Search
- Page Path
- HOME > Search
- Calcium & bone metabolism
- Persistence with Denosumab in Male Osteoporosis Patients: A Real-World, Non-Interventional Multicenter Study
- Chaiho Jeong, Jeongmin Lee, Jinyoung Kim, Jeonghoon Ha, Kwanhoon Jo, Yejee Lim, Mee Kyoung Kim, Hyuk-Sang Kwon, Tae-Seo Sohn, Ki-Ho Song, Moo Il Kang, Ki-Hyun Baek
- Endocrinol Metab. 2023;38(2):260-268. Published online April 27, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1663
- 1,702 View
- 106 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Persistence with denosumab in male patients has not been adequately investigated, although poor denosumab persistence is associated with a significant risk of rebound vertebral fractures.
Methods
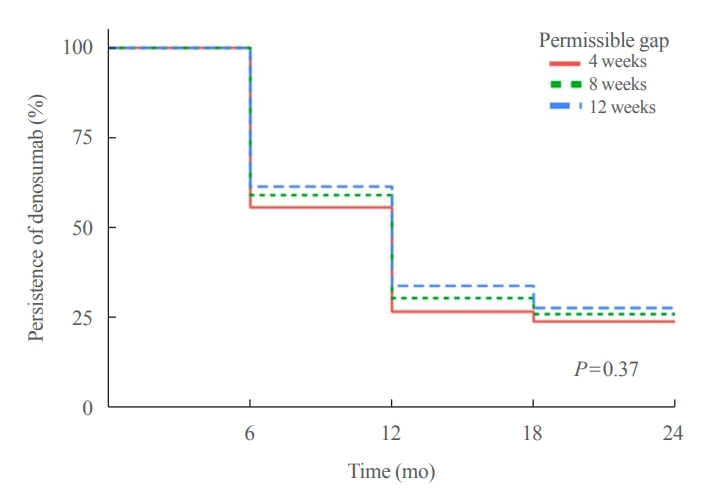
We retrospectively evaluated 294 Korean male osteoporosis patients treated with denosumab at three medical centers and examined their persistence with four doses of denosumab injection over 24 months of treatment. Persistence was defined as the extent to which a patient adhered to denosumab treatment in terms of the prescribed interval and dose, with a permissible gap of 8 weeks. For patients who missed their scheduled treatment appointment(s) during the follow-up period (i.e., no-shows), Cox proportional regression analysis was conducted to explore the factors associated with poor adherence. Several factors were considered, such as age, prior anti-osteoporotic drug use, the treatment provider’s medical specialty, the proximity to the medical center, and financial burdens of treatment.
Results
Out of 294 male patients, 77 (26.2%) completed all four sequential rounds of the denosumab treatment. Out of 217 patients who did not complete the denosumab treatment, 138 (63.6%) missed the scheduled treatment(s). Missing treatment was significantly associated with age (odds ratio [OR], 1.03), prior bisphosphonate use (OR, 0.76), and prescription by non-endocrinologists (OR, 2.24). Denosumab was stopped in 44 (20.3%) patients due to medical errors, in 24 (11.1%) patients due to a T-score improvement over –2.5, and in five (2.3%) patients due to expected dental procedures.
Conclusion
Our study showed that only one-fourth of Korean male osteoporosis patients were fully adherent to 24 months of denosumab treatment. -
Citations
Citations to this article as recorded by- Denosumab
Reactions Weekly.2023; 1963(1): 206. CrossRef
- Denosumab

- Calcium & Bone Metabolism
- Real-World Safety and Effectiveness of Denosumab in Patients with Osteoporosis: A Prospective, Observational Study in South Korea
- Yumie Rhee, Dong-Gune Chang, Jeonghoon Ha, Sooa Kim, Yusun Lee, Euna Jo, Jung-Min Koh
- Endocrinol Metab. 2022;37(3):497-505. Published online June 3, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1427

- 5,265 View
- 263 Download
- 8 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
The efficacy and safety of denosumab have been established in a phase 3, randomized, placebo-controlled trial in Korean postmenopausal women with osteoporosis. This postmarketing surveillance study was aimed to investigate the safety and effectiveness of denosumab in Korean real-world clinical practice.
