku, Yeo Joo Kim, Tae Kun Oh
- Endocrinol Metab. 2020;35(1):142-148. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.142
- 4,698 View
- 80 Download
- 3 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
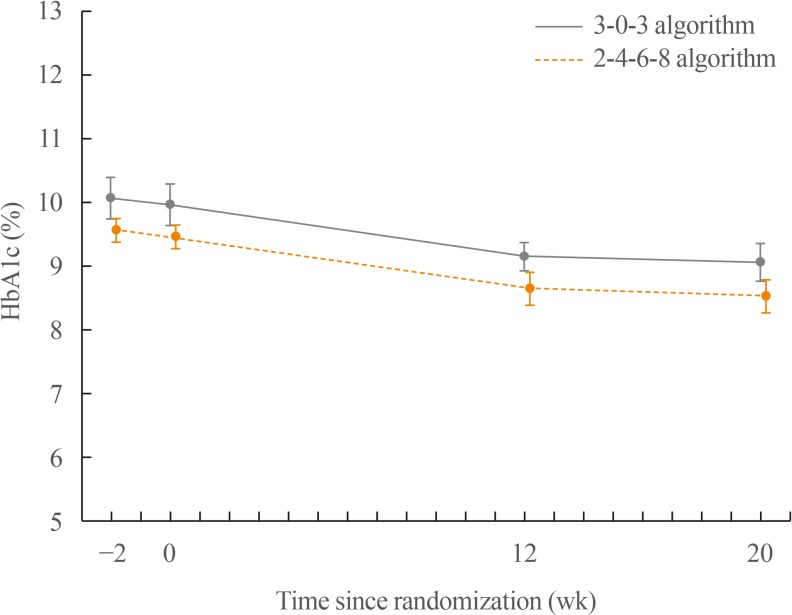
ePub Background This study was conducted to compare glycaemic control with insulin detemir administered according to two titration algorithms (3-0-3 and 2-4-6-8) after 20 weeks of treatment in subjects with type 2 diabetes mellitus inadequately controlled on metformin.
Methods This was a 20-week, randomised, multicentre, open-labelled, treat-to-target trial. Forty-six patients were randomised in a 1:1 manner to either the 3-0-3 (G3,
n =23) or 2-4-6-8 (G2,n =23) algorithm. The primary endpoint was change of haemoglobin A1c (HbA1c), and the secondary safety endpoint included hypoglycaemic events.Results After 20 weeks, HbA1c decreased similarly in the G3 and G2 groups, with a mean change of −0.9% from baseline. The mean change in fasting plasma glucose was numerically similar in both groups. The hypoglycaemia event rate per 100-patient-years of exposure (
r ) in the G2 group (r =1,427) was higher than that in the G3 group (r =807).Conclusion Both treatment groups had numerically similar HbA1c reductions. A trend towards fewer hypoglycaemia episodes after dose stabilisation was seen with the simpler G3. Clinically, this may be an important observation, as a simpler titration algorithm may support self-management and maintenance of insulin therapy.
-
Citations
Citations to this article as recorded by- Time for Using Machine Learning for Dose Guidance in Titration of People With Type 2 Diabetes? A Systematic Review of Basal Insulin Dose Guidance
Camilla Heisel Nyholm Thomsen, Stine Hangaard, Thomas Kronborg, Peter Vestergaard, Ole Hejlesen, Morten Hasselstrøm Jensen
Journal of Diabetes Science and Technology.2022; : 193229682211459. CrossRef - Efficacy and safety of patient-led versus physician-led titration of basal insulin in patients with uncontrolled type 2 diabetes: a meta-analysis of randomized controlled trials
Marco Castellana, Filippo Procino, Rodolfo Sardone, Pierpaolo Trimboli, Gianluigi Giannelli
BMJ Open Diabetes Research & Care.2020; 8(1): e001477. CrossRef
- Time for Using Machine Learning for Dose Guidance in Titration of People With Type 2 Diabetes? A Systematic Review of Basal Insulin Dose Guidance

- Clinical Study
- Favorable Glycemic Control with Once-Daily Insulin Degludec/Insulin Aspart after Changing from Basal Insulin in Adults with Type 2 Diabetes
- Han Na Jang, Ye Seul Yang, Seong Ok Lee, Tae Jung Oh, Bo Kyung Koo, Hye Seung Jung
- Endocrinol Metab. 2019;34(4):382-389. Published online December 23, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.4.382
- 4,982 View
- 143 Download
- 7 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background Conflicting results have been reported on the efficacy of insulin degludec/insulin aspart (IDegAsp) compared to basal insulin in type 2 diabetes. We investigated the effects of changing basal insulin to IDegAsp on glycemic control and sought to identify factors related to those effects.
Methods In this retrospective study of patients from three referral hospitals, patients with type 2 diabetes using basal insulin with hemoglobin A1c (HbA1c) levels less than 11.0% were enrolled. Basal insulin was replaced with IDegAsp, and data were analyzed from 3 months before to 3 months after the replacement.
Results Eighty patients were recruited (52.5% male; mean age, 67.0±9.8 years; mean duration of diabetes, 18.9±8.5 years; mean HbA1c, 8.7%±1.0%). HbA1c levels increased during 3 months of basal insulin use, but significantly decreased after changing to IDegAsp (8.28%±1.10%,
P =0.0001). The reduction was significant at 6 months in 35 patients whose longer-term data were available. Patients with a measured fasting plasma glucose (m-FPG) lower than their predicted FPG (p-FPG) by regression from HbA1c showed a significant HbA1c reduction caused by the change to IDegAsp, even without a significantly increased insulin dose. However, patients whose m-FPG was higher than their p-FPG did not experience a significant HbA1c reduction, despite a significantly increased insulin dose. Furthermore, the HbA1c reduction caused by IDegAsp was significant in patients with low fasting C-peptide levels and high insulin doses.Conclusion We observed a significant glucose-lowering effect by replacing basal insulin with IDegAsp, especially in patients with a lower m-FPG than p-FPG.
-
Citations
Citations to this article as recorded by- Evaluation of the efficiency of insulin degludec/insulin aspart therapy in controlling hyperglycemia and hypoglycemia in patients with type 2 diabetes mellitus: a real-life experience
Gökçen Güngör Semiz, İsmail Selimoğlu, Mehmet Emin Arayici, Serkan Yener, Abdurrahman Çömlekçi, Tevfik Demir
International Journal of Diabetes in Developing Countries.2023; 43(4): 544. CrossRef - Low fasting glucose‐to‐estimated average glucose ratio was associated with superior response to insulin degludec/aspart compared with basal insulin in patients with type 2 diabetes
Han Na Jang, Ye Seul Yang, Tae Jung Oh, Bo Kyung Koo, Seong Ok Lee, Kyong Soo Park, Hak Chul Jang, Hye Seung Jung
Journal of Diabetes Investigation.2022; 13(1): 85. CrossRef - Efficacy and Safety of Insulin Degludec/Insulin Aspart (IDegAsp) in Type 2 Diabetes: Systematic Review and Meta-Analysis
Brenda C Edina, Jeremy R Tandaju, Lowilius Wiyono
Cureus.2022;[Epub] CrossRef - Comparing time to intensification between insulin degludec/insulin aspart and insulin glargine: A single-center experience from India
Rajiv Kovil
Journal of Diabetology.2022; 13(2): 171. CrossRef - Efficacy and Safety of Insulin Degludec/Insulin Aspart Compared with a Conventional Premixed Insulin or Basal Insulin: A Meta-Analysis
Shinje Moon, Hye-Soo Chung, Yoon-Jung Kim, Jae-Myung Yu, Woo-Ju Jeong, Jiwon Park, Chang-Myung Oh
Metabolites.2021; 11(9): 639. CrossRef - Fear of Hypoglycemia in Adults with diabetes mellitus switching to Treatment with IDegAsp Co-formulation to Examine real-world setting: an observational study (The HATICE study)
Ulaş Serkan Topaloğlu, Hatice Kayış Topaloğlu, Melih Kızıltepe, Mesut Kılıç, Sami Bahçebaşı, Sibel Ata, Şeyma Yıldız, Yasin Şimşek
Drug Metabolism and Drug Interactions.2021; 36(2): 129. CrossRef - Response: Favorable Glycemic Control with Once-Daily Insulin Degludec/Insulin Aspart after Changing from Basal Insulin in Adults with Type 2 Diabetes (Endocrinol Metab 2019; 34:382-9, Han Na Jang et al.)
Han Na Jang, Hye Seung Jung
Endocrinology and Metabolism.2020; 35(1): 194. CrossRef - Letter: Favorable Glycemic Control with Once-Daily Insulin Degludec/Insulin Aspart after Changing from Basal Insulin in Adults with Type 2 Diabetes (Endocrinol Metab 2019; 34:382-9, Han Na Jang et al.)
Sang Youl Rhee
Endocrinology and Metabolism.2020; 35(1): 192. CrossRef - Fear of hypoglycemia in adults with diabetes mellitus switching to treatment with IDegAsp co-formulation to examine real-world setting: an observational study (The HATICE study)
Ulaş Serkan Topaloğlu, Hatice Kayış Topaloğlu, Melih Kızıltepe, Mesut Kılıç, Sami Bahçebaşı, Sibel Ata, Şeyma Yıldız, Yasin Şimşek
Drug Metabolism and Personalized Therapy.2020;[Epub] CrossRef
- Evaluation of the efficiency of insulin degludec/insulin aspart therapy in controlling hyperglycemia and hypoglycemia in patients with type 2 diabetes mellitus: a real-life experience

- Glucocorticoid-Induced Diabetes Mellitus: An Important but Overlooked Problem
- Sunghwan Suh, Mi Kyoung Park
- Endocrinol Metab. 2017;32(2):180-189. Published online May 29, 2017
- DOI: https://doi.org/10.3803/EnM.2017.32.2.180
- 15,172 View
- 588 Download
- 108 Web of Science
- 117 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Glucocorticoids are widely used as potent anti-inflammatory and immunosuppressive drugs to treat a wide range of diseases. However, they are also associated with a number of side effects, including new-onset hyperglycemia in patients without a history of diabetes mellitus (DM) or severely uncontrolled hyperglycemia in patients with known DM. Glucocorticoid-induced diabetes mellitus (GIDM) is a common and potentially harmful problem in clinical practice, affecting almost all medical specialties, but is often difficult to detect in clinical settings. However, scientific evidence is lacking regarding the effects of GIDM, as well as strategies for prevention and treatment. Similarly to nonsteroid-related DM, the principles of early detection and risk factor modification apply. Screening for GIDM should be considered in all patients treated with medium to high doses of glucocorticoids. Challenges in the management of GIDM stem from wide fluctuations in postprandial hyperglycemia and the lack of clearly defined treatment protocols. Together with lifestyle measures, hypoglycemic drugs with insulin-sensitizing effects are indicated. However, insulin therapy is often unavoidable, to the point that insulin can be considered the drug of choice. The treatment of GIDM should take into account the degree and pattern of hyperglycemia, as well as the type, dose, and schedule of glucocorticoid used. Moreover, it is essential to instruct the patient and/or the patient's family about how to perform the necessary adjustments. Prospective studies are needed to answer the remaining questions regarding GIDM.
