Search
- Page Path
- HOME > Search
- Diabetes, obesity and metabolism
- Initial Combination Therapy in Type 2 Diabetes
- Ji Yoon Kim, Nam Hoon Kim
- Endocrinol Metab. 2024;39(1):23-32. Published online November 30, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1816
- 1,910 View
- 227 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
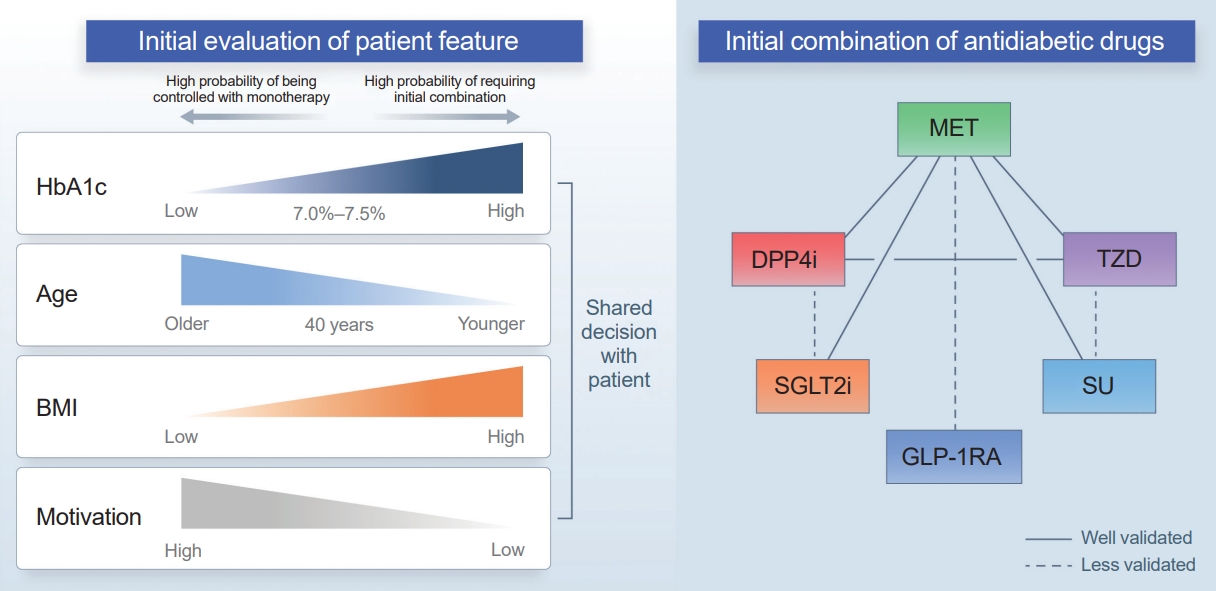
ePub - Type 2 diabetes (T2D) is a progressive disease in which it is challenging to achieve long-term durable glycemic control. However, intensive glycemic control is crucial for preventing diabetes-related complications. Previous studies showed that monotherapy with a stepwise add-on approach was seldom effective for long-term durable glycemic control. Combination therapy, which refers to the use of two or more drugs to control hyperglycemia, has multiple benefits, including the ability to target a variety of pathophysiological processes underlying hyperglycemia. In clinical trials, initial combination therapy showed better glycemic control than monotherapy or a stepwise approach. Emerging evidence indicates that initial combination therapy is associated with preserved β-cell function and fewer complications in T2D. However, cost-effectiveness and adverse events with combination therapy are issues that should be considered. Therefore, initial combination therapy is an important option for patients with T2D that clinicians should consider with a view toward balancing benefits and potential harms. In this review, we summarize the literature addressing initial combination therapy in T2D, and we suggest optimal strategies based on clinical situations and patient characteristics.

- Diabetes, Obesity and Metabolism
- Receptor-Mediated Muscle Homeostasis as a Target for Sarcopenia Therapeutics
- Jong Hyeon Yoon, Ki-Sun Kwon
- Endocrinol Metab. 2021;36(3):478-490. Published online June 28, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1081

- 8,781 View
- 331 Download
- 9 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Sarcopenia is a disease characterized by age-related decline of skeletal muscle mass and function. The molecular mechanisms of the pathophysiology of sarcopenia form a complex network due to the involvement of multiple interconnected signaling pathways. Therefore, signaling receptors are major targets in pharmacological strategies in general. To provide a rationale for pharmacological interventions for sarcopenia, we herein describe several druggable signaling receptors based on their role in skeletal muscle homeostasis and changes in their activity with aging. A brief overview is presented of the efficacy of corresponding drug candidates under clinical trials. Strategies targeting the androgen receptor, vitamin D receptor, Insulin-like growth factor-1 receptor, and ghrelin receptor primarily focus on promoting anabolic action using natural ligands or mimetics. Strategies involving activin receptors and angiotensin receptors focus on inhibiting catabolic action. This review may help to select specific targets or combinations of targets in the future.