Methods
Patients with osteoporosis who had received denosumab per the Korean approved indications in the postmarketing setting between September 2014 and September 2019 were enrolled. The primary endpoint was the incidence of adverse events (AEs) and adverse drug reactions (ADRs). The secondary endpoint was the percent change from baseline in bone mineral density (BMD) of the lumbar spine, total hip, and femoral neck.
Results
Of the 3,221 patients enrolled, 3,185 were included in the safety analysis set; 2,973 (93.3%) were female, and the mean± standard deviation (SD) age was 68.9±9.9 years. The mean±SD study period was 350.0±71.4 days. AEs, fatal AEs, and ADRs occurred in 19.3%, 0.8%, and 1.6%, respectively. The most frequent AEs, occurring in >0.5% of patients, were dizziness (0.7%), arthralgia (0.7%), back pain (0.6%), and myalgia (0.6%). Hypocalcemia occurred in 0.3% of patients. There were no cases of osteonecrosis of the jaw and atypical femoral fracture. Mean±SD percent change from baseline in BMD of the lumbar spine, total hip, and femoral neck was 7.3%±23.6%, 3.6%±31.4%, and 3.2%±10.7%, respectively.
Conclusion
The safety and effectiveness of denosumab in Korean patients with osteoporosis in this study were comparable with those in the Korean randomized controlled trial, with no new safety findings. -
Citations
Citations to this article as recorded by- Prevalence of denosumab-induced hypocalcemia: a retrospective observational study of patients routinely monitored with ionized calcium post-injection
Anna Spångeus, Johan Rydetun, Mischa Woisetschläger
Osteoporosis International.2024; 35(1): 173. CrossRef - Cost-consequence analysis of continuous denosumab therapy for osteoporosis treatment in South Korea
Seungju Cha, Minjeong Sohn, Hyowon Yang, Eric J. Yeh, Ki-Hyun Baek, Jeonghoon Ha, Hyemin Ku
BMC Musculoskeletal Disorders.2024;[Epub] CrossRef - Denosumab and the Risk of Diabetes in Patients Treated for Osteoporosis
Huei-Kai Huang, Albert Tzu-Ming Chuang, Tzu-Chi Liao, Shih-Chieh Shao, Peter Pin-Sung Liu, Yu-Kang Tu, Edward Chia-Cheng Lai
JAMA Network Open.2024; 7(2): e2354734. CrossRef - Adverse Effects of Denosumab in Kidney Transplant Recipients: A 20-Year Retrospective Single-Center Observation Study in Central Taiwan