-
Citations
Citations to this article as recorded by- COVID‐19 associated mucormycosis surge: A review on multi‐pathway mechanisms
Mohsen Pourazizi, Atousa Hakamifard, Alireza Peyman, Rasoul Mohammadi, Shakiba Dehghani, Najmeh Tavousi, Nastaran‐Sadat Hosseini, Hamed Azhdari Tehrani, Bahareh Abtahi‐Naeini
Parasite Immunology.2024;[Epub] CrossRef - Drug-induced hyperglycemia and diabetes
Marie-Anne Heurtebize, Jean-Luc Faillie
Therapies.2024; 79(2): 221. CrossRef - Immunosuppression in solid organ–transplant recipients and impact on nutrition support
Nicole K. Wilson, Ann D. Kataria
Nutrition in Clinical Practice.2024; 39(1): 109. CrossRef - The effect of different types of oral or intravenous corticosteroids on capillary blood glucose levels in hospitalized inpatients with and without diabetes
Vaishali Limbachia, Ian Nunney, Daniel J. Page, Hannah A. Barton, Leena K. Patel, Georgia N. Thomason, Stephan L. Green, Kieran F.J. Lewis, Ketan Dhatariya
Clinical Therapeutics.2024; 46(2): e59. CrossRef - Incidence and Characteristics of the Hyperosmolar Hyperglycemic State: A Danish Cohort Study
Emilie V. Rosager, Amalia Lærke K. Heltø, Cathrine U. Fox Maule, Lennart Friis-Hansen, Janne Petersen, Finn E. Nielsen, Steen B. Haugaard, Rasmus Gregersen
Diabetes Care.2024; 47(2): 272. CrossRef - Cortisol levels across the lifespan in common marmosets (Callithrix jacchus)
Matthew Lopez, Amaya Seidl, Kimberley A. Phillips
American Journal of Primatology.2024;[Epub] CrossRef - Belimumab in a Patient with Systemic Lupus Erythematosus with Juvenile Onset and Steroid-induced Diabetes: Clinical Case
Maria I. Kaleda, Irina P. Nikishina, Alesya V. Firsa
Current Pediatrics.2024; 22(6): 546. CrossRef - Optimal initial insulin dosage for managing steroid-induced hyperglycemia in hospitalized COVID-19 patients: A retrospective single-center study
Nuttavadee Ketaroonrut, Sasisopin Kiertiburanakul, Chutintorn Sriphrapradang
SAGE Open Medicine.2024;[Epub] CrossRef - Important aspects of carbohydrate metabolism disorders development in hematology/oncology patients during therapy with glucocorticosteroids: a review of the literature
N. T. Vatutin, E. V. Sklyannaya, V. V. Gribov
Oncohematology.2024; 19(2): 118. CrossRef - The safety and use of perioperative dexamethasone in the perioperative management of primary sporadic supratentorial meningiomas
Felix Arlt, Alim Emre Basaran, Markus Vogel, Martin Vychopen, Clemens Seidel, Alonso Barrantes-Freer, Erdem Güresir, Johannes Wach
Frontiers in Oncology.2024;[Epub] CrossRef - Sars-Cov2 Induced Biochemical Mechanisms in Liver Damage and Intestinal Lesions
Liudmila V. Spirina, Vladimir N. Masunov, Denis A. Dyakov, Olga E. Akbasheva, Amina Y. Kebekbayeva, Igor Yu. Shuvalov, Nadezhda V. Masunova, Irina V. Kovaleva, Yumzhana Dagbaeva
Indian Journal of Clinical Biochemistry.2023; 38(4): 437. CrossRef - Mouse Pancreatic Peptide Hormones Probed at the Sub-Single-Islet Level: The Effects of Acute Corticosterone Treatment
Aleksandra Antevska, Connor C. Long, Samuel D. Dupuy, J. Jason Collier, Michael D. Karlstad, Thanh D. Do
Journal of Proteome Research.2023; 22(1): 235. CrossRef - Type 1 and other types of diabetes mellitus in the perioperative period. What the anaesthetist should know
Robert van Wilpe, Abraham H. Hulst, Sarah.E. Siegelaar, J. Hans DeVries, Benedikt Preckel, Jeroen Hermanides
Journal of Clinical Anesthesia.2023; 84: 111012. CrossRef - Continuous Glucose Monitoring of Steroid-Induced Hyperglycemia in Patients With Dermatologic Diseases
Monika Kleinhans, Lea Jessica Albrecht, Sven Benson, Dagmar Fuhrer, Joachim Dissemond, Susanne Tan
Journal of Diabetes Science and Technology.2023; : 193229682211479. CrossRef - The Effects of Daily Prednisone and Tocilizumab on Hemoglobin A1c During the Treatment of Giant Cell Arteritis
Naomi J. Patel, Veronica Tozzo, John M. Higgins, John H. Stone
Arthritis & Rheumatology.2023; 75(4): 586. CrossRef - Characterization, evolution and risk factors of diabetes and prediabetes in a pediatric cohort of renal and liver transplant recipients
Sophie Welsch, Virginie Mailleux, Priscilla le Hardy de Beaulieu, Nadejda Ranguelov, Nathalie Godefroid, Annie Robert, Xavier Stephenne, Isabelle Scheers, Raymond Reding, Etienne M. Sokal, Philippe A. Lysy
Frontiers in Pediatrics.2023;[Epub] CrossRef - The safety of perioperative dexamethasone with antiemetic dosage in surgical patients with diabetes mellitus: a systematic review and meta-analysis
Qian-Yun Pang, Jing-Yun Wang, Xiao-Long Liang, Yan Jiang, Hong-Liang Liu
Perioperative Medicine.2023;[Epub] CrossRef - Link between Blood Cell-Associated Inflammatory Indices and Chemotherapy-Induced Hyperglycemia in Women Affected with Breast Cancer: Clinical Studies
Krishna Prasad, Suresh Rao, Sanath Kumar Hegde, Thomas George, Rhea Katherine D'souza, Sucharitha Suresh, Manjeshwar Shrinath Baliga
South Asian Journal of Cancer.2023; 12(02): 118. CrossRef - Hyperglycemia and Glycemic Variability Associated with Glucocorticoids in Women without Pre-Existing Diabetes Undergoing Neoadjuvant or Adjuvant Taxane Chemotherapy for Early-Stage Breast Cancer
Dana Mahin, Sayeh Moazami Lavasani, Leon Cristobal, Niki Tank Patel, Mina Sedrak, Daphne Stewart, James Waisman, Yuan Yuan, Wai Yu, Raynald Samoa, Nora Ruel, Susan E. Yost, Hayley Lee, Sung Hee Kil, Joanne E. Mortimer
Journal of Clinical Medicine.2023; 12(5): 1906. CrossRef - Oral mometasone furoate administration preserves anti-inflammatory action with fewer metabolic adverse effects in rats
Priscila L. Zimath, Milena S. Almeida, Maciel A. Bruxel, Alex Rafacho
Biochemical Pharmacology.2023; 210: 115486. CrossRef - Regeneration of an infected skin wound under conditions of experimental steroid hyperglycemia
L. A. Balykova, V. I. Inchina, T. V. Tarasova, D. A. Khaydar, L. M. Mosina, I. V. Saushev, A. V. Kuchuk, A. Mutvakel, I. V. Begoulov, R. S. Tarasov, P. V. Ageev, D. S. Ovchenkov
Research and Practical Medicine Journal.2023; 10(1): 90. CrossRef - Time to reposition sulfonylureas in type 2 diabetes management in Indian context: A pragmatic practical approach
Ashok Kumar Das, Banshi Saboo, Rajeev Chawla, S. R. Aravind, Rajesh Rajput, Awadhesh K. Singh, J. J. Mukherjee, Ashok Jhingan, Parag Shah, Vaishali Deshmukh, Shailaja Kale, Shalini Jaggi, G. R. Sridhar, Rajnish Dhediya, Kumar Gaurav
International Journal of Diabetes in Developing Countries.2023; 43(6): 856. CrossRef - Risk for Newly Diagnosed Type 2 Diabetes Mellitus after COVID-19 among Korean Adults: A Nationwide Matched Cohort Study
Jong Han Choi, Kyoung Min Kim, Keeho Song, Gi Hyeon Seo
Endocrinology and Metabolism.2023; 38(2): 245. CrossRef - Zein nanoparticles as oral carrier for mometasone furoate delivery
Priscila Zimath, Soraia Pinto, Sofia Dias, Alex Rafacho, Bruno Sarmento
Drug Delivery and Translational Research.2023; 13(11): 2948. CrossRef - Impact of Diabetes in COVID-19 Associated Mucormycosis and its Management:
A Non-Systematic Literature Review
Muhammed Rashid, Asha K. Rajan, Girish Thunga, Vishal Shanbhag, Sreedharan Nair
Current Diabetes Reviews.2023;[Epub] CrossRef - Adrenomedullin peptides and precursor levels in relation to haemodynamics and prognosis after heart transplantation
Abdulla Ahmed, Kriss Kania, Hebba Abdul Rahim, Salaheldin Ahmed, Göran Rådegran
ESC Heart Failure.2023; 10(4): 2427. CrossRef - Part II: Interactive case: Drug‐induced endocrine disorders
Amy C. Donihi
JACCP: JOURNAL OF THE AMERICAN COLLEGE OF CLINICAL PHARMACY.2023; 6(6): 663. CrossRef - Treating the Side Effects of Exogenous Glucocorticoids; Can We Separate the Good From the Bad?
Riccardo Pofi, Giorgio Caratti, David W Ray, Jeremy W Tomlinson
Endocrine Reviews.2023; 44(6): 975. CrossRef - Disease-modifying anti-rheumatic drugs associated with different diabetes risks in patients with rheumatoid arthritis
Yu-Jih Su, Hui-Ming Chen, Tien-Ming Chan, Tien-Tsai Cheng, Shan-Fu Yu, Jia-Feng Chen, Chun-Yu Lin, Chung-Yuan Hsu
RMD Open.2023; 9(3): e003045. CrossRef - The Prevalence of Diabetes Mellitus Type II (DMII) in the Multiple Sclerosis Population: A Systematic Review and Meta-Analysis
Vasileios Giannopapas, Lina Palaiodimou, Dimitrios Kitsos, Georgia Papagiannopoulou, Konstantina Stavrogianni, Athanasios Chasiotis, Maria Kosmidou, John S. Tzartos, George P. Paraskevas, Daphne Bakalidou, Georgios Tsivgoulis, Sotirios Giannopoulos
Journal of Clinical Medicine.2023; 12(15): 4948. CrossRef - Diabetes Mellitus Secondary to Endocrine Diseases: An Update of Diagnostic and Treatment Particularities
Mihaela Simona Popoviciu, Lorena Paduraru, Raluca Marinela Nutas, Alexandra Maria Ujoc, Galal Yahya, Kamel Metwally, Simona Cavalu
International Journal of Molecular Sciences.2023; 24(16): 12676. CrossRef - Usefulness of Indian Diabetes Risk Score in Predicting Treatment-Induced Hyperglycemia in Women Undergoing Adjuvant Chemotherapy for Breast Cancer
Krishna Prasad, Sanath Hegde, Suresh Rao, Rhea Katherine D'souza, Thomas George, Manjeshwar Shrinath Baliga, Sucharitha Suresh
South Asian Journal of Cancer.2023;[Epub] CrossRef - The inverse association between DNA gaps and HbA1c levels in type 2 diabetes mellitus
Jirapan Thongsroy, Apiwat Mutirangura
Scientific Reports.2023;[Epub] CrossRef - Corticosteroids for COVID-19: worth it or not?
Fariya Akter, Yusha Araf, Mohammad Jakir Hosen
Molecular Biology Reports.2022; 49(1): 567. CrossRef - Evidence-Based Management of Steroid-Induced Hyperglycemia in the Inpatient Setting
Lauren Longaker, Jennifer N. Clements
ADCES in Practice.2022; 10(1): 40. CrossRef - Is Methylprednisolone Acetate-Related Insulin Resistance Preventable in Cats?
Karine Marchioro Leal, Mariana Barcelos Rocha, Fernanda Venzon Varela, Luana Rodrigues, Priscila Viau Furtado, Fernanda Vieira Amorim da Costa, Álan Gomes Pöppl
Topics in Companion Animal Medicine.2022; 49: 100648. CrossRef - Ac3IV, a V1a and V1b receptor selective vasopressin analogue, protects against hydrocortisone-induced changes in pancreatic islet cell lineage
Shruti Mohan, Ryan A. Lafferty, Peter R. Flatt, R. Charlotte Moffett, Nigel Irwin
Peptides.2022; 152: 170772. CrossRef - Hospital management of hyperglycemia in the context of COVID-19: evidence-based clinical considerations
Thiago Bosco Mendes, Alexandre Barbosa Câmara-de-Souza, Bruno Halpern
Diabetology & Metabolic Syndrome.2022;[Epub] CrossRef - When therapeutic drugs lead to diabetes
Bruno Fève, André J. Scheen
Diabetologia.2022; 65(5): 751. CrossRef - Nutrition implications of intrinsic restrictive lung disease
Sylvia Rinaldi, Christine Balsillie, Cassandra Truchon, Awatif AL‐Mubarak, Marco Mura, Janet Madill
Nutrition in Clinical Practice.2022; 37(2): 239. CrossRef - Coinfection by Aspergillus and Mucoraceae Species in Two Cases of Acute Rhinosinusitis as a Complication of COVID-19
Payam Tabarsi, Somayeh Sharifynia, Mihan Pourabdollah Toutkaboni, Zahra Abtahian, Mohammad Rahdar, Arefeh Sadat Mirahmadian, Atousa Hakamifard, Simone Cesaro
Case Reports in Medicine.2022; 2022: 1. CrossRef - Case Report: Neratinib Therapy Improves Glycemic Control in a Patient With Type 2 Diabetes and Breast Cancer
Vasileios Angelis, Stephen R. D. Johnston, Amin Ardestani, Kathrin Maedler
Frontiers in Endocrinology.2022;[Epub] CrossRef - The Impact of Deranged Glucose Metabolism and Diabetes in the Pathogenesis
and Prognosis of the Novel SARS-CoV-2: A Systematic Review of Literature
Victor O. Ukwenya, Sunday A. Adelakun, Temiloluwa A. Fuwape, Ayotunde S. Adeagbo
Current Diabetes Reviews.2022;[Epub] CrossRef - Could anakinra outmatch dexamethasone/tocilizumab in COVID-19?