-
Citations
Citations to this article as recorded by- The Current Landscape of Pharmacotherapies for Sarcopenia
Gulistan Bahat, Serdar Ozkok
Drugs & Aging.2024; 41(2): 83. CrossRef - Associations of micronutrient dietary patterns with sarcopenia among US adults: a population-based study
Yining Liu, Xiangliang Liu, Linnan Duan, Yixin Zhao, Yuwei He, Wei Li, Jiuwei Cui
Frontiers in Nutrition.2024;[Epub] CrossRef - Impact of Vitamin D Level on Sarcopenia in Elderly People: A Critical Review
Saniya Khan, Sunil Kumar, Sourya Acharya, Anil Wanjari
Journal of Health and Allied Sciences NU.2023; 13(04): 453. CrossRef - Novel Potential Targets for Function-Promoting Therapies: Orphan Nuclear Receptors, Anti-inflammatory Drugs, Troponin Activators, Mas Receptor Agonists, and Urolithin A
Waly Dioh, Vihang Narkar, Anurag Singh, Fady Malik, Luigi Ferrucci, Cendrine Tourette, Jean Mariani, Rob van Maanen, Roger A Fielding, Lewis A Lipsitz
The Journals of Gerontology: Series A.2023; 78(Supplement): 44. CrossRef - Alverine citrate promotes myogenic differentiation and ameliorates muscle atrophy
Jong Hyeon Yoon, Seung-Min Lee, Younglang Lee, Min Ju Kim, Jae Won Yang, Jeong Yi Choi, Ju Yeon Kwak, Kwang-Pyo Lee, Yong Ryoul Yang, Ki-Sun Kwon
Biochemical and Biophysical Research Communications.2022; 586: 157. CrossRef - Adeno-associated virus-mediated expression of an inactive CaMKIIβ mutant enhances muscle mass and strength in mice
Takahiro Eguchi, Yuji Yamanashi
Biochemical and Biophysical Research Communications.2022; 589: 192. CrossRef - Gastric Mobility and Gastrointestinal Hormones in Older Patients with Sarcopenia
Hsien-Hao Huang, Tse-Yao Wang, Shan-Fan Yao, Pei-Ying Lin, Julia Chia-Yu Chang, Li-Ning Peng, Liang-Kung Chen, David Hung-Tsang Yen
Nutrients.2022; 14(9): 1897. CrossRef - Molecular Mechanisms Underlying Intensive Care Unit-Acquired Weakness and Sarcopenia
Marcela Kanova, Pavel Kohout
International Journal of Molecular Sciences.2022; 23(15): 8396. CrossRef
- The Current Landscape of Pharmacotherapies for Sarcopenia

- Acute Hyperglycemia Associated with Anti-Cancer Medication
- Yul Hwangbo, Eun Kyung Lee
- Endocrinol Metab. 2017;32(1):23-29. Published online March 20, 2017
- DOI: https://doi.org/10.3803/EnM.2017.32.1.23
- 6,225 View
- 130 Download
- 41 Web of Science
- 43 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Hyperglycemia during chemotherapy occurs in approximately 10% to 30% of patients. Glucocorticoids and L-asparaginase are well known to cause acute hyperglycemia during chemotherapy. Long-term hyperglycemia is also frequently observed, especially in patients with hematologic malignancies treated with L-asparaginase-based regimens and total body irradiation. Glucocorticoid-induced hyperglycemia often develops because of increased insulin resistance, diminished insulin secretion, and exaggerated hepatic glucose output. Screening strategies for this condition include random glucose testing, hemoglobin A1c testing, oral glucose loading, and fasting plasma glucose screens. The management of hyperglycemia starts with insulin or sulfonylurea, depending on the type, dose, and delivery of the glucocorticoid formulation. Mammalian target of rapamycin (mTOR) inhibitors are associated with a high incidence of hyperglycemia, ranging from 13% to 50%. Immunotherapy, such as anti-programmed death 1 (PD-1) antibody treatment, induces hyperglycemia with a prevalence of 0.1%. The proposed mechanism of immunotherapy-induced hyperglycemia is an autoimmune process (insulitis). Withdrawal of the PD-1 inhibitor is the primary treatment for severe hyperglycemia. The efficacy of glucocorticoid therapy is not fully established and the decision to resume PD-1 inhibitor therapy depends on the severity of the hyperglycemia. Diabetic patients should achieve optimized glycemic control before initiating treatment, and glucose levels should be monitored periodically in patients initiating mTOR inhibitor or PD-1 inhibitor therapy. With regard to hyperglycemia caused by anti-cancer therapy, frequent monitoring and proper management are important for promoting the efficacy of anti-cancer therapy and improving patients' quality of life.