Tsung-Yin Tsai, Zi-Hong You, Shang-Feng Tsai, Ming-Ju Wu, Tung-Min Yu, Ya-Wen Chuang, Yung-Chieh Lin, Ya-Lian Deng, Chiann-Yi Hsu, Cheng-Hsu Chen
Transplantation Proceedings.2023; 55(4): 837. CrossRef - Persistence with Denosumab in Male Osteoporosis Patients: A Real-World, Non-Interventional Multicenter Study
Chaiho Jeong, Jeongmin Lee, Jinyoung Kim, Jeonghoon Ha, Kwanhoon Jo, Yejee Lim, Mee Kyoung Kim, Hyuk-Sang Kwon, Tae-Seo Sohn, Ki-Ho Song, Moo Il Kang, Ki-Hyun Baek
Endocrinology and Metabolism.2023; 38(2): 260. CrossRef - Effect of Denosumab on Bone Density in Postmenopausal Osteoporosis: A Comparison with and without Calcium Supplementation in Patients on Standard Diets in Korea
Chaiho Jeong, Jinyoung Kim, Jeongmin Lee, Yejee Lim, Dong-Jun Lim, Ki-Hyun Baek, Jeonghoon Ha
Journal of Clinical Medicine.2023; 12(21): 6904. CrossRef - Denosumab
Reactions Weekly.2022; 1919(1): 221. CrossRef - Denosumab, an effective osteoporosis treatment option for men
Sung Hye Kong
The Korean Journal of Internal Medicine.2022; 37(5): 947. CrossRef
- Prevalence of denosumab-induced hypocalcemia: a retrospective observational study of patients routinely monitored with ionized calcium post-injection

- Calcium & Bone Metabolism
- Discontinuing Denosumab: Can It Be Done Safely? A Review of the Literature
- Wei Lin Tay, Donovan Tay
- Endocrinol Metab. 2022;37(2):183-194. Published online April 14, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1369

- 15,965 View
- 888 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
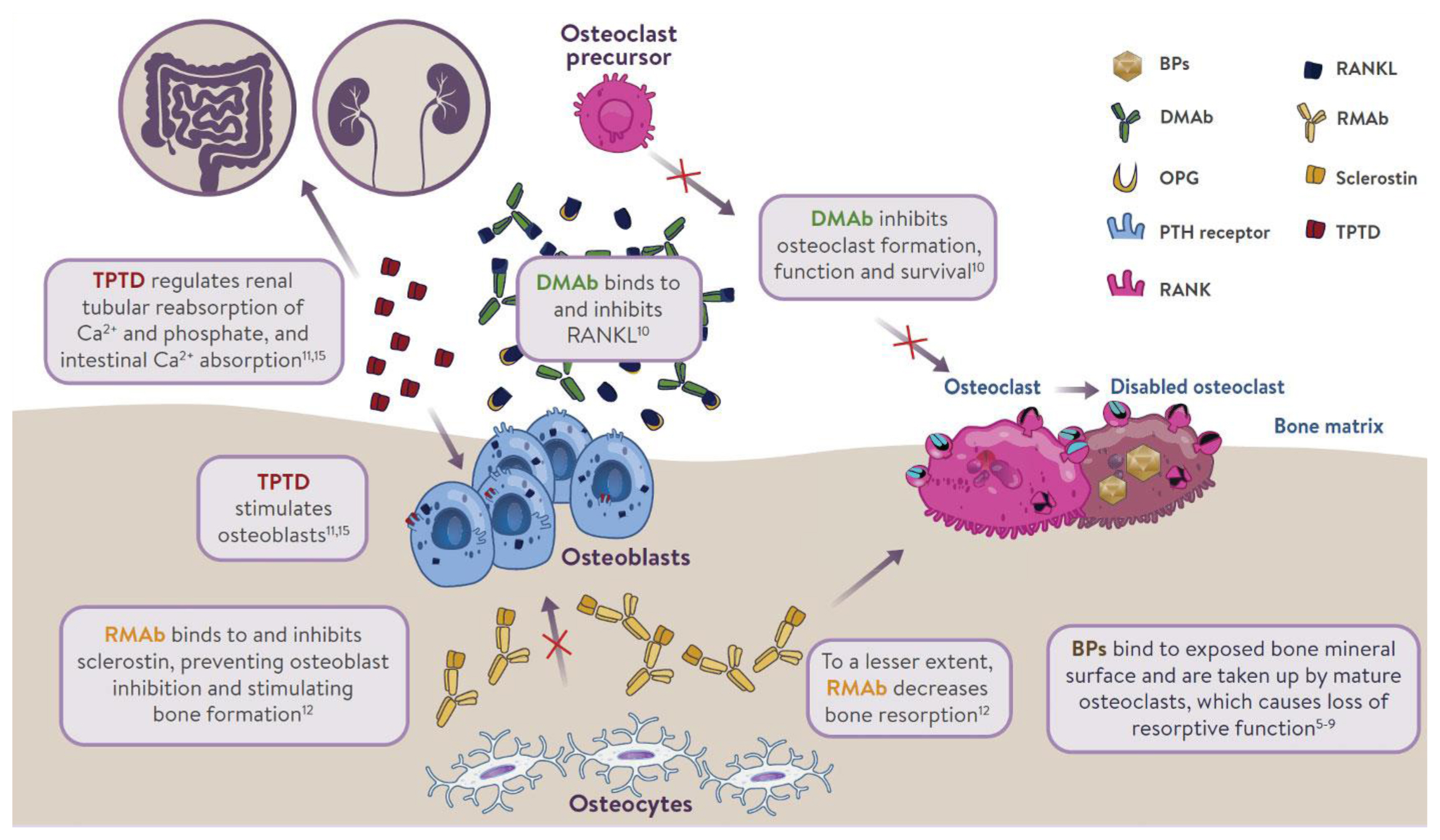
ePub - Denosumab, which has been approved for the treatment of osteoporosis since 2010, is a fully humanised monoclonal antibody against a cytokine, receptor activator of nuclear factor kappa B ligand (RANKL), involved in bone resorption. Continued use of denosumab results in a potent and sustained decrease in bone turnover, an increase in bone mineral density (BMD), and a reduction in vertebral and hip fractures. The anti-resorptive effects of denosumab are reversible upon cessation, and this reversal is accompanied by a transient marked increase in bone turnover that is associated with bone loss, and of concern, an increased risk of multiple vertebral fractures. In this review, we outline the effects of denosumab withdrawal on bone turnover markers, BMD, histomorphometry, and fracture risk. We provide an update on recent clinical trials that sought to answer how clinicians can transition away from denosumab safely with follow-on therapy to mitigate bone loss and summarise the recommendations of various international guidelines.