Rahul Gupta
Bulletin of the National Research Centre.2022;[Epub] CrossRef - Circadian clock, diurnal glucose metabolic rhythm, and dawn phenomenon
Fei Peng, Xin Li, Fang Xiao, Ruxing Zhao, Zheng Sun
Trends in Neurosciences.2022; 45(6): 471. CrossRef - 3,3′,4,5′-Tetramethoxy-trans-stilbene Improves Insulin Resistance by Activating the IRS/PI3K/Akt Pathway and Inhibiting Oxidative Stress
Yi Tan, Lingchao Miao, Jianbo Xiao, Wai San Cheang
Current Issues in Molecular Biology.2022; 44(5): 2175. CrossRef - Management of Glucocorticoid-Induced Hyperglycemia
Parag Shah, Sanjay Kalra, Yogesh Yadav, Nilakshi Deka, Tejal Lathia, Jubbin Jagan Jacob, Sunil Kumar Kota, Saptarshi Bhattacharya, Sharvil S Gadve, KAV Subramanium, Joe George, Vageesh Iyer, Sujit Chandratreya, Pankaj Kumar Aggrawal, Shailendra Kumar Sing
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2022; Volume 15: 1577. CrossRef - Effects of glucocorticoids on interstitial glucose concentrations in individuals with hematologic cancer and without known diagnosis of diabetes: a pilot study
Marcos Tadashi Kakitani Toyoshima, Priscilla Cukier, Alexandre Barbosa Câmara de Souza, Juliana Pereira, Ana Oliveira Hoff, Marcia Nery
einstein (São Paulo).2022;[Epub] CrossRef - Mucormycosis in the COVID-19 Environment: A Multifaceted Complication
Rohit Sharma, Praveen Kumar, Abdur Rauf, Ashun Chaudhary, Pradeep Kumar Prajapati, Talha Bin Emran, Clara Mariana Gonçalves Lima, Carlos Adam Conte-Junior
Frontiers in Cellular and Infection Microbiology.2022;[Epub] CrossRef - Black pepper oil (Piper nigrum L.) mitigates dexamethasone induced pancreatic damage via modulation of oxidative and nitrosative stress
Mona F. Mahmoud, Asmaa M. Elmaghraby, Noura Ali, Islam Mostafa, Assem M. El-Shazly, Mohamed A.O. Abdelfattah, Mansour Sobeh
Biomedicine & Pharmacotherapy.2022; 153: 113456. CrossRef - Various Coated Barrier Membranes for Better Guided Bone Regeneration: A Review
Ji-Youn Kim, Jun-Beom Park
Coatings.2022; 12(8): 1059. CrossRef - RETROSPECTIVE STUDY ON GLYCAEMIC CONTROL OF THE MIDDLE-AGED PATIENTS RECEIVING STEROID THERAPY IN COVID ICU
Sayantan Dutta, Sumanta Ghosh Maulik, Jisnu Nayak
PARIPEX INDIAN JOURNAL OF RESEARCH.2022; : 1. CrossRef - Risk of diabetes and the impact on preexisting diabetes in patients with lymphoma treated with steroid-containing immunochemotherapy
Joachim Baech, Marianne Tang Severinsen, Andreas K. Øvlisen, Henrik Frederiksen, Peter Vestergaard, Christian Torp-Pedersen, Judit Jørgensen, Michael Roost Clausen, Christian B. Poulsen, Peter Brown, Anne Ortved Gang, Robert Schou Pedersen, Karin Ekström
Blood Advances.2022; 6(15): 4427. CrossRef - Diabètes pharmaco-induits : quatre classes médicamenteuses au cœur de notre pratique clinique
André J. Scheen, Bruno Fève
Médecine des Maladies Métaboliques.2022; 16(7): 627. CrossRef - Dexamethasone-induced derangement in some liver function parameters: Hepatoprotective effect of L-Citrulline
Timothy Danboyi, Abdulazeez Jimoh, Evelyn Hassan-Danboyi, AbdulWahab Alhassan, AugustineBanlibo Dubo
Nigerian Journal of Experimental and Clinical Biosciences.2022; 10(3): 74. CrossRef - Polypharmacy Patterns in Multimorbid Older People with Cardiovascular Disease: Longitudinal Study
Noemí Villén, Albert Roso-Llorach, Carlos Gallego-Moll, Marc Danes-Castells, Sergio Fernández-Bertolin, Amelia Troncoso-Mariño, Monica Monteagudo, Ester Amado, Concepción Violán
Geriatrics.2022; 7(6): 141. CrossRef - Increased risk of type 2 diabetes in patients with systemic lupus erythematosus: A nationwide cohort study in Taiwan
Yeong-Jang Lin, Chih-Chiang Chien, Chung-Han Ho, Hung-An Chen, Chao-Yu Chen
Medicine.2022; 101(51): e32520. CrossRef - Synthetic Pharmacotherapy for Systemic Lupus Erythematosus: Potential Mechanisms of Action, Efficacy, and Safety
Angélica María Téllez Arévalo, Abraham Quaye, Luis Carlos Rojas-Rodríguez, Brian D. Poole, Daniela Baracaldo-Santamaría, Claudia M. Tellez Freitas
Medicina.2022; 59(1): 56. CrossRef - Effect of Ficus lacor Buch. Ham. Fruit Extract on Dexamethasone Induced Insulin Resistant Rats
V. S. Mule, N. S. Naikwade
Research Journal of Pharmacy and Technology.2022; : 5559. CrossRef - Prednisolone-induced diabetes mellitus in the cat: a historical cohort
Sivert Nerhagen, Hanne L Moberg, Gudrun S Boge, Barbara Glanemann
Journal of Feline Medicine and Surgery.2021; 23(2): 175. CrossRef - Mechanisms and Clinical Applications of Glucocorticoid Steroids in Muscular Dystrophy
Mattia Quattrocelli, Aaron S. Zelikovich, Isabella M. Salamone, Julie A. Fischer, Elizabeth M. McNally
Journal of Neuromuscular Diseases.2021; 8(1): 39. CrossRef - A practical approach to the clinical challenges in initiation of basal insulin therapy in people with type 2 diabetes
Thomas Forst, Pratik Choudhary, Doron Schneider, Bruno Linetzky, Paolo Pozzilli
Diabetes/Metabolism Research and Reviews.2021;[Epub] CrossRef - Incidence and control of steroid-induced hyperglycaemia in hospitalised patients at a tertiary care centre for lung diseases
Matej Dobravc Verbič, Jasna Gruban, Mojca Kerec Kos
Pharmacological Reports.2021; 73(3): 796. CrossRef - Epigenetics in blood–brain barrier disruption
Stephanie A. Ihezie, Iny Elizebeth Mathew, Devin W. McBride, Ari Dienel, Spiros L. Blackburn, Peeyush Kumar Thankamani Pandit
Fluids and Barriers of the CNS.2021;[Epub] CrossRef - Risk factors for corticosteroid-induced hyperglycemia requiring insulin therapy in hospitalized patients without diabetes
Catherine Li, Patricia Krause, Gretchen Stern
Endocrine.2021; 73(2): 476. CrossRef - Population pharmacodynamic modeling of intramuscular and oral dexamethasone and betamethasone effects on six biomarkers with circadian complexities in Indian women
Wojciech Krzyzanski, Mark A. Milad, Alan H. Jobe, Thomas Peppard, Robert R. Bies, William J. Jusko
Journal of Pharmacokinetics and Pharmacodynamics.2021; 48(3): 411. CrossRef - Hormonal activity in commonly used Black hair care products: evaluating hormone disruption as a plausible contribution to health disparities
Tamarra James-Todd, Lisa Connolly, Emma V. Preston, Marlee R. Quinn, Monika Plotan, Yuling Xie, Bharathi Gandi, Shruthi Mahalingaiah
Journal of Exposure Science & Environmental Epidemiology.2021; 31(3): 476. CrossRef - New‐onset diabetes in “long COVID”
Thirunavukkarasu Sathish, Mary Chandrika Anton, Tharsan Sivakumar
Journal of Diabetes.2021; 13(8): 693. CrossRef - Glucocorticoid-Induced Exacerbation of Mycobacterial Infection Is Associated With a Reduced Phagocytic Capacity of Macrophages
Yufei Xie, Jiajun Xie, Annemarie H. Meijer, Marcel J. M. Schaaf
Frontiers in Immunology.2021;[Epub] CrossRef - Glucocorticoid signaling in pancreatic islets modulates gene regulatory programs and genetic risk of type 2 diabetes
Anthony Aylward, Mei-Lin Okino, Paola Benaglio, Joshua Chiou, Elisha Beebe, Jose Andres Padilla, Sharlene Diep, Kyle J. Gaulton, Michael L. Stitzel
PLOS Genetics.2021; 17(5): e1009531. CrossRef - A Practical Guide for the Management of Steroid Induced Hyperglycaemia in the Hospital
Felix Aberer, Daniel A. Hochfellner, Harald Sourij, Julia K. Mader
Journal of Clinical Medicine.2021; 10(10): 2154. CrossRef - Combination of Bawang Dayak Extract and Acarbose against Male White Rat Glucose Levels
Aditya Maulana Perdana Putra, Ratih Pratiwi Sari, Siska Musiam
Borneo Journal of Pharmacy.2021; 4(2): 84. CrossRef - Role of Gliclazide in safely navigating type 2 diabetes mellitus patients towards euglycemia: Expert opinion from India
Subhash Wangnoo, M. Shunmugavelu, Sagili Vijaya Bhaskar Reddy, Vijay Negalur, Shreerang Godbole, Vinay K Dhandhania, Nareen Krishna, Kumar Gaurav
Endocrine and Metabolic Science.2021; 4: 100102. CrossRef - Genome-Wide Differential Methylation Profiles from Two Terpene-Rich Medicinal Plant Extracts Administered in Osteoarthritis Rats
Younhee Shin, Sathiyamoorthy Subramaniyam, Jin-Mi Chun, Ji-Hyeon Jeon, Ji-Man Hong, Hojin Jung, Boseok Seong, Chul Kim
Plants.2021; 10(6): 1132. CrossRef - Chronic glucocorticoid treatment induces hepatic lipid accumulation and hyperinsulinaemia in part through actions on AgRP neurons
Erika Harno, Charlotte Sefton, Jonathan R. Wray, Tiffany-Jayne Allen, Alison Davies, Anthony P. Coll, Anne White
Scientific Reports.2021;[Epub] CrossRef - Endocrine Disorders in Autoimmune Rheumatological Diseases: A Focus on Thyroid Autoimmune Diseases and on the Effects of Chronic Glucocorticoid Treatment
Filippo Egalini, Mirko Parasiliti Caprino, Giulia Gaggero, Vincenzo Cappiello, Jacopo Giannelli, Ruth Rossetto Giaccherino, Loredana Pagano, Roberta Giordano
Endocrines.2021; 2(3): 171. CrossRef - Current cancer therapies and their influence on glucose control
Carly Yim, Kerry Mansell, Nassrein Hussein, Terra Arnason
World Journal of Diabetes.2021; 12(7): 1010. CrossRef - Immune‐checkpoint inhibitor‐associated diabetes compared to other diabetes types ‐ A prospective, matched control study
Sascha R. Tittel, Katharina Laubner, Sebastian M. Schmid, Stefan Kress, Sigrun Merger, Wolfram Karges, Frank J. Wosch, Marcus Altmeier, Marianne Pavel, Reinhard W. Holl
Journal of Diabetes.2021; 13(12): 1007. CrossRef - Connecting the Dots: Interplay of Pathogenic Mechanisms between COVID-19 Disease and Mucormycosis
Hariprasath Prakash, Anna Skiada, Raees Ahmad Paul, Arunaloke Chakrabarti, Shivaprakash Mandya Rudramurthy
Journal of Fungi.2021; 7(8): 616. CrossRef - Antioxidant effects of L-citrulline supplementation in high-fat diet- and dexamethasone-induced Type-2 diabetes mellitus in wistar rats (Rattus norvegicus)
Evelyn Hassan-Danboyi, Abdulazeez Jimoh, Abdulwahab Alhassan, Timothy Danboyi, KabirAhmed Mohammed, AugustineBanlibo Dubo, Jamilu Haruna, BulusBilly Yakubu
Nigerian Journal of Experimental and Clinical Biosciences.2021; 9(2): 95. CrossRef - ASSESSMENT OF THE POSSIBLE CAUSES OF DIABETES MELLITUS DEVELOPED IN PATIENTS POST COVID-19 TREATMENT IN A TERTIARY CARE HOSPITAL
KHUJITH RAJUENI, RUTUJA AMBEKAR, HITENDRAPAL SOLANKI, ABDULRAHAMAN ABUBAKAR MOMIN, SUNITA PAWAR
International Journal of Pharmacy and Pharmaceutical Sciences.2021; : 11. CrossRef - Potent Anti-Inflammatory, Arylpyrazole-Based Glucocorticoid Receptor Agonists That Do Not Impair Insulin Secretion
Brandon J. Kennedy, Ashley M. Lato, Alexander R. Fisch, Susan J. Burke, Justin K. Kirkland, Carson W. Prevatte, Lee E. Dunlap, Russell T. Smith, Konstantinos D. Vogiatzis, J. Jason Collier, Shawn R. Campagna
ACS Medicinal Chemistry Letters.2021; 12(10): 1568. CrossRef - Diabetes in COVID-19 patients: challenges and possible management strategies
Riyan Al Islam Reshad, Sumaiya Hafiz Riana, Mohammad Al-baruni Chowdhury, Abu Tayab Moin, Faruque Miah, Bishajit Sarkar, Nurnabi Azad Jewel
The Egyptian Journal of Bronchology.2021;[Epub] CrossRef - Excess Body Mass—A Factor Leading to the Deterioration of COVID-19 and Its Complications—A Narrative Review
Weronika Gryczyńska, Nikita Litvinov, Bezawit Bitew, Zuzanna Bartosz, Weronika Kośmider, Paweł Bogdański, Damian Skrypnik
Viruses.2021; 13(12): 2427. CrossRef - Risk of Future Type 2 Diabetes Mellitus in Patients Developing Steroid-Induced Hyperglycemia During Hospitalization for Chronic Obstructive Pulmonary Disease Exacerbation
Jagriti Upadhyay, Nitin Trivedi, Amos Lal
Lung.2020; 198(3): 525. CrossRef - Acetylation of Hsp90 reverses dexamethasone-mediated inhibition of insulin secretion