-
Citations
Citations to this article as recorded by- Bridging the Gap: Pancreas Tissue Slices From Organ and Tissue Donors for the Study of Diabetes Pathogenesis
Christian M. Cohrs, Chunguang Chen, Mark A. Atkinson, Denise M. Drotar, Stephan Speier
Diabetes.2024; 73(1): 11. CrossRef - Assessment of metabolic syndrome parameters in pediatric acute lymphoblastic leukemia survivors
Ömer Kartal, Orhan Gürsel
Indian Journal of Cancer.2023; 60(3): 325. CrossRef - Increased risk of incident diabetes after therapy with immune checkpoint inhibitor compared with conventional chemotherapy: A longitudinal trajectory analysis using a tertiary care hospital database
Minyoung Lee, Kyeongseob Jeong, Yu Rang Park, Yumie Rhee
Metabolism.2023; 138: 155311. CrossRef - Analysis of the Incidence of Type 2 Diabetes, Requirement of Insulin Treatment, and Diabetes-Related Complications among Patients with Cancer
Su Jung Lee, Chulho Kim, Hyunjae Yu, Dong-Kyu Kim
Cancers.2023; 15(4): 1094. CrossRef - A Case of Pembrolizumab-Induced Diabetic Ketoacidosis and Hyperthyroidism in a Patient With Recurrent Esophageal Adenocarcinoma
Jonathan Salangsang, Surendra Sapkota, Sanjeev Kharel, Prakash Gupta, Abhishek Kalla
Cureus.2023;[Epub] CrossRef - Link between Blood Cell-Associated Inflammatory Indices and Chemotherapy-Induced Hyperglycemia in Women Affected with Breast Cancer: Clinical Studies
Krishna Prasad, Suresh Rao, Sanath Kumar Hegde, Thomas George, Rhea Katherine D'souza, Sucharitha Suresh, Manjeshwar Shrinath Baliga
South Asian Journal of Cancer.2023; 12(02): 118. CrossRef - Insulin resistance in patients with cancer: a systematic review and meta-analysis
Joan M. Màrmol, Michala Carlsson, Steffen H. Raun, Mia K. Grand, Jonas Sørensen, Louise Lang Lehrskov, Erik A. Richter, Ole Norgaard, Lykke Sylow
Acta Oncologica.2023; 62(4): 364. CrossRef - Metabolic obesity phenotypes and obesity‐related cancer risk in the National Health and Nutrition Examination Survey
Maci Winn, Prasoona Karra, Heinz Freisling, Marc J. Gunter, Benjamin Haaland, Michelle L. Litchman, Jennifer A. Doherty, Mary C. Playdon, Sheetal Hardikar
Endocrinology, Diabetes & Metabolism.2023;[Epub] CrossRef - Effects of Vitamin Intake on Blood Glucose in Cancer Patients Undergoing Chemotherapy: Quantitative and Descriptive Research
Ji Yeong Kim, Kyung Hee Lim
Korean Journal of Adult Nursing.2023; 35(2): 148. CrossRef - Oncologists’ responsibility, comfort, and knowledge managing hyperglycemia in patients with cancer undergoing chemotherapy: a cross sectional study
Teresa M. Salgado, Rotana M. Radwan, Erin Hickey Zacholski, Emily Mackler, Tonya M. Buffington, Kerri T. Musselman, William J. Irvin, Jennifer M. Perkins, Trang N. Le, Dave L. Dixon, Karen B. Farris, Vanessa B. Sheppard, Resa M. Jones
Supportive Care in Cancer.2023;[Epub] CrossRef - Diabetes management in cancer patients. An Italian Association of Medical Oncology, Italian Association of Medical Diabetologists, Italian Society of Diabetology, Italian Society of Endocrinology and Italian Society of Pharmacology multidisciplinary conse
N. Silvestris, T. Franchina, M. Gallo, A. Argentiero, A. Avogaro, G. Cirino, A. Colao, R. Danesi, G. Di Cianni, S. D’Oronzo, A. Faggiano, S. Fogli, D. Giuffrida, S. Gori, N. Marrano, R. Mazzilli, M. Monami, M. Montagnani, L. Morviducci, A. Natalicchio, A.