-
Citations
Citations to this article as recorded by- Loss of lower extremity bone mineral density 1 year after denosumab is discontinued in persons with subacute spinal cord injury
Christopher M. Cirnigliaro, Michael F. La Fountaine, J. Scott Parrott, Steven C. Kirshblum, Susan J. Sauer, Sue A. Shapses, Isa A. McClure, William A. Bauman
Osteoporosis International.2023; 34(4): 741. CrossRef - Persistence with Denosumab in Male Osteoporosis Patients: A Real-World, Non-Interventional Multicenter Study
Chaiho Jeong, Jeongmin Lee, Jinyoung Kim, Jeonghoon Ha, Kwanhoon Jo, Yejee Lim, Mee Kyoung Kim, Hyuk-Sang Kwon, Tae-Seo Sohn, Ki-Ho Song, Moo Il Kang, Ki-Hyun Baek
Endocrinology and Metabolism.2023; 38(2): 260. CrossRef
- Loss of lower extremity bone mineral density 1 year after denosumab is discontinued in persons with subacute spinal cord injury

- Calcium & Bone Metabolism
- Review and Update of the Risk Factors and Prevention of Antiresorptive-Related Osteonecrosis of the Jaw
- Ha Young Kim
- Endocrinol Metab. 2021;36(5):917-927. Published online October 21, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1170

- 4,384 View
- 267 Download
- 8 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Antiresorptive-related osteonecrosis of the jaw (ARONJ) is a rare but serious adverse event of bisphosphonate or denosumab administration; it is associated with severe pain and a deteriorated quality of life. Since its first report in 2003, there have been many studies on its definition, epidemiology, pathophysiology, diagnosis, and treatment. Nevertheless, the epidemiology and mechanisms underlying this condition have not yet been fully delineated and several risk factors are known. Moreover, as there is no effective treatment currently available for osteonecrosis of the jaw, prevention is essential. Furthermore, close cooperation between prescribing physicians and dentists is important. The aim of this review was to provide up-to-date information regarding the risk factors and prevention of ARONJ from a physician’s perspective.