Kecheng Zhu, Yumei Zhang, Juan Zhang, Feiye Zhou, Linlin Zhang, Shushu Wang, Qin Zhu, Qianqian Liu, Xiao Wang, Libin Zhou
Toxicology Letters.2020; 320: 19. CrossRef - Use of inhaled corticosteroids and the risk of developing type 2 diabetes in patients with chronic obstructive pulmonary disease
Mohamad Isam Saeed, Josefin Eklöf, Imane Achir, Pradeesh Sivapalan, Howraman Meteran, Anders Løkke, Tor Biering‐Sørensen, Filip Krag Knop, Jens‐Ulrik Stæhr Jensen
Diabetes, Obesity and Metabolism.2020; 22(8): 1348. CrossRef Patterns of Glucose Fluctuation are Challenging in Patients Treated for Non-Hodgkin’s Lymphoma
Andreja Marić, Tanja Miličević, Jelena Vučak Lončar, Davor Galušić, Maja Radman
International Journal of General Medicine.2020; Volume 13: 131. CrossRef- Metformin's effectiveness in preventing prednisone-induced hyperglycemia in hematological cancers
Lucy A Ochola, David G Nyamu, Eric M Guantai, Irene W Weru
Journal of Oncology Pharmacy Practice.2020; 26(4): 823. CrossRef - Study rationale and design of the EANITIATE study (EmpAgliflozin compared to NPH Insulin for sTeroId diAbeTEs) - a randomized, controlled, multicenter trial of safety and efficacy of treatment with empagliflozin compared with NPH-insulin in patients with
Carina Kirstine Klarskov, Helga Holm Schultz, Frederik Persson, Tomas Møller Christensen, Thomas Peter Almdal, Ole Snorgaard, Katrine Bagge Hansen, Ulrik Pedersen-Bjergaard, Peter Lommer Kristensen
BMC Endocrine Disorders.2020;[Epub] CrossRef - Implementation of a Weight-Based Protocol for the Management of Steroid-Induced Hyperglycemia
Alyson K. Myers, Mahmuda Khan, Sebastian Choi, Patricia Garnica, Guillaume Stoffels, Amanda Lin
American Journal of Therapeutics.2020; 27(4): e392. CrossRef - The difference between steroid diabetes mellitus and type 2 diabetes mellitus: a whole-body 18F-FDG PET/CT study
Qingqing Zhao, Jinxin Zhou, Yu Pan, Huijun Ju, Liying Zhu, Yang Liu, Yifan Zhang
Acta Diabetologica.2020; 57(11): 1383. CrossRef - Glucocorticoid dose-dependent risk of type 2 diabetes in six immune-mediated inflammatory diseases: a population-based cohort analysis
Jianhua Wu, Sarah L Mackie, Mar Pujades-Rodriguez
BMJ Open Diabetes Research & Care.2020; 8(1): e001220. CrossRef - Diabète et corticoïdes : nouveautés et aspects pratiques
M. Bastin, F. Andreelli
La Revue de Médecine Interne.2020; 41(9): 607. CrossRef - Dexamethasone in the era of COVID-19: friend or foe? An essay on the effects of dexamethasone and the potential risks of its inadvertent use in patients with diabetes
Janine Alessi, Giovana B. de Oliveira, Beatriz D. Schaan, Gabriela H. Telo
Diabetology & Metabolic Syndrome.2020;[Epub] CrossRef - Glycemic Response to Oral Dexamethasone Predicts Incident Prediabetes in Normoglycemic Subjects With Parental Diabetes
Ebenezer Nyenwe, Deirdre James, Jim Wan, Sam Dagogo-Jack
Journal of the Endocrine Society.2020;[Epub] CrossRef - Outcomes of Hospitalized Patients with Glucocorticoid-Induced Hyperglycemia—A Retrospective Analysis
Neele Delfs, Tristan Struja, Sandra Gafner, Thaddaeus Muri, Ciril Baechli, Philipp Schuetz, Beat Mueller, Claudine Angela Blum
Journal of Clinical Medicine.2020; 9(12): 4079. CrossRef - Incidence of Hyperglycemia/Secondary Diabetes in Women who have Undergone Curative Chemotherapy for Breast Cancer: First Study from India
Suresh Rao, Krishna Prasad, Soniya Abraham, Thomas George, Supreeth Kakkaje Chandran, Manjeshwar Shrinath Baliga
South Asian Journal of Cancer.2020; 09(03): 130. CrossRef - Analysis of the Potential Association of Drug-Metabolizing Enzymes CYP2C9*3 and CYP2C19*3 Gene Variations With Type 2 Diabetes: A Case-Control Study
Imadeldin Elfaki, Rashid Mir, Faisel Mohammed Abu-Duhier, Chandan Kumar Jha, Adel Ibrahim Ahmad Al-Alawy, Abdullatif Taha Babakr, Salem Abd El-Hadi Habib
Current Drug Metabolism.2020; 21(14): 1152. CrossRef - What is the optimal time for measuring glucose concentration to detect steroid-induced hyperglycemia in patients with rheumatic diseases?
Güven Barış Cansu, Döndü Üsküdar Cansu, Bengür Taşkıran, Şule Yaşar Bilge, Muzaffer Bilgin, Cengiz Korkmaz
Clinical Biochemistry.2019; 67: 33. CrossRef - Risedronate Attenuates Podocyte Injury in Phosphate Transporter-Overexpressing Rats
Yohei Asada, Takeshi Takayanagi, Tsukasa Kawakami, Eisuke Tomatsu, Atsushi Masuda, Yasumasa Yoshino, Sahoko Sekiguchi-Ueda, Megumi Shibata, Tomihiko Ide, Hajime Niimi, Eishin Yaoita, Yusuke Seino, Yoshihisa Sugimura, Atsushi Suzuki
International Journal of Endocrinology.2019; 2019: 1. CrossRef - Novel aspects of PCSK9 and lipoprotein receptors in renal disease-related dyslipidemia
Pragyi Shrestha, Bart van de Sluis, Robin P.F. Dullaart, Jacob van den Born
Cellular Signalling.2019; 55: 53. CrossRef - Understanding the burden of refractory myasthenia gravis
Christiane Schneider-Gold, Tim Hagenacker, Nico Melzer, Tobias Ruck
Therapeutic Advances in Neurological Disorders.2019; 12: 175628641983224. CrossRef - Drug-induced diabetes type 2: In silico study involving class B GPCRs
Dorota Latek, Ewelina Rutkowska, Szymon Niewieczerzal, Judyta Cielecka-Piontek, Arun Shukla
PLOS ONE.2019; 14(1): e0208892. CrossRef - Periodically repeated rituximab administrations in children with refractory nephrotic syndrome: 2-year multicenter observational study
Toshiyuki Takahashi, Takayuki Okamoto, Yasuyuki Sato, Takeshi Yamazaki, Asako Hayashi, Hayato Aoyagi, Michihiko Ueno, Norio Kobayashi, Kimiaki Uetake, Masanori Nakanishi, Tadashi Ariga
Pediatric Nephrology.2019; 34(1): 87. CrossRef - Management of hyperglycaemia in persons with non-insulin-dependent type 2 diabetes mellitus who are started on systemic glucocorticoid therapy: a systematic review
Milos Tatalovic, Roger Lehmann, Marcus Cheetham, Albina Nowak, Edouard Battegay, Silvana K Rampini
BMJ Open.2019; 9(5): e028914. CrossRef - The effect of diabetes mellitus on in-hospital hyperglycemia, length of stay and survival in patients with brain tumor receiving dexamethasone: A descriptive and comparative analysis
Panteleimon Pantelidis, Parmenion P. Tsitsopoulos, Eleni Pappa, Elpida Theologou, Nikolaos Karanikolas, Christos Drosos, Christos Tsonidis
Clinical Neurology and Neurosurgery.2019; 184: 105450. CrossRef - Impact of glucocorticoid treatment before pregnancy on glucose homeostasis of offspring exposed to glucocorticoid in adult life
Flávia Natividade da Silva, Henver Simionato Brunetta, Maciel Alencar Bruxel, Felipe Azevedo Gomes, Alex Rafacho
Life Sciences.2019; 237: 116913. CrossRef - One week of continuous corticosterone exposure impairs hepatic metabolic flexibility, promotes islet β-cell proliferation, and reduces physical activity in male C57BL/6 J mice
Susan J. Burke, Heidi M. Batdorf, Tai-Yu Huang, Joseph W. Jackson, Katarina A. Jones, Thomas M. Martin, Kristen E. Rohli, Michael D. Karlstad, Tim E. Sparer, David H. Burk, Shawn R. Campagna, Robert C. Noland, Paul L. Soto, J. Jason Collier
The Journal of Steroid Biochemistry and Molecular Biology.2019; 195: 105468. CrossRef - Effect of preadmission glucocorticoid therapy on 30-day mortality in critically ill patients: a retrospective study of a mixed ICU population in a tertiary hospital
Tak Kyu Oh, In-Ae Song, Jae Ho Lee, Cheong Lim, Young-Tae Jeon, Hee-Joon Bae, You Hwan Jo
Annals of Intensive Care.2019;[Epub] CrossRef - Hospitalization as an Opportunity to Optimize Glycemic Control in Oncology Patients
Amy Hiestand, James Flory, Ritika Chitkara
Current Diabetes Reports.2019;[Epub] CrossRef - Corticothérapie prolongée chez une personne âgée et diabète
J.L. Schlienger
Médecine des Maladies Métaboliques.2018; 12(7): 599. CrossRef - Activation of nuclear receptor PXR impairs glucose tolerance and dysregulates GLUT2 expression and subcellular localization in liver
Fatemeh Hassani-Nezhad-Gashti, Jaana Rysä, Outi Kummu, Juha Näpänkangas, Marcin Buler, Mikko Karpale, Janne Hukkanen, Jukka Hakkola
Biochemical Pharmacology.2018; 148: 253. CrossRef - Diabetes Mellitus Secondary to Cushing’s Disease
Mattia Barbot, Filippo Ceccato, Carla Scaroni
Frontiers in Endocrinology.2018;[Epub] CrossRef - MANAGEMENT OF ENDOCRINE DISEASE: Critical review of the evidence underlying management of glucocorticoid-induced hyperglycaemia
Anjana Radhakutty, Morton G Burt
European Journal of Endocrinology.2018; 179(4): R207. CrossRef - Use of parenteral glucocorticoids and the risk of new onset type 2 diabetes mellitus: A case-control study
Ala Keyany, Johannes T.H. Nielen, Patrick C. Souverein, Frank de Vries, Bart van den Bemt
Diabetes Research and Clinical Practice.2018; 139: 100. CrossRef - Dominance of the hypothalamus-pituitary-adrenal axis over the renin-angiotensin-aldosterone system is a risk factor for decreased insulin secretion
Makoto Daimon, Aya Kamba, Hiroshi Murakami, Satoru Mizushiri, Sho Osonoi, Kota Matsuki, Eri Sato, Jutaro Tanabe, Shinobu Takayasu, Yuki Matsuhashi, Miyuki Yanagimachi, Ken Terui, Kazunori Kageyama, Itoyo Tokuda, Shizuka Kurauchi, Shigeyuki Nakaji
Scientific Reports.2017;[Epub] CrossRef
- COVID‐19 associated mucormycosis surge: A review on multi‐pathway mechanisms

- Acute Hyperglycemia Associated with Anti-Cancer Medication
- Yul Hwangbo, Eun Kyung Lee
- Endocrinol Metab. 2017;32(1):23-29. Published online March 20, 2017
- DOI: https://doi.org/10.3803/EnM.2017.32.1.23
- 6,244 View
- 131 Download
- 41 Web of Science
- 43 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Hyperglycemia during chemotherapy occurs in approximately 10% to 30% of patients. Glucocorticoids and L-asparaginase are well known to cause acute hyperglycemia during chemotherapy. Long-term hyperglycemia is also frequently observed, especially in patients with hematologic malignancies treated with L-asparaginase-based regimens and total body irradiation. Glucocorticoid-induced hyperglycemia often develops because of increased insulin resistance, diminished insulin secretion, and exaggerated hepatic glucose output. Screening strategies for this condition include random glucose testing, hemoglobin A1c testing, oral glucose loading, and fasting plasma glucose screens. The management of hyperglycemia starts with insulin or sulfonylurea, depending on the type, dose, and delivery of the glucocorticoid formulation. Mammalian target of rapamycin (mTOR) inhibitors are associated with a high incidence of hyperglycemia, ranging from 13% to 50%. Immunotherapy, such as anti-programmed death 1 (PD-1) antibody treatment, induces hyperglycemia with a prevalence of 0.1%. The proposed mechanism of immunotherapy-induced hyperglycemia is an autoimmune process (insulitis). Withdrawal of the PD-1 inhibitor is the primary treatment for severe hyperglycemia. The efficacy of glucocorticoid therapy is not fully established and the decision to resume PD-1 inhibitor therapy depends on the severity of the hyperglycemia. Diabetic patients should achieve optimized glycemic control before initiating treatment, and glucose levels should be monitored periodically in patients initiating mTOR inhibitor or PD-1 inhibitor therapy. With regard to hyperglycemia caused by anti-cancer therapy, frequent monitoring and proper management are important for promoting the efficacy of anti-cancer therapy and improving patients' quality of life.