ESMO Open.2023; 8(6): 102062. CrossRef - Prognostic Factors for Hyperglycemia in Patients Receiving Chemotherapy
Jiyeong Kim, Kyung Hee Lim
Cancer Nursing.2023;[Epub] CrossRef - Severe Insulin Resistance in a Patient Treated With Nivolumab and Brentuximab-Vedotin for Hodgkin Lymphoma
Elif Tama, Meghan Black, Muhamad Alhaj Moustafa, Maria D Hurtado
JCEM Case Reports.2023;[Epub] CrossRef - A New Hypothesis Describing the Pathogenesis of Oral Mucosal Injury Associated with the Mammalian Target of Rapamycin (mTOR) Inhibitors
Stephen T. Sonis, Alessandro Villa
Cancers.2023; 16(1): 68. CrossRef - Management of Phosphatidylinositol-3-Kinase Inhibitor-Associated Hyperglycemia
Marcus D. Goncalves, Azeez Farooki
Integrative Cancer Therapies.2022; 21: 153473542110731. CrossRef - Metformin Induced Cognitive Impairment and Neuroinflammation in CMF-Treated Rats
Ahmad H. Alhowai, Yasser Almogbel, Ahmed A.H. Abdel, Maha A. Aldubay, Hani A. Alfheeaid, Shatha G. Felemban, Sridevi Chigurupat, Ibrahim F. Alharbi, Hindi S. Alharbi
International Journal of Pharmacology.2022; 18(2): 228. CrossRef - Glucose Influences the Response of Glioblastoma Cells to Temozolomide and Dexamethasone
Anna M Bielecka-Wajdman, Tomasz Ludyga, Daria Smyk, Wojciech Smyk, Magdalena Mularska, Patrycja Świderek, Wojciech Majewski, Christina Susanne Mullins, Michael Linnebacher, Ewa Obuchowicz
Cancer Control.2022; 29: 107327482210754. CrossRef - Cardiometabolic Comorbidities in Cancer Survivors
Leah L. Zullig, Anthony D. Sung, Michel G. Khouri, Shelley Jazowski, Nishant P. Shah, Andrea Sitlinger, Dan V. Blalock, Colette Whitney, Robin Kikuchi, Hayden B. Bosworth, Matthew J. Crowley, Karen M. Goldstein, Igor Klem, Kevin C. Oeffinger, Susan Dent
JACC: CardioOncology.2022; 4(2): 149. CrossRef - Glucose deprivation reduces proliferation and motility, and enhances the anti-proliferative effects of paclitaxel and doxorubicin in breast cell lines in vitro
Maitham A. Khajah, Sarah Khushaish, Yunus A. Luqmani, Yi-Hsien Hsieh
PLOS ONE.2022; 17(8): e0272449. CrossRef - Gemigliptin exerts protective effects against doxorubicin-induced hepatotoxicity by inhibiting apoptosis via the regulation of fibroblast growth factor 21 expression
Kyeong-Min Lee, Yeo Jin Hwang, Gwon-Soo Jung
Biochemical and Biophysical Research Communications.2022; 626: 135. CrossRef - Glucocorticoid-Induced Hyperglycemia in Oncologic Outpatients: A Narrative Review Using the Quadruple Aim Framework
Ihab Kandil, Erin Keely
Canadian Journal of Diabetes.2022; 46(7): 730. CrossRef - Real-World Experience of Monitoring Practice of Endocrinopathies Associated with the Use of Novel Targeted Therapies among Patients with Solid Tumors
Atika AlHarbi, Majed Alshamrani, Mansoor Khan, Abdelmajid Alnatsheh, Mohammed Aseeri
Medical Sciences.2022; 10(4): 65. CrossRef - The Assessment of the Hypothalamic-Pituitary-Adrenal Axis After Oncological Treatment in Pediatric Patients with Acute Lymphoblastic Leukemia
Barbara Hull, Anna Wedrychowicz, Magdalena Ossowska, Aleksandra Furtak, Joanna Badacz, Szymon Skoczeń, Jerzy B. Starzyk
Journal of Clinical Research in Pediatric Endocrinology.2022; 14(4): 393. CrossRef - Targeting Mitochondria and Oxidative Stress in Cancer- and Chemotherapy-Induced Muscle Wasting
Joshua R. Huot, Dryden Baumfalk, Aridai Resendiz, Andrea Bonetto, Ashley J. Smuder, Fabio Penna
Antioxidants & Redox Signaling.2022;[Epub] CrossRef - Onkodiabetológia III.