-
Citations
Citations to this article as recorded by- Risk factors for dental findings of the development of medication-related osteonecrosis of the jaw: Investigation of 3734 teeth in cancer patients receiving high dose antiresorptive agents
Mitsunobu Otsuru, Yoshinari Fujiki, Sakiko Soutome, Norio Nakamura, Taro Miyoshi, Tomofumi Naruse, Mizuho Ohnuma, Yuka Hotokezaka, Satoshi Rokutanda, Masahiro Umeda
Journal of Dental Sciences.2024; 19(1): 203. CrossRef - Editorial: Immunological processes in maxillofacial bone pathology
Matthias Tröltzsch
Frontiers in Immunology.2024;[Epub] CrossRef - Polysacharide of Agaricus blazei gel mitigates bone necrosis in model of the jaws related to bisphosphonate via Wnt signaling
Vanessa Costa de Sousa, Fátima Regina Nunes Sousa, Raquel Felipe Vasconcelos, Gisele Angelino Barreto, Conceição S. Martins, Nilson Romero Dias, Sislana Costa, Maria Jennifer Chaves Bernardino, George de Almeida Silva, Nadine Linhares, Delane Gondim, Mirn
Scientific Reports.2024;[Epub] CrossRef - When and how to stop denosumab therapy in a patient with osteoporosis
Eirena L. Goulden, Rachel K. Crowley
Clinical Endocrinology.2023; 98(5): 649. CrossRef - Clinical and Histopathological Aspects of MRONJ in Cancer Patients
George Adrian Ciobanu, Laurențiu Mogoantă, Adrian Camen, Mihaela Ionescu, Daniel Vlad, Ionela Elisabeta Staicu, Cristina Maria Munteanu, Mircea Ionuț Gheorghiță, Răzvan Mercuț, Elena Claudia Sin, Sanda Mihaela Popescu
Journal of Clinical Medicine.2023; 12(10): 3383. CrossRef - Bisphosphonates and osteonecrosis of the jaws: Clinical and forensic aspects
Diana Nogueira, Inês Morais Caldas, Ricardo Jorge Dinis-Oliveira
Archives of Oral Biology.2023; 155: 105792. CrossRef - Correlations between Immune Response and Etiopathogenic Factors of Medication-Related Osteonecrosis of the Jaw in Cancer Patients Treated with Zoledronic Acid
George Adrian Ciobanu, Laurențiu Mogoantă, Sanda Mihaela Popescu, Mihaela Ionescu, Cristina Maria Munteanu, Ionela Elisabeta Staicu, Răzvan Mercuț, Cristian Corneliu Georgescu, Monica Scrieciu, Daniel Vlad, Adrian Camen
International Journal of Molecular Sciences.2023; 24(18): 14345. CrossRef - Analysis of the Degree of Information of Dental Surgeons about Antiresorptive Drugs According to the Time Since Graduation in Dentistry
Flávia Godinho Costa Wanderley Rocha, Roberto Paulo Correia de Araújo
Pesquisa Brasileira em Odontopediatria e Clínica Integrada.2023;[Epub] CrossRef - Safety and Efficacy of Pamidronate in Neonatal Hypercalcemia Caused by Subcutaneous Fat Necrosis: A Case Report
Stefano Martinelli, Marco Pitea, Italo Francesco Gatelli, Tara Raouf, Graziano Barera, Ottavio Vitelli
Frontiers in Pediatrics.2022;[Epub] CrossRef - Zoledronic acid for osteoporosis and associated low-energy fractures
S. S. Rodionova, A. F. Kolondaev, A. N. Torgashin, I. A. Solomyannik
Meditsinskiy sovet = Medical Council.2022; (21): 163. CrossRef
- Risk factors for dental findings of the development of medication-related osteonecrosis of the jaw: Investigation of 3734 teeth in cancer patients receiving high dose antiresorptive agents

- Bone Metabolism
- Long-Term Treatment of Postmenopausal Osteoporosis
- Jacques P. Brown
- Endocrinol Metab. 2021;36(3):544-552. Published online June 22, 2021
- DOI: https://doi.org/10.3803/EnM.2021.301
- 14,432 View
- 918 Download
- 37 Web of Science
- 35 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Osteoporosis is an incurable chronic condition, like heart disease, diabetes, or hypertension. A large gap currently exists in the primary prevention of fractures, and studies show that an estimated 80% to 90% of adults do not receive appropriate osteoporosis management even in the secondary prevention setting. Case finding strategies have been developed and effective pharmacological interventions are available. This publication addresses how best to use the pharmacological options available for postmenopausal osteoporosis to provide lifelong fracture protection in patients at high and very high risk of fracture. The benefit of osteoporosis therapies far outweighs the rare risks.