-
Citations
Citations to this article as recorded by- Bridging the Gap: Pancreas Tissue Slices From Organ and Tissue Donors for the Study of Diabetes Pathogenesis
Christian M. Cohrs, Chunguang Chen, Mark A. Atkinson, Denise M. Drotar, Stephan Speier
Diabetes.2024; 73(1): 11. CrossRef - Assessment of metabolic syndrome parameters in pediatric acute lymphoblastic leukemia survivors
Ömer Kartal, Orhan Gürsel
Indian Journal of Cancer.2023; 60(3): 325. CrossRef - Increased risk of incident diabetes after therapy with immune checkpoint inhibitor compared with conventional chemotherapy: A longitudinal trajectory analysis using a tertiary care hospital database
Minyoung Lee, Kyeongseob Jeong, Yu Rang Park, Yumie Rhee
Metabolism.2023; 138: 155311. CrossRef - Analysis of the Incidence of Type 2 Diabetes, Requirement of Insulin Treatment, and Diabetes-Related Complications among Patients with Cancer
Su Jung Lee, Chulho Kim, Hyunjae Yu, Dong-Kyu Kim
Cancers.2023; 15(4): 1094. CrossRef - A Case of Pembrolizumab-Induced Diabetic Ketoacidosis and Hyperthyroidism in a Patient With Recurrent Esophageal Adenocarcinoma
Jonathan Salangsang, Surendra Sapkota, Sanjeev Kharel, Prakash Gupta, Abhishek Kalla
Cureus.2023;[Epub] CrossRef - Link between Blood Cell-Associated Inflammatory Indices and Chemotherapy-Induced Hyperglycemia in Women Affected with Breast Cancer: Clinical Studies
Krishna Prasad, Suresh Rao, Sanath Kumar Hegde, Thomas George, Rhea Katherine D'souza, Sucharitha Suresh, Manjeshwar Shrinath Baliga
South Asian Journal of Cancer.2023; 12(02): 118. CrossRef - Insulin resistance in patients with cancer: a systematic review and meta-analysis
Joan M. Màrmol, Michala Carlsson, Steffen H. Raun, Mia K. Grand, Jonas Sørensen, Louise Lang Lehrskov, Erik A. Richter, Ole Norgaard, Lykke Sylow
Acta Oncologica.2023; 62(4): 364. CrossRef - Metabolic obesity phenotypes and obesity‐related cancer risk in the National Health and Nutrition Examination Survey
Maci Winn, Prasoona Karra, Heinz Freisling, Marc J. Gunter, Benjamin Haaland, Michelle L. Litchman, Jennifer A. Doherty, Mary C. Playdon, Sheetal Hardikar
Endocrinology, Diabetes & Metabolism.2023;[Epub] CrossRef - Effects of Vitamin Intake on Blood Glucose in Cancer Patients Undergoing Chemotherapy: Quantitative and Descriptive Research
Ji Yeong Kim, Kyung Hee Lim
Korean Journal of Adult Nursing.2023; 35(2): 148. CrossRef - Oncologists’ responsibility, comfort, and knowledge managing hyperglycemia in patients with cancer undergoing chemotherapy: a cross sectional study
Teresa M. Salgado, Rotana M. Radwan, Erin Hickey Zacholski, Emily Mackler, Tonya M. Buffington, Kerri T. Musselman, William J. Irvin, Jennifer M. Perkins, Trang N. Le, Dave L. Dixon, Karen B. Farris, Vanessa B. Sheppard, Resa M. Jones
Supportive Care in Cancer.2023;[Epub] CrossRef - Diabetes management in cancer patients. An Italian Association of Medical Oncology, Italian Association of Medical Diabetologists, Italian Society of Diabetology, Italian Society of Endocrinology and Italian Society of Pharmacology multidisciplinary conse
N. Silvestris, T. Franchina, M. Gallo, A. Argentiero, A. Avogaro, G. Cirino, A. Colao, R. Danesi, G. Di Cianni, S. D’Oronzo, A. Faggiano, S. Fogli, D. Giuffrida, S. Gori, N. Marrano, R. Mazzilli, M. Monami, M. Montagnani, L. Morviducci, A. Natalicchio, A.
ESMO Open.2023; 8(6): 102062. CrossRef - Prognostic Factors for Hyperglycemia in Patients Receiving Chemotherapy
Jiyeong Kim, Kyung Hee Lim
Cancer Nursing.2023;[Epub] CrossRef - Severe Insulin Resistance in a Patient Treated With Nivolumab and Brentuximab-Vedotin for Hodgkin Lymphoma
Elif Tama, Meghan Black, Muhamad Alhaj Moustafa, Maria D Hurtado
JCEM Case Reports.2023;[Epub] CrossRef - A New Hypothesis Describing the Pathogenesis of Oral Mucosal Injury Associated with the Mammalian Target of Rapamycin (mTOR) Inhibitors
Stephen T. Sonis, Alessandro Villa
Cancers.2023; 16(1): 68. CrossRef - Management of Phosphatidylinositol-3-Kinase Inhibitor-Associated Hyperglycemia
Marcus D. Goncalves, Azeez Farooki
Integrative Cancer Therapies.2022; 21: 153473542110731. CrossRef - Metformin Induced Cognitive Impairment and Neuroinflammation in CMF-Treated Rats
Ahmad H. Alhowai, Yasser Almogbel, Ahmed A.H. Abdel, Maha A. Aldubay, Hani A. Alfheeaid, Shatha G. Felemban, Sridevi Chigurupat, Ibrahim F. Alharbi, Hindi S. Alharbi
International Journal of Pharmacology.2022; 18(2): 228. CrossRef - Glucose Influences the Response of Glioblastoma Cells to Temozolomide and Dexamethasone
Anna M Bielecka-Wajdman, Tomasz Ludyga, Daria Smyk, Wojciech Smyk, Magdalena Mularska, Patrycja Świderek, Wojciech Majewski, Christina Susanne Mullins, Michael Linnebacher, Ewa Obuchowicz
Cancer Control.2022; 29: 107327482210754. CrossRef - Cardiometabolic Comorbidities in Cancer Survivors
Leah L. Zullig, Anthony D. Sung, Michel G. Khouri, Shelley Jazowski, Nishant P. Shah, Andrea Sitlinger, Dan V. Blalock, Colette Whitney, Robin Kikuchi, Hayden B. Bosworth, Matthew J. Crowley, Karen M. Goldstein, Igor Klem, Kevin C. Oeffinger, Susan Dent
JACC: CardioOncology.2022; 4(2): 149. CrossRef - Glucose deprivation reduces proliferation and motility, and enhances the anti-proliferative effects of paclitaxel and doxorubicin in breast cell lines in vitro
Maitham A. Khajah, Sarah Khushaish, Yunus A. Luqmani, Yi-Hsien Hsieh
PLOS ONE.2022; 17(8): e0272449. CrossRef - Gemigliptin exerts protective effects against doxorubicin-induced hepatotoxicity by inhibiting apoptosis via the regulation of fibroblast growth factor 21 expression
Kyeong-Min Lee, Yeo Jin Hwang, Gwon-Soo Jung
Biochemical and Biophysical Research Communications.2022; 626: 135. CrossRef - Glucocorticoid-Induced Hyperglycemia in Oncologic Outpatients: A Narrative Review Using the Quadruple Aim Framework
Ihab Kandil, Erin Keely
Canadian Journal of Diabetes.2022; 46(7): 730. CrossRef - Real-World Experience of Monitoring Practice of Endocrinopathies Associated with the Use of Novel Targeted Therapies among Patients with Solid Tumors
Atika AlHarbi, Majed Alshamrani, Mansoor Khan, Abdelmajid Alnatsheh, Mohammed Aseeri
Medical Sciences.2022; 10(4): 65. CrossRef - The Assessment of the Hypothalamic-Pituitary-Adrenal Axis After Oncological Treatment in Pediatric Patients with Acute Lymphoblastic Leukemia
Barbara Hull, Anna Wedrychowicz, Magdalena Ossowska, Aleksandra Furtak, Joanna Badacz, Szymon Skoczeń, Jerzy B. Starzyk
Journal of Clinical Research in Pediatric Endocrinology.2022; 14(4): 393. CrossRef - Targeting Mitochondria and Oxidative Stress in Cancer- and Chemotherapy-Induced Muscle Wasting
Joshua R. Huot, Dryden Baumfalk, Aridai Resendiz, Andrea Bonetto, Ashley J. Smuder, Fabio Penna
Antioxidants & Redox Signaling.2022;[Epub] CrossRef - Onkodiabetológia III.
Róbert János Bánhegyi, Blanka Veréb, Andrea Gazdag, Beatrix Rácz, Róbert Wagner, Norbert Fülöp, Béla Pikó
Orvosi Hetilap.2022; 163(41): 1614. CrossRef - Economic burden of diabetes among medicare beneficiaries with cancer
Cassidi C McDaniel, F Ellen Loh, Devan M Rockwell, Courtney P McDonald, Chiahung Chou
Journal of Pharmaceutical Health Services Research.2021; 12(2): 142. CrossRef - The prognostic outcome of ‘type 2 diabetes mellitus and breast cancer’ association pivots on hypoxia-hyperglycemia axis
Ilhaam Ayaz Durrani, Attya Bhatti, Peter John
Cancer Cell International.2021;[Epub] CrossRef - Increased risk of diabetes in cancer survivors: a pooled analysis of 13 population-based cohort studies
Y. Xiao, H. Wang, Y. Tang, J. Yan, L. Cao, Z. Chen, Z. Shao, Z. Mei, Z. Jiang
ESMO Open.2021; 6(4): 100218. CrossRef - Sublethal concentrations of high glucose prolong mitotic arrest in a spindle assembly checkpoint activity dependent manner in budding yeast
Pinar B. Thomas, Elif E. Cavusoglu, Nur Kaluc
Biologia.2021; 76(12): 3883. CrossRef - Hyperglycemia in Childhood Acute Lymphoblastic Leukemia During Induction Chemotherapy
Nengcy Erlina Tasik Rerung, Andi Cahyadi, Nur Rochmah, Maria Christina Shanty Larasati, Mia Ratwita Andarsini, Muhammad Faizi, IDG Ugrasena, Bambang Permono
MEDICINUS.2021; 34(1): 18. CrossRef - Effect of Acute Chemotherapy on Glucose Levels in Rats
Ahmad H. Alhowail, Gena S. Alfawzan, Maha A. Aldubayan, Lolwah S. Alsalam
International Journal of Pharmacology.2020; 16(3): 276. CrossRef - Predictors of Disease Progression or Performance Status Decline in Patients Undergoing Neoadjuvant Therapy for Localized Pancreatic Head Adenocarcinoma
Alessandro Paniccia, Ana L. Gleisner, Mazen S. Zenati, Amr I. Al Abbas, Jae Pil Jung, Nathan Bahary, Kenneth K. W. Lee, David Bartlett, Melissa E. Hogg, Herbert J. Zeh, Amer H. Zureikat
Annals of Surgical Oncology.2020; 27(8): 2961. CrossRef - Fasting to enhance Cancer treatment in models: the next steps
Jing Zhang, Yanlin Deng, Bee Luan Khoo
Journal of Biomedical Science.2020;[Epub] CrossRef - Concurrent diabetic ketoacidosis and pancreatitis in Paediatric acute lymphoblastic leukemia receiving L-asparaginase
Patel Zeeshan Jameel, Sham Lohiya, Amol Dongre, Sachin Damke, Bhavana B. Lakhkar
BMC Pediatrics.2020;[Epub] CrossRef - Hyperglycemia during Adjuvant Chemotherapy as a Prognostic Factor in Breast Cancer Patients without Diabetes
Ha Rim Ahn, Sang Yull Kang, Hyun Jo Youn, Sung Hoo Jung
Journal of Breast Cancer.2020; 23(4): 398. CrossRef - Side effects of adjuvant chemotherapy and their impact on outcome in elderly breast cancer patients: a cohort study
Valentina Zanuso, Vittorio Fregoni, Lorenzo Gervaso
Future Science OA.2020; : FSO617. CrossRef - Incidence of Hyperglycemia/Secondary Diabetes in Women who have Undergone Curative Chemotherapy for Breast Cancer: First Study from India
Suresh Rao, Krishna Prasad, Soniya Abraham, Thomas George, Supreeth Kakkaje Chandran, Manjeshwar Shrinath Baliga
South Asian Journal of Cancer.2020; 09(03): 130. CrossRef - Hyperglycemic ADR Distribution of Doxorubicin From VigiBase
Jincheng Yang, Jun Yang
American Journal of Therapeutics.2019; 26(3): e428. CrossRef - Hyperglycemia During Childhood Cancer Therapy: Incidence, Implications, and Impact on Outcomes
Allison Grimes, Ashraf Mohamed, Jenna Sopfe, Rachel Hill, Jane Lynch
JNCI Monographs.2019; 2019(54): 132. CrossRef - Steroid-induced diabetes in cancer patients
Gemma Dinn
Journal of Prescribing Practice.2019; 1(12): 610. CrossRef - Risk Factors for Doxorubicin-Induced Serious Hyperglycaemia-Related Adverse Drug Reactions
Jincheng Yang, Yu Wang, Kang Liu, Wen Yang, Jianying Zhang
Diabetes Therapy.2019; 10(5): 1949. CrossRef - Effect of glucose and palmitate environment on proliferation and migration of PC3‐prostate cancer cells
Lívia Prometti Rezende, Maria Raquel Unterkircher Galheigo, Breno Costa Landim, Amanda Rodrigues Cruz, Françoise Vasconcelos Botelho, Renata Graciele Zanon, Rejane Maira Góes, Daniele Lisboa Ribeiro
Cell Biology International.2019; 43(4): 373. CrossRef - Incidence of Diabetes After Cancer Development
Yul Hwangbo, Danbee Kang, Minwoong Kang, Saemina Kim, Eun Kyung Lee, Young Ae Kim, Yoon Jung Chang, Kui Son Choi, So-Youn Jung, Sang Myung Woo, Jin Seok Ahn, Sung Hoon Sim, Yun Soo Hong, Roberto Pastor-Barriuso, Eliseo Guallar, Eun Sook Lee, Sun-Young Kon
JAMA Oncology.2018; 4(8): 1099. CrossRef
- Bridging the Gap: Pancreas Tissue Slices From Organ and Tissue Donors for the Study of Diabetes Pathogenesis

- Clinical Study
- Obesity and Hyperglycemia in Korean Men with Klinefelter Syndrome: The Korean Endocrine Society Registry
- Seung Jin Han, Kyung-Soo Kim, Wonjin Kim, Jung Hee Kim, Yong-ho Lee, Ji Sun Nam, Ji A Seo, Bu Kyung Kim, Jihyun Lee, Jin Ook Chung, Min-Hee Kim, Tae-Seo Sohn, Han Seok Choi, Seong Bin Hong, Yoon-Sok Chung
- Endocrinol Metab. 2016;31(4):598-603. Published online December 20, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.4.598
- 5,275 View
- 35 Download
- 20 Web of Science
- 18 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The aim of this study was to investigate the prevalence of obesity in Korean men with Klinefelter syndrome (KS) and the associated risk factors for obesity and hyperglycemia.