Róbert János Bánhegyi, Blanka Veréb, Andrea Gazdag, Beatrix Rácz, Róbert Wagner, Norbert Fülöp, Béla Pikó
Orvosi Hetilap.2022; 163(41): 1614. CrossRef - Economic burden of diabetes among medicare beneficiaries with cancer
Cassidi C McDaniel, F Ellen Loh, Devan M Rockwell, Courtney P McDonald, Chiahung Chou
Journal of Pharmaceutical Health Services Research.2021; 12(2): 142. CrossRef - The prognostic outcome of ‘type 2 diabetes mellitus and breast cancer’ association pivots on hypoxia-hyperglycemia axis
Ilhaam Ayaz Durrani, Attya Bhatti, Peter John
Cancer Cell International.2021;[Epub] CrossRef - Increased risk of diabetes in cancer survivors: a pooled analysis of 13 population-based cohort studies
Y. Xiao, H. Wang, Y. Tang, J. Yan, L. Cao, Z. Chen, Z. Shao, Z. Mei, Z. Jiang
ESMO Open.2021; 6(4): 100218. CrossRef - Sublethal concentrations of high glucose prolong mitotic arrest in a spindle assembly checkpoint activity dependent manner in budding yeast
Pinar B. Thomas, Elif E. Cavusoglu, Nur Kaluc
Biologia.2021; 76(12): 3883. CrossRef - Hyperglycemia in Childhood Acute Lymphoblastic Leukemia During Induction Chemotherapy
Nengcy Erlina Tasik Rerung, Andi Cahyadi, Nur Rochmah, Maria Christina Shanty Larasati, Mia Ratwita Andarsini, Muhammad Faizi, IDG Ugrasena, Bambang Permono
MEDICINUS.2021; 34(1): 18. CrossRef - Effect of Acute Chemotherapy on Glucose Levels in Rats
Ahmad H. Alhowail, Gena S. Alfawzan, Maha A. Aldubayan, Lolwah S. Alsalam
International Journal of Pharmacology.2020; 16(3): 276. CrossRef - Predictors of Disease Progression or Performance Status Decline in Patients Undergoing Neoadjuvant Therapy for Localized Pancreatic Head Adenocarcinoma
Alessandro Paniccia, Ana L. Gleisner, Mazen S. Zenati, Amr I. Al Abbas, Jae Pil Jung, Nathan Bahary, Kenneth K. W. Lee, David Bartlett, Melissa E. Hogg, Herbert J. Zeh, Amer H. Zureikat
Annals of Surgical Oncology.2020; 27(8): 2961. CrossRef - Fasting to enhance Cancer treatment in models: the next steps
Jing Zhang, Yanlin Deng, Bee Luan Khoo
Journal of Biomedical Science.2020;[Epub] CrossRef - Concurrent diabetic ketoacidosis and pancreatitis in Paediatric acute lymphoblastic leukemia receiving L-asparaginase
Patel Zeeshan Jameel, Sham Lohiya, Amol Dongre, Sachin Damke, Bhavana B. Lakhkar
BMC Pediatrics.2020;[Epub] CrossRef - Hyperglycemia during Adjuvant Chemotherapy as a Prognostic Factor in Breast Cancer Patients without Diabetes
Ha Rim Ahn, Sang Yull Kang, Hyun Jo Youn, Sung Hoo Jung
Journal of Breast Cancer.2020; 23(4): 398. CrossRef - Side effects of adjuvant chemotherapy and their impact on outcome in elderly breast cancer patients: a cohort study
Valentina Zanuso, Vittorio Fregoni, Lorenzo Gervaso
Future Science OA.2020; : FSO617. CrossRef - Incidence of Hyperglycemia/Secondary Diabetes in Women who have Undergone Curative Chemotherapy for Breast Cancer: First Study from India
Suresh Rao, Krishna Prasad, Soniya Abraham, Thomas George, Supreeth Kakkaje Chandran, Manjeshwar Shrinath Baliga
South Asian Journal of Cancer.2020; 09(03): 130. CrossRef - Hyperglycemic ADR Distribution of Doxorubicin From VigiBase
Jincheng Yang, Jun Yang
American Journal of Therapeutics.2019; 26(3): e428. CrossRef - Hyperglycemia During Childhood Cancer Therapy: Incidence, Implications, and Impact on Outcomes
Allison Grimes, Ashraf Mohamed, Jenna Sopfe, Rachel Hill, Jane Lynch
JNCI Monographs.2019; 2019(54): 132. CrossRef - Steroid-induced diabetes in cancer patients
Gemma Dinn
Journal of Prescribing Practice.2019; 1(12): 610. CrossRef - Risk Factors for Doxorubicin-Induced Serious Hyperglycaemia-Related Adverse Drug Reactions