-
Citations
Citations to this article as recorded by- Effects of stepwise administration of osteoprotegerin and parathyroid hormone-related peptide DNA vectors on bone formation in ovariectomized rat model
Ye Ji Eom, Jang-Woon Kim, Yeri Alice Rim, Jooyoung Lim, Se In Jung, Ji Hyeon Ju
Scientific Reports.2024;[Epub] CrossRef - Glycolithocholic acid increases the frequency of circulating Tregs through constitutive androstane receptor to alleviate postmenopausal osteoporosis
Xiaoyu Cai, Zhi Li, Yao Yao, Yongquan Zheng, Meng Zhang, Yiqing Ye
Biochemical Pharmacology.2024; 219: 115951. CrossRef - Cucumber seed polypeptides regulate RANKL-induced osteoclastogenesis through OPG/RANKL/RANK and NF-κB
Tao Yu, Xiao Liu, Meng Jiang, Yuanyue Li, Heng Su, Ben Niu
In Vitro Cellular & Developmental Biology - Animal.2024; 60(1): 54. CrossRef - Eupatilin ameliorates postmenopausal osteoporosis via elevating microRNA‐211‐5p and repressing JAK2/STAT3 pathway
Liu Hong, Chao Yang
Environmental Toxicology.2024; 39(4): 2218. CrossRef - Strontium-Doped Mesoporous Bioactive Glass-Loading Bisphosphonates Inhibit Osteoclast Differentiation and Prevent Osteoporosis in Ovariectomized Mice
Zhi Zhou, Shicheng Huo, Zhanchun Li
Coatings.2024; 14(1): 97. CrossRef - A novel PDIA3/FTO/USP20 positive feedback regulatory loop induces osteogenic differentiation of preosteoblast in osteoporosis
Fei Zhang, Chen Liu, Zhiyong Chen, Chengyi Zhao
Cell Biology International.2024; 48(4): 541. CrossRef - Research Progress of Zoledronic Acid in the Treatment of Osteoarthritis
保成 刘
Advances in Clinical Medicine.2024; 14(02): 2821. CrossRef - A novel mechanism of Vildagliptin in regulating bone metabolism and mitigating osteoporosis
Jinwen He, Dacheng Zhao, Bo Peng, Xingwen Wang, Shenghong Wang, Xiaobing Zhao, Peng Xu, Bin Geng, Yayi Xia
International Immunopharmacology.2024; 130: 111671. CrossRef - Positive benefit-risk ratio of Psoraleae Fructus: Comprehensive safety assessment and osteogenic effects in rats
Zhuo Shi, Jin-chao Pan, Yi Ru, Ning-ning Shen, Yu-fu Liu, Cheng Zhang, Xiang-jun Wu, Fang-yang Li, Jia-lu Cui, Chun-qi Yang, Jun-ling Yang, Mao-xing Li, Cheng-rong Xiao, Zeng-chun Ma, Chuan Li, Yu-guang Wang, Yue Gao
Journal of Ethnopharmacology.2024; 326: 117967. CrossRef - Function-oriented mechanism discovery of coumarins from Psoralea corylifolia L. in the treatment of ovariectomy-induced osteoporosis based on multi-omics analysis
Qianyi Wei, Yongrong Zhou, Zhengtao Hu, Ye Shi, Qing Ning, Keyun Ren, Xinyu Guo, Ronglin Zhong, Zhi Xia, Yinghao Yin, Yongxin Hu, Yingjie Wei, Ziqi Shi
Journal of Ethnopharmacology.2024; 329: 118130. CrossRef - Efficacy and Possible Mechanisms of Astragali Radix and its Ingredients
in Animal Models of Osteoporosis: A Preclinical Review and Metaanalysis
Ning Cao, Zhangxuan Shou, Yi Xiao, Puqing Liu
Current Drug Targets.2024; 25(2): 135. CrossRef - CircRNA hsa_circ_0006859 inhibits the osteogenic differentiation of BMSCs and aggravates osteoporosis by targeting miR-642b-5p/miR-483-3p and upregulating EFNA2/DOCK3