Methods Data were collected retrospectively from medical records from 11 university hospitals in Korea between 1994 and 2014. Subjects aged ≥18 years with newly diagnosed KS were enrolled. The following parameters were recorded at baseline before treatment: chief complaint, height, weight, fasting glucose level, lipid panel, blood pressure, testosterone, luteinizing hormone, follicle-stimulating hormone, karyotyping patterns, and history of hypertension, diabetes, and dyslipidemia.
Results Data were analyzed from 376 of 544 initially enrolled patients. The rate of the 47 XXY chromosomal pattern was 94.1%. The prevalence of obesity (body mass index ≥25 kg/m2) in Korean men with KS was 42.6%. The testosterone level was an independent risk factor for obesity and hyperglycemia.
Conclusion Obesity is common in Korean men with KS. Hypogonadism in patients with KS was associated with obesity and hyperglycemia.
-
Citations
Citations to this article as recorded by- A dual-center study of predictive factors for sperm retrieval through microdissection testicular sperm extraction and intracytoplasmic sperm injection outcomes in men with non-mosaic Klinefelter syndrome
Jong Hyeun Baeck, Tae Jin Kim, Tae Heon Kim, Seung-Ryeol Lee, Dong Soo Park, Hwang Kwon, Ji Eun Shin, Dong Hyeon Lee, Young Dong Yu
Investigative and Clinical Urology.2023; 64(1): 41. CrossRef - Cardiorespiratory fitness in adolescents and young adults with Klinefelter syndrome – a pilot study
Julia Spiekermann, Kathrin Sinningen, Beatrice Hanusch, Michaela Kleber, Michael M. Schündeln, Cordula Kiewert, Heide Siggelkow, Jakob Höppner, Corinna Grasemann
Frontiers in Endocrinology.2023;[Epub] CrossRef - Metabolic Profile in a Cohort of Young Sicilian Patients with Klinefelter’s Syndrome: The Role of Irisin
Stefano Radellini, Valentina Guarnotta, Vincenzo Sciabica, Giuseppe Pizzolanti, Carla Giordano, Vito Angelo Giagulli
International Journal of Endocrinology.2022; 2022: 1. CrossRef - Metabolic and Nutritional Aspects in Paediatric Patients with Klinefelter Syndrome: A Narrative Review
Chiara Mameli, Giulia Fiore, Arianna Sangiorgio, Marta Agostinelli, Giulia Zichichi, Gianvincenzo Zuccotti, Elvira Verduci
Nutrients.2022; 14(10): 2107. CrossRef - Klinefelter syndrome in an adolescent with severe obesity, insulin resistance, and hyperlipidemia, successfully treated with testosterone replacement therapy
Shota Fukuhara, Jun Mori, Hisakazu Nakajima
Clinical Pediatric Endocrinology.2021; 30(3): 127. CrossRef - Glucose metabolic disorder in Klinefelter syndrome: a retrospective analysis in a single Chinese hospital and literature review
Shixuan Liu, Tao Yuan, Shuoning Song, Shi Chen, Linjie Wang, Yong Fu, Yingyue Dong, Yan Tang, Weigang Zhao
BMC Endocrine Disorders.2021;[Epub] CrossRef - What Every Internist-Endocrinologist Should Know about Rare Genetic Syndromes in Order to Prevent Needless Diagnostics, Missed Diagnoses and Medical Complications: Five Years of ‘Internal Medicine for Rare Genetic Syndromes’
Anna G. W. Rosenberg, Minke R. A. Pater, Karlijn Pellikaan, Kirsten Davidse, Anja A. Kattentidt-Mouravieva, Rogier Kersseboom, Anja G. Bos-Roubos, Agnies van Eeghen, José M. C. Veen, Jiske J. van der Meulen, Nina van Aalst-van Wieringen, Franciska M. E. H
Journal of Clinical Medicine.2021; 10(22): 5457. CrossRef - Klinefelter Syndrome and Diabetes
Mark J. O’Connor, Emma A. Snyder, Frances J. Hayes
Current Diabetes Reports.2019;[Epub] CrossRef - Endocrine aspects of Klinefelter syndrome
Adriana Herrera Lizarazo, Michelle McLoughlin, Maria G. Vogiatzi
Current Opinion in Endocrinology, Diabetes & Obesity.2019; 26(1): 60. CrossRef - Sex differences in metabolism and cardiometabolic disorders
Karthickeyan Chella Krishnan, Margarete Mehrabian, Aldons J. Lusis
Current Opinion in Lipidology.2018; 29(5): 404. CrossRef - Klinefelter Syndrome: Integrating Genetics, Neuropsychology, and Endocrinology
Claus H Gravholt, Simon Chang, Mikkel Wallentin, Jens Fedder, Philip Moore, Anne Skakkebæk
Endocrine Reviews.2018; 39(4): 389. CrossRef - Sex differences in obesity, lipid metabolism, and inflammation—A role for the sex chromosomes?
Temeka Zore, Maria Palafox, Karen Reue
Molecular Metabolism.2018; 15: 35. CrossRef - Klinefelter syndrome, insulin resistance, metabolic syndrome, and diabetes: review of literature and clinical perspectives
Andrea Salzano, Roberta D’Assante, Liam M. Heaney, Federica Monaco, Giuseppe Rengo, Pietro Valente, Daniela Pasquali, Eduardo Bossone, Daniele Gianfrilli, Andrea Lenzi, Antonio Cittadini, Alberto M. Marra, Raffaele Napoli
Endocrine.2018; 61(2): 194. CrossRef - Síndrome de Klinefelter y riesgo cardiovascular
A. Yamaguchi, P. Knoblovits
Hipertensión y Riesgo Vascular.2018; 35(4): 195. CrossRef - Articles inEndocrinology and Metabolismin 2016
Won-Young Lee
Endocrinology and Metabolism.2017; 32(1): 62. CrossRef - Sex differences in obesity: X chromosome dosage as a risk factor for increased food intake, adiposity and co-morbidities
Karen Reue
Physiology & Behavior.2017; 176: 174. CrossRef - Klinefelter Syndrome with Morbid Obesity Before Bariatric Surgery: A Case Report
Parisa Janmohammadi, Gholamreza Mohammadi-Farsani, Hana Arghavani, Mahmoud Arshad, Tayebeh Mokhber
Journal of Minimally Invasive Surgical Sciences.2017;[Epub] CrossRef - Klinefelter Syndrome and Metabolic Disorder
Ji Cheol Bae
Endocrinology and Metabolism.2016; 31(4): 535. CrossRef
- A dual-center study of predictive factors for sperm retrieval through microdissection testicular sperm extraction and intracytoplasmic sperm injection outcomes in men with non-mosaic Klinefelter syndrome

- Clinical Study
- Prognostic Factors in Patients Hospitalized with Diabetic Ketoacidosis
- Avinash Agarwal, Ambuj Yadav, Manish Gutch, Shuchi Consul, Sukriti Kumar, Ved Prakash, Anil Kumar Gupta, Annesh Bhattacharjee
- Endocrinol Metab. 2016;31(3):424-432. Published online September 1, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.3.424
- 4,704 View
- 82 Download
- 28 Web of Science
- 26 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Diabetic ketoacidosis (DKA) is characterized by a biochemical triad of hyperglycemia, acidosis, and ketonemia. This condition is life-threatening despite improvements in diabetic care. The purpose of this study was to evaluate the clinical and biochemical prognostic markers of DKA. We assessed correlations in prognostic markers with DKA-associated morbidity and mortality.
Methods Two hundred and seventy patients that were hospitalized with DKA over a period of 2 years were evaluated clinically and by laboratory tests. Serial assays of serum electrolytes, glucose, and blood pH were performed, and clinical outcome was noted as either discharged to home or death.
Results The analysis indicated that significant predictors included sex, history of type 1 diabetes mellitus or type 2 diabetes mellitus, systolic blood pressure, diastolic blood pressure, total leukocyte count, Acute Physiology and Chronic Health Evaluation II (APACHE II) score, blood urea nitrogen, serum creatinine, serum magnesium, serum phosphate, serum osmolality, serum glutamic oxaloacetic transaminases, serum glutamic pyruvic transaminases, serum albumin, which were further regressed and subjected to multivariate logistic regression (MLR) analysis. The MLR analysis indicated that males were 7.93 times more likely to have favorable outcome compared with female patients (odds ratio, 7.93; 95% confidence interval, 3.99 to 13.51), while decreases in mean APACHE II score (14.83) and serum phosphate (4.38) at presentation may lead to 2.86- and 2.71-fold better outcomes, respectively, compared with higher levels (APACHE II score, 25.00; serum phosphate, 6.04).
Conclusion Sex, baseline biochemical parameters such as APACHE II score, and phosphate level were important predictors of the DKA-associated mortality.
-
Citations
Citations to this article as recorded by- Prognosis of patients with extreme acidosis on admission to the emergency department: A retrospective cohort study
Amichai Gutgold, Shaden Salameh, Jeries Nashashibi, Yonatan Gershinsky
The American Journal of Emergency Medicine.2024; 76: 36. CrossRef - The critical role of pen needles and training in insulin delivery
Tracey Sainsbury
British Journal of Nursing.2024; 33(5): 242. CrossRef - Clinical characteristics of people with diabetic ketoacidosis at a clinic in The Gambia: a retrospective study
Orighomisan F Agboghoroma, Modou Jobe, Karen Forrest
Journal of Endocrinology, Metabolism and Diabetes of South Africa.2023; 28(1): 14. CrossRef - Elevated alanine transaminase is nonlinearly associated with in-hospital death in ICU-admitted diabetic ketoacidosis patients
Qiaoling Liu, Chen Gong, Yunjie Geng, Jiuhong You
Diabetes Research and Clinical Practice.2023; 197: 110555. CrossRef - Diabetic keto-acidosis in pancreatic diabetes – how is it different from DKA in type 1 or type 2 DM?