Jincheng Yang, Yu Wang, Kang Liu, Wen Yang, Jianying Zhang
Diabetes Therapy.2019; 10(5): 1949. CrossRef - Effect of glucose and palmitate environment on proliferation and migration of PC3‐prostate cancer cells
Lívia Prometti Rezende, Maria Raquel Unterkircher Galheigo, Breno Costa Landim, Amanda Rodrigues Cruz, Françoise Vasconcelos Botelho, Renata Graciele Zanon, Rejane Maira Góes, Daniele Lisboa Ribeiro
Cell Biology International.2019; 43(4): 373. CrossRef - Incidence of Diabetes After Cancer Development
Yul Hwangbo, Danbee Kang, Minwoong Kang, Saemina Kim, Eun Kyung Lee, Young Ae Kim, Yoon Jung Chang, Kui Son Choi, So-Youn Jung, Sang Myung Woo, Jin Seok Ahn, Sung Hoon Sim, Yun Soo Hong, Roberto Pastor-Barriuso, Eliseo Guallar, Eun Sook Lee, Sun-Young Kon
JAMA Oncology.2018; 4(8): 1099. CrossRef
- Bridging the Gap: Pancreas Tissue Slices From Organ and Tissue Donors for the Study of Diabetes Pathogenesis

- Obesity and Metabolism
- Antiobesity Pharmacotherapy for Patients with Type 2 Diabetes: Focus on Long-Term Management
- Won Seon Jeon, Cheol-Young Park
- Endocrinol Metab. 2014;29(4):410-417. Published online December 29, 2014
- DOI: https://doi.org/10.3803/EnM.2014.29.4.410
- 3,521 View
- 41 Download
- 11 Web of Science
- 14 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Type 2 diabetes and obesity have a complex relationship; obesity is linked to insulin resistance, the precursor to type 2 diabetes. The management of obesity is an important method to delay onset of diabetes and improve the glycemic durability of antidiabetic agents. However, insulin and some of the oral hypoglycemic agents used to treat diabetes cause significant weight gain, and it is difficult for patients with diabetes to reduce and maintain their weight by life-style changes alone. Thus, antiobesity medications or bariatric surgery may be a necessary adjunct for certain obese patients with diabetes. In 2012, the U.S. Food and Drug Administration (FDA) approved lorcaserin and phentermine/topiramate extended-release for the management of chronic weight, and approval for naltrexone/bupropion sustained-release as an adjunct to exercise and reduced caloric intake followed in 2014. Liraglutide is pending FDA approval for antiobesity drug. Here we review the efficacy of approved and new promising drugs for the management of obesity.
-
Citations
Citations to this article as recorded by- A new kind of diabetes medication approved by the FDA: is there hope for obesity?
Danisha Dhirani, Ahmad Shahid, Hassan Mumtaz
International Journal of Surgery.2023; 109(2): 81. CrossRef - Current pharmacological approaches in obesity treatment
Pelin TİRYAKİOĞLU, Hüseyin YILMAZ, İsmail DEMİR, İsmail YILMAZ
DAHUDER Medical Journal.2023; 3(2): 32. CrossRef - Estudio del potencial antidiabético y antiobesidad de las hojas de Neurolaena lobata (Asteraceae)
Yohum S Lozada-Diaz, Oscar J Patiño-Ladino, Fabián H López-Vallejo, Kevin P Lévuok-Mena, Juliet A Prieto-Rodríguez
Revista Productos Naturales.2022; 5(2): 70. CrossRef - Indikationsstellung in der Adipositastherapie – Surgeons first? // Indications in obesity therapy - surgeons first?
Maximilian von Heesen
Zentralblatt für Chirurgie - Zeitschrift für Allgemeine, Viszeral-, Thorax- und Gefäßchirurgie.2022; 147(06): 525. CrossRef - Anti-Obesity Drugs: Long-Term Efficacy and Safety: An Updated Review
Young Jin Tak, Sang Yeoup Lee
The World Journal of Men's Health.2021; 39(2): 208. CrossRef - Long-Term Efficacy and Safety of Anti-Obesity Treatment: Where Do We Stand?