Peng Yin, Yuan Xue
International Immunopharmacology.2023; 116: 109844. CrossRef - Resveratrol induces proliferation and differentiation of mouse pre-osteoblast MC3T3-E1 by promoting autophagy
Weiye Cai, Bin Sun, Chao Song, Fei Liu, Zhengliang Wu, Zongchao Liu
BMC Complementary Medicine and Therapies.2023;[Epub] CrossRef - Oridonin Attenuates Thioacetamide-Induced Osteoclastogenesis Through MAPK/NF-κB Pathway and Thioacetamide-Inhibited Osteoblastogenesis Through BMP-2/RUNX2 Pathway
XiaoLi Jin, Jia Xu, Fanfan Yang, Jin Chen, Feng Luo, Bin Xu, Jian Xu
Calcified Tissue International.2023; 112(6): 704. CrossRef - Phytochemical Compounds Involved in the Bone Regeneration Process and Their Innovative Administration: A Systematic Review
Alina Hanga-Farcaș, Florina Miere (Groza), Gabriela Adriana Filip, Simona Clichici, Luminita Fritea, Laura Grațiela Vicaș, Eleonora Marian, Annamaria Pallag, Tunde Jurca, Sanda Monica Filip, Mariana Eugenia Muresan
Plants.2023; 12(10): 2055. CrossRef - Screening of superior anti‐osteoporotic flavonoids from Epimedii Folium with dual effects of reversing iron overload and promoting osteogenesis
Jun Jiang, Jinjin He, Shichang Xiao, Jiayi Shenyuan, Tong Chen, Dan Pei
Biomedical Chromatography.2023;[Epub] CrossRef - Study on the Effect of Bushen Zhuanggu Tablet Combined with Conventional Regimen on Bone Mineral Density Improvement, Functional Recovery and Fracture Risk Prevention in Patients with Postmenopausal Osteoporosis
Tianliang Chen, Guilan Li, Yongtao Xu, Min Tang
Computational and Mathematical Methods in Medicine.2023; 2023: 1. CrossRef - Circ_0001825 promotes osteogenic differentiation in human-derived mesenchymal stem cells via miR-1270/SMAD5 axis
Changjun Zheng, Lingzhi Ding, Ziming Xiang, Mingxuan Feng, Fujiang Zhao, Zhaoxin Zhou, Chang She
Journal of Orthopaedic Surgery and Research.2023;[Epub] CrossRef - Identification of ROCK1 as a novel biomarker for postmenopausal osteoporosis and pan-cancer analysis
Bowen Lai, Heng Jiang, Yuan Gao, Xuhui Zhou
Aging.2023; 15(17): 8873. CrossRef - The Mechanotransduction Signaling Pathways in the Regulation of Osteogenesis
Zhaoshuo Liu, Qilin Wang, Junyou Zhang, Sihan Qi, Yingying Duan, Chunyan Li
International Journal of Molecular Sciences.2023; 24(18): 14326. CrossRef - Decoding the mechanism of Eleutheroside E in treating osteoporosis via network pharmacological analysis and molecular docking of osteoclast-related genes and gut microbiota
Tianyu Zhou, Yilin Zhou, Dongdong Ge, Youhong Xie, Jiangyan Wang, Lin Tang, Qunwei Dong, Ping Sun
Frontiers in Endocrinology.2023;[Epub] CrossRef - Epigallocatechin gallate alleviates osteoporosis by regulating the gut microbiota and serum metabolites in rats
Xuebing Han, Yifeng Fu, Keyu Wang, Siying Li, Chang Jiang, Shuangshuang Wang, Zheng Wang, Gang Liu, Siwang Hu
Food & Function.2023; 14(23): 10564. CrossRef - The Molecular Role of Polyamines in Age-Related Diseases: An Update