Sunetra Mondal, Riddhi DasGupta, Moushumi Lodh, Ashok Parida, Mandira Haldar, Arunangshu Ganguly
International Journal of Diabetes in Developing Countries.2023;[Epub] CrossRef - Comparative study of diabetic ketoacidosis in the elderly and non-elderly patients: A nine-year experience from an academic hospital in North India
Ashok Kumar Pannu, Ravindran Kiran, Abhishek Kumar, Saurabh Chandrabhan Sharda, Mandip Bhatia, Atul Saroch, Pinaki Dutta, Navneet Sharma
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(12): 102903. CrossRef - Clinical Profile and Outcome of Diabetic Ketoacidosis in Type 1 and Type 2 Diabetes: A Comparative Study
Sachin Kamle, Madhuri Holay, Prashant Patil, Parimal Tayde
Vidarbha Journal of Internal Medicine.2022; 32: 21. CrossRef - Effect of subjective tool based aerobic exercise on pulmonary functions in patients with type 2 diabetes mellitus – a feasibility RCT
M. Saini, J. Kaur
Comparative Exercise Physiology.2022; 18(3): 239. CrossRef - Clinical characteristics and outcomes of care in patients hospitalized with diabetic ketoacidosis
Mohsen S. Eledrisi, Haifaa Alkabbani, Malk Aboawon, Aya Ali, Imad Alabdulrazzak, Maab Elhaj, Ashraf Ahmed, Hazim Alqahwachi, Joanne Daghfal, Salem A. Beshyah, Rayaz A. Malik
Diabetes Research and Clinical Practice.2022; 192: 110041. CrossRef - An Audit of Factors Impacting the Time to Resolution of the Metabolic Parameters in Diabetic Ketoacidosis Patients
Muath F AlWahbi , Sami H Alharbi, Saleh A Almesned, Faisal A Alfawzan, Rayan T Alsager, Abdullah A AlHojailan, Emad A Alfadhel, Fahad G Al-Harbi
Cureus.2022;[Epub] CrossRef - Incidence of Diabetic Ketoacidosis among Adults with Type 1 Diabetes in Saudi Arabia: Systematic review
Ayoub Ali Alshaikh, Rawan Zaifallh Alsalman, Nada Hamzah Albarqi, Razan Salem Alqahtani, Ali Ahmed Almontashri, Atheer Saud Alshahrani, Mohammed Abdullah Alshehri
Pharmacophore.2022; 13(4): 105. CrossRef - Features and long‐term outcomes of patients hospitalized for diabetic ketoacidosis
Michal Michaelis, Tzippy Shochat, Ilan Shimon, Amit Akirov
Diabetes/Metabolism Research and Reviews.2021;[Epub] CrossRef - Incidence, characteristics and long-term outcomes of patients with diabetic ketoacidosis: a prospective prognosis cohort study in an emergency department
Rachel Teixeira Leal Nunes, Carolina Frade Magalhães Girardin Pimentel Mota, Paulo Ricardo Gessolo Lins, Fernanda Salles Reis, Thais Castanheira de Freitas Resende, Ludmila de Andrade Barberino, Pedro Henrique Luiz da Silva, Aecio Flavio Teixeira de Gois
Sao Paulo Medical Journal.2021; 139(1): 10. CrossRef - Management of diabetic ketoacidosis in special populations
Mohsen S. Eledrisi, Salem A. Beshyah, Rayaz A. Malik
Diabetes Research and Clinical Practice.2021; 174: 108744. CrossRef - Profile of diabetic ketoacidosis at the National Diabetes and Endocrine Center in Tripoli, Libya, 2015
Aida Elkituni, Halla Elshwekh, Nesrein M. Bendala, Wafeya S. Atwear, Fawzia A. Aldaba, Abdulmunam M. Fellah
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2021; 15(3): 771. CrossRef - Frequency of Diabetic Ketoacidosis and Its Determinants Among Pediatric Diabetes Mellitus Patients in Northwest Ethiopia
Atitegeb Abera Kidie, Ayenew Molla Lakew, Tiruneh Ayele
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2021; Volume 14: 4819. CrossRef - Diabetic ketoacidosis
Ketan K. Dhatariya, Nicole S. Glaser, Ethel Codner, Guillermo E. Umpierrez
Nature Reviews Disease Primers.2020;[Epub] CrossRef - Risk and Relevance of Insulin Pump Therapy in the Aetiology of Ketoacidosis in People with Type 1 Diabetes
Lena Christina Giessmann, Peter Herbert Kann
Experimental and Clinical Endocrinology & Diabetes.2020; 128(11): 745. CrossRef - Clinical and biochemical profile, precipitants and prognostic factors of diabetic ketoacidosis: A retrospective study from a tertiary care center of north India
Harpreet Singh, Atul Saroch, Ashok Kumar Pannu, H.J. Sachin, Navneet Sharma, Pinaki Dutta
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2019; 13(4): 2357. CrossRef - Sudden death due to diabetic ketoacidosis following power failure of an insulin pump: Autopsy and pump data
Mette Louise Blouner Gram Kjærulff, Birgitte Schmidt Astrup
Journal of Forensic and Legal Medicine.2019; 63: 34. CrossRef - Defining and characterising diabetic ketoacidosis in adults
Ketan K. Dhatariya
Diabetes Research and Clinical Practice.2019; 155: 107797. CrossRef - Effects of diabetic ketoacidosis in the respiratory system
Alice Gallo de Moraes, Salim Surani
World Journal of Diabetes.2019; 10(1): 16. CrossRef - Increasing Hospitalizations for DKA: A Need for Prevention Programs
Priyathama Vellanki, Guillermo E. Umpierrez
Diabetes Care.2018; 41(9): 1839. CrossRef - Guidelines and controversies in the management of diabetic ketoacidosis – A mini-review
Tasnim Islam, Khalid Sherani, Salim Surani, Abhay Vakil
World Journal of Diabetes.2018; 9(12): 226. CrossRef - Closing the Mortality Gap in Diabetic Ketoacidosis and Hyperosmolar Hyperglycemic State: Implications of a Clinical Decision Support App
Saperstein Y, Park J, McFarlane SI
International Journal of Clinical Endocrinology and Metabolism.2018; : 008. CrossRef - Incidence and prevalence of diabetic ketoacidosis (DKA) among adults with type 1 diabetes mellitus (T1D): a systematic literature review
Soulmaz Fazeli Farsani, Kimberly Brodovicz, Nima Soleymanlou, Jan Marquard, Erika Wissinger, Brett A Maiese
BMJ Open.2017; 7(7): e016587. CrossRef
- Prognosis of patients with extreme acidosis on admission to the emergency department: A retrospective cohort study

- Obesity and Metabolism
- Neurocognitive Changes and Their Neural Correlates in Patients with Type 2 Diabetes Mellitus
- Junghyun H Lee, Yera Choi, Chansoo Jun, Young Sun Hong, Han Byul Cho, Jieun E Kim, In Kyoon Lyoo
- Endocrinol Metab. 2014;29(2):112-121. Published online June 26, 2014
- DOI: https://doi.org/10.3803/EnM.2014.29.2.112
- 4,715 View
- 49 Download
- 34 Web of Science
- 31 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader As the prevalence and life expectancy of type 2 diabetes mellitus (T2DM) continue to increase, the importance of effective detection and intervention for the complications of T2DM, especially neurocognitive complications including cognitive dysfunction and dementia, is receiving greater attention. T2DM is thought to influence cognitive function through an as yet unclear mechanism that involves multiple factors such as hyperglycemia, hypoglycemia, and vascular disease. Recent developments in neuroimaging methods have led to the identification of potential neural correlates of T2DM-related neurocognitive changes, which extend from structural to functional and metabolite alterations in the brain. The evidence indicates various changes in the T2DM brain, including global and regional atrophy, white matter hyperintensity, altered functional connectivity, and changes in neurometabolite levels. Continued neuroimaging research is expected to further elucidate the underpinnings of cognitive decline in T2DM and allow better diagnosis and treatment of the condition.
-
Citations
Citations to this article as recorded by- The level of serum retinol-binding protein is associated with diabetic mild cognitive impairment
Wenjie Zhang, Yuqi Yuan, Xiaoxia Cui, Shihong Chen, Xianghua Zhuang
Brain Research.2024; 1822: 148670. CrossRef - Research Progress on Lipocalin-2 in Diabetic Encephalopathy
Wenjie Zhang, Shihong Chen, Xianghua Zhuang
Neuroscience.2023; 515: 74. CrossRef - Voluntary Attention and Quality of Life in Patients With Type 1 and Type 2 Diabetes Mellitus: Differences in Changes Depending on Disease Type and Duration
N. E. Tadevosyan, A. S. Khachunts, M. Gohargani, A. A. Sahakyan, A. A. Tumanyan
Journal of Evolutionary Biochemistry and Physiology.2022; 58(2): 569. CrossRef - Modifiable risk factors for neurocognitive and psychosocial problems after Hodgkin lymphoma
AnnaLynn M. Williams, Sedigheh Mirzaei Salehabadi, Mengqi Xing, Nicholas S. Phillips, Matthew J. Ehrhardt, Rebecca Howell, Yutaka Yasui, Kevin C. Oeffinger, Todd Gibson, Eric J. Chow, Wendy Leisenring, Deokumar Srivastava, Melissa M. Hudson, Leslie L. Rob
Blood.2022; 139(20): 3073. CrossRef - Type 2 Diabetes Independent of Glycemic Control is Associated With Cognitive Impairments: Findings From NHANES
Rozmin Jiwani, Brittany Dennis, Alfonso L. Neri, Chandler Bess, Sara Espinoza, Jing Wang, Monica C. Serra
Clinical Nursing Research.2022; 31(7): 1225. CrossRef - Diabetes and associated cognitive disorders: Role of the Hypothalamic-Pituitary Adrenal axis
Nathalie Marissal-Arvy, Marie-Pierre Moisan
Metabolism Open.2022; 15: 100202. CrossRef - Inside the diabetic brain: Insulin resistance and molecular mechanism associated with cognitive impairment and its possible therapeutic strategies
Bhaskar Jyoti Dutta, Shamsher Singh, Sanket Seksaria, Ghanshyam Das Gupta, Amrita Singh
Pharmacological Research.2022; 182: 106358. CrossRef - The role of LRP1 in Aβ efflux transport across the blood-brain barrier and cognitive dysfunction in diabetes mellitus
Xue P, Long Zz, Jiang Gg, Wang Lp, Bian Cm, Wang Yl, M.F. Chen, Li W
Neurochemistry International.2022; 160: 105417. CrossRef - Childhood Neurotoxicity and Brain Resilience to Adverse Events during Adulthood
AnnaLynn M. Williams, Yin Ting Cheung, Geehong Hyun, Wei Liu, Kirsten K. Ness, Matthew J. Ehrhardt, Daniel A. Mulrooney, Nickhill Bhakta, Pia Banerjee, Tara M. Brinkman, Daniel M. Green, Wassim Chemaitilly, I‐Chan Huang, Deokumar Srivastava, Melissa M. Hu
Annals of Neurology.2021; 89(3): 534. CrossRef - Metformin restores hippocampal neurogenesis and learning and memory via regulating gut microbiota in the obese mouse model
Xiaoyi Ma, Wenchang Xiao, Hao Li, Pei Pang, Feixiao Xue, Lu Wan, Lei Pei, Huanhuan Yan
Brain, Behavior, and Immunity.2021; 95: 68. CrossRef - Promoting Successful Cognitive Aging: A Ten-Year Update
Taylor J. Krivanek, Seth A. Gale, Brittany M. McFeeley, Casey M. Nicastri, Kirk R. Daffner
Journal of Alzheimer's Disease.2021; 81(3): 871. CrossRef - Association of Vitamin D Level and Nerve Conduction Study Parameters with Cognitive Function in Diabetic Neuropathy Patients
Aida Fithrie, Fasihah Irfani Fitri, Muhammad Reza Putra
Open Access Macedonian Journal of Medical Sciences.2021; 9(B): 72. CrossRef - Insulin resistance takes center stage: a new paradigm in the progression of bipolar disorder
Cynthia V. Calkin
Annals of Medicine.2019; 51(5-6): 281. CrossRef - Vitamin D Supplementation and Cognition in People with Type 2 Diabetes: A Randomized Control Trial
Mary A. Byrn, William Adams, Sue Penckofer, Mary Ann Emanuele
Journal of Diabetes Research.2019; 2019: 1. CrossRef - Neurocognitive impairment in type 2 diabetes mellitus
Marianna Karvani, P. Simos, S. Stavrakaki, D. Kapoukranidou
Hormones.2019; 18(4): 523. CrossRef - Benefits of combination low-dose pioglitazone plus fish oil on aged type 2 diabetes mice
Yuzuru Iizuka, Hyounju Kim, Satoshi Hirako, Kanako Chiba, Masahiro Wada, Akiyo Matsumoto
Journal of Food and Drug Analysis.2018; 26(4): 1265. CrossRef - Association of ApoE Genetic Polymorphism and Type 2 Diabetes with Cognition in Non-Demented Aging Chinese Adults: A Community Based Cross-Sectional Study
Jie Zhen, Tong Lin, Xiaochen Huang, Huiqiang Zhang, Shengqi Dong, Yifan Wu, Linlin Song, Rong Xiao, Linhong Yuan
Aging and disease.2018; 9(3): 346. CrossRef - Chronic Health Conditions and Neurocognitive Function in Aging Survivors of Childhood Cancer: A Report from the Childhood Cancer Survivor Study
Yin Ting Cheung, Tara M Brinkman, Chenghong Li, Yasmin Mzayek, Deokumar Srivastava, Kirsten K Ness, Sunita K Patel, Rebecca M Howell, Kevin C Oeffinger, Leslie L Robison, Gregory T Armstrong, Kevin R Krull
JNCI: Journal of the National Cancer Institute.2018; 110(4): 411. CrossRef - Diabetes, Depression, and Cognition: a Recursive Cycle of Cognitive Dysfunction and Glycemic Dysregulation
Sheila Black, Kyle Kraemer, Avani Shah, Gaynell Simpson, Forrest Scogin, Annie Smith
Current Diabetes Reports.2018;[Epub] CrossRef - Hypoglycemia is associated with dementia in elderly patients with type 2 diabetes mellitus: An analysis based on the Korea National Diabetes Program Cohort
Sang Ouk Chin, Sang Youl Rhee, Suk Chon, Sei Hyun Baik, Yongsoo Park, Moon Suk Nam, Kwan Woo Lee, Ki Hong Chun, Jeong-taek Woo, Young Seol Kim
Diabetes Research and Clinical Practice.2016; 122: 54. CrossRef - Bipolar disorders, type 2 diabetes mellitus, and the brain
Tomas Hajek, Roger McIntyre, Martin Alda
Current Opinion in Psychiatry.2016; 29(1): 1. CrossRef - 1,5-Anhydro-D-Glucitol Could Reflect Hypoglycemia Risk in Patients with Type 2 Diabetes Receiving Insulin Therapy
Min Kyeong Kim, Hye Seung Jung, Soo Heon Kwak, Young Min Cho, Kyong Soo Park, Seong Yeon Kim
Endocrinology and Metabolism.2016; 31(2): 284. CrossRef - Insulin in the nervous system and the mind: Functions in metabolism, memory, and mood
Seung-Hwan Lee, Janice M. Zabolotny, Hu Huang, Hyon Lee, Young-Bum Kim
Molecular Metabolism.2016; 5(8): 589. CrossRef - Toll-like receptor 2 and type 2 diabetes
Zahra Sepehri, Zohre Kiani, Ali Akbar Nasiri, Farhad Kohan
Cellular & Molecular Biology Letters.2016;[Epub] CrossRef - Long-term Variability in Glycemic Control Is Associated With White Matter Hyperintensities in APOE4 Genotype Carriers With Type 2 Diabetes
Abigail Livny, Ramit Ravona-Springer, Anthony Heymann, Rachel Priess, Tammar Kushnir, Galia Tsarfaty, Leeron Rabinov, Reut Moran, Hadass Hoffman, Itzik Cooper, Lior Greenbaum, Jeremy Silverman, Mary Sano, Sterling C. Johnson, Barbara B. Bendlin, Michal Sc
Diabetes Care.2016; 39(6): 1056. CrossRef - DIABETES MELLITUS Y SU ASOCIACIÓN CON DETERIORO COGNITIVO Y DEMENCIA
Gonzalo Muñoz A., Christina Degen, Johannes Schröder, Pablo Toro E.