Young Jin Tak, Sang Yeoup Lee
Current Obesity Reports.2021; 10(1): 14. CrossRef - Weight-centric pharmacological management of type 2 diabetes mellitus – An essential component of cardiovascular disease prevention
Emir Muzurović, Siniša Dragnić, Sanja Medenica, Brigita Smolović, Predrag Bulajić, Dimitri P. Mikhailidis
Journal of Diabetes and its Complications.2020; 34(8): 107619. CrossRef - Diet-induced obese alters the expression and function of hepatic drug-metabolizing enzymes and transporters in rats
Lei Zhang, Peipei Xu, Yi Cheng, Peili Wang, Xinrun Ma, Mingyao Liu, Xin Wang, Feng Xu
Biochemical Pharmacology.2019; 164: 368. CrossRef - Updates on obesity pharmacotherapy
Amanda Velazquez, Caroline M. Apovian
Annals of the New York Academy of Sciences.2018; 1411(1): 106. CrossRef - Effects of Obex in Overweight and Obese Subjects With or Without Impaired Fasting Glucose: A Pilot Study
Eduardo Cabrera-Rode, Janet Rodríguez, Aimee Álvarez, Ragmila Echevarría, Antonio Darwin Reyes, Ileana Cubas-Dueñas, Silvia Elena Turcios-Tristá, Oscar Díaz-Díaz
Journal of Dietary Supplements.2017; 14(6): 626. CrossRef - Obesity context of type 2 diabetes and medication perspectives
Abha Pandit, Abhay Kumar Pandey
Apollo Medicine.2016; 13(2): 91. CrossRef - Fatty acid metabolism and the basis of brown adipose tissue function
María Calderon-Dominguez, Joan F. Mir, Raquel Fucho, Minéia Weber, Dolors Serra, Laura Herrero
Adipocyte.2016; 5(2): 98. CrossRef - The Perioperative Implications of New Weight Loss Drugs
Jessica A. Darnobid, Stephanie B. Jones
Advances in Anesthesia.2016; 34(1): 1. CrossRef - Articles in 'Endocrinology and Metabolism' in 2014
Won-Young Lee
Endocrinology and Metabolism.2015; 30(1): 47. CrossRef
- A new kind of diabetes medication approved by the FDA: is there hope for obesity?

- Adrenal gland
- Adult Multisystem Langerhans Cell Histiocytosis Presenting with Central Diabetes Insipidus Successfully Treated with Chemotherapy
- Jung-Eun Choi, Hae Ri Lee, Jung Hun Ohn, Min Kyong Moon, Juri Park, Seong Jin Lee, Moon-Gi Choi, Hyung Joon Yoo, Jung Han Kim, Eun-Gyoung Hong
- Endocrinol Metab. 2014;29(3):394-399. Published online September 25, 2014
- DOI: https://doi.org/10.3803/EnM.2014.29.3.394
- 3,915 View
- 31 Download
- 6 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader We report the rare case of an adult who was diagnosed with recurrent multisystem Langerhans cell histiocytosis (LCH) involving the pituitary stalk and lung who present with central diabetes insipidus and was successfully treated with systemic steroids and chemotherapy. A 49-year-old man visited our hospital due to symptoms of polydipsia and polyuria that started 1 month prior. Two years prior to presentation, he underwent excision of right 6th and 7th rib lesions for the osteolytic lesion and chest pain, which were later confirmed to be LCH on pathology. After admission, the water deprivation test was done and the result indicated that he had central diabetes insipidus. Sella magnetic resonance imaging showed a mass on the pituitary stalk with loss of normal bright spot at the posterior lobe of the pituitary. Multiple patchy infiltrations were detected in both lung fields by computed tomography (CT). He was diagnosed with recurrent LCH and was subsequently treated with inhaled desmopressin, systemic steroids, vinblastine, and mercaptopurine. The pituitary mass disappeared after two months and both lungs were clear on chest CT after 11 months. Although clinical remission in multisystem LCH in adults is reportedly rare, our case of adult-onset multisystem LCH was treated successfully with systemic chemotherapy using prednisolone, vinblastine, and 6-mercaptopurine, which was well tolerated.