Revista Médica Clínica Las Condes.2016; 27(2): 266. CrossRef - Blood electrolyte disturbances during severe hypoglycemia in Korean patients with type 2 diabetes
Mi Yeon Kang
The Korean Journal of Internal Medicine.2015; 30(5): 648. CrossRef - Whenever You Lose Connection, Take Intranasal Insulin?
Antje Gottschalk, Björn Ellger
Diabetes.2015; 64(3): 687. CrossRef - Spatial Patterns of Structural Brain Changes in Type 2 Diabetic Patients and Their Longitudinal Progression With Intensive Control of Blood Glucose
Guray Erus, Harsha Battapady, Tianhao Zhang, James Lovato, Michael E. Miller, Jeff D. Williamson, Lenore J. Launer, R. Nick Bryan, Christos Davatzikos
Diabetes Care.2015; 38(1): 97. CrossRef - Articles in 'Endocrinology and Metabolism' in 2014
Won-Young Lee
Endocrinology and Metabolism.2015; 30(1): 47. CrossRef - Cerebrolysin reverses hippocampal neural atrophy in a mice model of diabetes mellitus type 1
Lizzette Sanchez‐Vega, Ismael Juárez, Maria De Jesus Gomez‐Villalobos, Gonzalo Flores
Synapse.2015; 69(6): 326. CrossRef
- The level of serum retinol-binding protein is associated with diabetic mild cognitive impairment

- Visual Seizure: A Reversible Complication of Non-Ketotic Hyperglycemia.
- Na Young Kim, Min Su Park
- Endocrinol Metab. 2012;27(2):155-158. Published online June 20, 2012
- DOI: https://doi.org/10.3803/EnM.2012.27.2.155
- 18,779 View
- 23 Download
-
 Abstract
Abstract
 PDF
PDF - A 65-year-old man with diabetes mellitus was presented with left visual aura, followed by a versive seizure, each lasting approximately 3 minutes. Neurological examination showed an intermittent left homonymous hemianopsia. Brain magnetic resonance imaging (MRI) showed right occipital lobe lesion, with cytotoxic edema. Blood glucose was 593 mg/dL and serum osmolarity was 309 mOsm/kg. The seizures were controlled by normalization of blood sugar and short-term anticonvulsant, and the lesions were resolved in a follow-up MRI. We report a case of visual seizures associated with non-ketotic hyperglycemia.

- A Case of Retroperitoneal Paraganglioma Manifested as Intractable Constipation with Paralytic Ileus and Aggravated Hyperglycemia.
- Seung Joon Hwang, Mi kwang Kwon, Suk Chon
- J Korean Endocr Soc. 2008;23(6):450-455. Published online December 1, 2008
- DOI: https://doi.org/10.3803/jkes.2008.23.6.450
- 1,802 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - Paragangliomas are extra-adrenal pheochromocytomas that arise from specialized neural crest cells. They are distributed anywhere from the upper neck to the pelvic floor, and they are classified on the basis of their anatomic origin. Functioning paragangliomas can cause the same clinical manifestations as pheochromocytoma, such as hypertension, diabetes mellitus, hyperadrenergic spells and so on. We experienced a retroperitoneal paraganglioma that was found in 66 year-old male who suffered from intractable constipation, and his constipation was caused by paralytic ileus and uncontrolled hyperglycemia. After he was diagnosed, removal of the paraganglioma was done and his clinical symptoms and sustained hyperglycemia were successfully resolved.

- The Abundance and Nuclear Distribution of TonEBP in Response to Changes of Tonicity in Hyperglycemic Cells .
- Won Kun Park
- J Korean Endocr Soc. 2004;19(5):501-510. Published online October 1, 2004
- 903 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
TonEBP (Tonicity-responsive enhancer binding protein) regulates the transcription of tonicity responsive genes, such as sodium-myo-inositol and the sodium- chloride-betaine co- transporters (SMIT & BGT1), heat shock protein 70 (HSP70) and aldose reductase (AR). To characterize the signals that activate TonEBP in hyperglycemic human retinal pigment epithelial (hRPE) cells, the abundance and nuclear distribution of TonEBP were studied in response to changes of tonicity in culture media. METHODS: After the cultures reached confluence, the hRPE cells were exposed for 3 days to 25 mM glucose and 100 mM NaCl, both with and without 20 M tolrestat. The expressions of AR, SMIT and HSP 70 were determined by northern blot, and the abundances of TonEBP by western blot. The nuclear distributions of TonEBP were observed by fluorescence microscopy, after immuno staining. RESULTS: The AR and SMIT mRNA levels in hyperglycemic and hypertonic media were decreased compared to those in hypertonic media alone. These decreased AR and SMIT mRNA expressions were also observed to be significantly prevented in those cells incubated with tolrestat. Stimulation of TonEBP in hypertonic medium occurs due to a combination of an increased abundance of TonEBP and an increased distribution into the nucleus from the cytoplasm. However, the expressions and nuclear distributions of TonEBP in hyperglycemic and hypertonic media were not different from those in hypertonic media alone. CONCLUSION: The expressions of AR and SMIT genes that may influence the development of diabetic complication were down-regulated by the intracellular accumulation of sorbitol in sustained hyperglycemia. TonEBP does not play a key role in the hypertonicity-induced transcriptional regulation of AR and SMIT in hyperglycemic cells, due to the intracellular accumulation of sorbitol and depletion of myo-inositol

- Effect of Acute Hyperglycemia - and Isoproterenol - induced Hypothalamic Somatostatin Release on the Thyroid Hormone Releasing Hormone - induced Thyroid Stimulating Hormone Secretion.
- Cheol Young Park, In Myung Yang, Seung Joon Oh, Deog Yoon Kim, Jeong Taek Woo, Sung Woon Kim, Jin Woo Kim, Young Seol Kim, Young Kil Choi
- J Korean Endocr Soc. 2000;15(4-5):486-492. Published online January 1, 2001
- 1,134 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Acute hyperglycemia stimulates somatostatin (SRIH) release from the hypothalamus, and which in turn suppress growth hormone (GH) secretion and thyroid stimulating hormone (TSH) from the anterior pituitary gland. Beta-adrenergic pathway is known to stimulate the hypothalamus SRIH release. Recently, We demonstrated that isoproterenol, a beta-adrenergic agonist, had an additional suppressive effect on the suppression by glucose of GHRH-stimulated GH response. Therefore, the present study aimed to determine whether isoproterenol has an additional suppressive effect on the suppression by glucose of TRH-stimulated TSH response. METHODS: Seven healthy young men, aged 24 to 27 years, were studied. Four different TRH stimulation tests were carried out. (Test 1) TRH (Hoechst AG, Germany), 200 microgram bolus, was given intravenously at 0 minute. (Test 2) Glucose, 100 g, was given orally 30 min before TRH administration. (Test 3) Isoproterenol(Isuprel, Sanofi Winthrop, USA), 0.012 pg/kg, was infused continuously for 120 min after TRH administration. (Test 4) After pretreatment with glucose as Test 2, isoproterenol and TRH were administered as Test 3. RESULTS: Oral glucose ingestion significantly suppressed the TRH-stimulated TSH secretion. Isoproterenol infusion significantly suppressed the TRH-stimulated TSH secretion. Glucose-induced suppression of the TSH response was significantly greater than that by isoproterenol. 1soproterenol infusion after glucose pretreatment did not show any additional suppressive effect on the glucose-induced suppression of TSH response to TRH. CONCLUSION: The results suggest that isoproterenol infusion in addition to glucose pretreatment before the TRH stimulation test is not necessary for the development of stronger stimulation test for the hypothalamic somatostatin secretion.

- Effect of Isoproterenol on the Glucose-induced Hypothalamin Somatostatin Release.
- Sung Woon Kim, Jin Woo Kim, Young Seol Kim, Young Kil Choi, In Myoung Yang, Jung Taek Woo, Chul Young Park, Sun Woo Kim, Jung Hyun Ro, Sang Hwa Kim, Seung Joon Oh, Duk Yoon Kim
- J Korean Endocr Soc. 1999;14(2):255-264. Published online January 1, 2001
- 1,082 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Acute hypoglycemia stimulates somatostatin (SRIH) release from the hypothalamus, and which in turn suppress growth hormone (GH) secretion from the anterior pituitary gland. However, the exact mechanism of glucose increases the hypothalamic SRIH secretion is not well known. Beta-adrenergic pathway is known to stimulate the hypothalamus SRIH release. We, therefore, hypothesized that the glucose-induced SRIH release may be mediated by the stimulation of the central beta-adrenergic system, and investigated to determine whether a beta-adrermgic aganist, isoproterenol, contribute the suppressive effect of glucose on the GHRH-induced GH secretian. METHODS: Ten healthy young men, aged 23 to 26 years, were studied. Four endocrinological tests were carried out. (Test 1) GHRH (Bachem, CA, U.S.A.), 100pg bolus, was given intravenously at 0 minute. (Test 2) Glucose 100 gm dissolved in water, was given orally at -30 minute and GHRH was administered as Test 1. (Test 3) Isoproterenol (Isuprel, Sanofi Winthrop, USA), 0.012 mg/kg, wasinfused continuously between 0 minute and 120 minute, and GHRH was administered as Test 1. (Test 4) Isoproterenol, 0.012 mg kg was infused continuously between 0 minute and 120 minute, and glucose and GHRH were administered as Test 2. RESULTS: Oral glucose ingestion significantly suppressed the GHRH-induced GH secretion. The acute hyperglycemia significantly suppressed GHRH-induced GH secretion. The pretreatments with isoproterenol significantly suppressed the GHRH-induced GH levels. The pretreatment with glucose and isoproterenol suppressed the GHRH-induced GH levels more compared to those induced by glucose in Test 2. The GH levels in Test 4 did not significantly differ from those in Test 3. CONCLUSION: The results of this study suggests that the hypothalamic somatostatinergic activity induced by the oral glucose administeration is not mediated by the beta-adrenergic pathway in normal men. (J Kor Soc Endocrinool 14:255-264, 1999)


 KES
KES

 First
First Prev
Prev