-
Citations
Citations to this article as recorded by- Adult localized Langerhans cell histiocytosis: A case report
Pan-Pan Yang, Su-Ye Hu, Xu-Ya Chai, Xiao-Meng Shi, Li-Xia Liu, Ling-E Li
World Journal of Clinical Cases.2023; 11(34): 8164. CrossRef - Adult Langerhans Cell Histiocytosis Masquerading as Hidradenitis Suppurativa
Jason Chertoff, Julian Chung, Ali Ataya
American Journal of Respiratory and Critical Care Medicine.2017; 195(8): e34. CrossRef - Articles in 'Endocrinology and Metabolism' in 2014
Won-Young Lee
Endocrinology and Metabolism.2015; 30(1): 47. CrossRef - Pulmonary Langerhans Cell Histiocytosis in an Adult Male Presenting with Central Diabetes Insipidus and Diabetes Mellitus: A Case Report
Yeun Seoung Choi, Jung Soo Lim, Woocheol Kwon, Soon-Hee Jung, Il Hwan Park, Myoung Kyu Lee, Won Yeon Lee, Suk Joong Yong, Seok Jeong Lee, Ye-Ryung Jung, Jiwon Choi, Ji Sun Choi, Joon Taek Jeong, Jin Sae Yoo, Sang-Ha Kim
Tuberculosis and Respiratory Diseases.2015; 78(4): 463. CrossRef - Adult-onset Langerhans cell histiocytosis presenting with adipsic diabetes insipidus, diabetes mellitus and hypopituitarism: A case report and review of literature
Erick S. Mendoza, Amy A. Lopez, Valerie Ann U. Valdez, Jean D. Uy-Ho, Sjoberg A. Kho
Journal of Clinical and Translational Endocrinology: Case Reports.2015; 1(1): 1. CrossRef
- Adult localized Langerhans cell histiocytosis: A case report

- Antibody-dependent Cell-mediated Cytotoxitity as a Prognostic Indicator in the Medical Treatment of Graves' Disease.
- Kwan Woo Lee, Young Goo Shin, Hye Rim Ro, Sung Kyu Lee, Yun Suk Chung, Hyun Man Kim, Yoon Jung Kim, Eun Kyung Hong, Bong Nam Chae
- J Korean Endocr Soc. 1998;13(4):554-562. Published online January 1, 2001
- 1,048 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The several forms of treatment of Graves disease-thyroidectomy, antithyroid drugs and radioiodide therapy-are in wide use now. But which therapy is best is a matter of debate. Some authors reported that in patients who underwent thyroidectomy, higher titers of serum antimicrosomal antibody were associated with 1) higher formation rates of germinal centers, 2) more lymphocyte infiltration in the thyroid tissue, 3) higher incidence of hypothyroidism, and 4) lower incidence of recurrence. We were interested in the relationship of thyroid autoantibody titers, ADCC(antibody-dependent cell-mediated cytotoxicity) activity and the clinical response to antithyroid medication. METHODS: We measured ADCC activities from patients in Graves disease(n-48), Hashimoto thyroiditis(n=17) and normal control(n=9). The patients of Graves disease were followed up for more than 1 year, and they were grouped into A(n=17, well responsed group to antithyroid medication) and B(n=31, poorly responsed group). We examined ADCC activities of patients' sera by chromium release assay. RESULTS: 1) Mean age of patients with Graves disease was 34.4210.4 years and 15 patients were male(31%). 2) Results of thyroid function tests of the Graves' patients were T 585.9 +/- 255.3 ng/dL, T4 21.3 +/- 12.2 mg/dL, TSH 0.11 +/- 0.06mIU/mL. Concentrations of antimicrosomal antibody, antithyroglobulin antibody and thyrotropin binding inhibitory immunoglobulin were 1279.1 +/- 1486.7 IU/mL, 488.1 +/- 751.1 IU/mL, and 38.5 +/- 33.4U/L respectively. 3) There was no significant difference between levels of thyroid hormones or concentrations of thyroid autoantibodies and ADCC activities in graves patients. 4) The ADCC activity of the Graves patient group(24.49%) was significantly higher than that of the normal control group(3.76%), and significantly lower than that of the Hashimotos thyroiditis group(36.34%). 5) There was no significant difference in ADCC activity between group A(18.24 +/- 13.44%) and B(27.91 +20.02%). CONCLUSION: From this results, we suggested that ADCC activity seems to be no value as a prognostic factor in predicting the response to antithyroid drugs in Graves disease patients. But, further studies, larger number of patients and long-term follow up, are needed.


 KES
KES

 First
First Prev
Prev