Guadalupe Elizabeth Jimenez Gutierrez, Fabiola V. Borbolla Jiménez, Luis G. Muñoz, Yessica Sarai Tapia Guerrero, Nadia Mireya Murillo Melo, José Melesio Cristóbal-Luna, Norberto Leyva Garcia, Joaquín Cordero-Martínez, Jonathan J. Magaña
International Journal of Molecular Sciences.2023; 24(22): 16469. CrossRef - Pueraria lobata-derived exosome-like nanovesicles alleviate osteoporosis by enhacning autophagy
Weiqiang Zhan, Mingzhu Deng, Xinqia Huang, Dong Xie, Xiang Gao, Jiaxian Chen, Zhen Shi, Jiaxu Lu, Hao Lin, Peng Li
Journal of Controlled Release.2023; 364: 644. CrossRef - Based on network pharmacology and molecular docking to explore the molecular mechanism of Ginseng and Astragalus decoction against postmenopausal osteoporosis
Wei Fan, Zong-Zhe Jiang, Sheng-Rong Wan
Medicine.2023; 102(46): e35887. CrossRef - Network pharmacology-based pharmacological mechanism prediction of Lycii Fructus against postmenopausal osteoporosis
Jianbo Wang, Yi Wang, Leyan Li, Shuiqi Cai, Dandan Mao, Hongkan Lou, Jian Zhao
Medicine.2023; 102(48): e36292. CrossRef - Benefits of lumican on human bone health: clinical evidence using bone marrow aspirates
Yun Sun Lee, So Jeong Park, Jin Young Lee, Eunah Choi, Beom-Jun Kim
The Korean Journal of Internal Medicine.2022; 37(4): 821. CrossRef - ED-71 inhibited osteoclastogenesis by enhancing EphrinB2–EphB4 signaling between osteoclasts and osteoblasts in osteoporosis
Yuan Zhang, Yuying Kou, Panpan Yang, Xing Rong, Rong Tang, Hongrui Liu, Minqi Li
Cellular Signalling.2022; 96: 110376. CrossRef - Effects of Muscles on Bone Metabolism—with a Focus on Myokines
Beom-Jun Kim
Annals of Geriatric Medicine and Research.2022; 26(2): 63. CrossRef - Evaluation of the tolerability of zoledronic acid preparations for parenteral administration
I. A. Shafieva, S. V. Bulgakova, A. V. Shafieva
Meditsinskiy sovet = Medical Council.2022; (11): 96. CrossRef - Impact of Alendronate Sodium plus Elcatonin on Postoperative Bone Pain in Patients with Osteoporotic Fractures
Baohui Wang, Yindi Sun, Da Shi, Xiuwei Han, Na Liu, Bo Wang, Zhijun Liao
BioMed Research International.2022; 2022: 1. CrossRef - Current use of bone turnover markers in the management of osteoporosis
Jacques P. Brown, Andrew Don-Wauchope, Pierre Douville, Caroline Albert, Samuel D. Vasikaran
Clinical Biochemistry.2022; 109-110: 1. CrossRef - Study on the influence of balloon dilation mode on the intravertebral cleft of osteoporotic fracture
Nanning Lv, Xiaoxiao Feng, Haojun Liu, Xuejun Jia, Shanqin Han, Mingming Liu
BMC Surgery.2022;[Epub] CrossRef - An Acid-Sensitive Bone Targeting Delivery System Carrying Acacetin Prevents Osteoporosis in Ovariectomized Mice
Xiaochen Sun, Chenyu Song, Chenxi Zhang, Chunlei Xing, Juan Lv, Huihui Bian, Nanning Lv, Dagui Chen, Xin Dong, Mingming Liu, Li Su
Pharmaceuticals.2022; 16(1): 2. CrossRef - Changes in Serum Dickkopf-1, RANK Ligand, Osteoprotegerin, and Bone Mineral Density after Allogeneic Hematopoietic Stem Cell Transplantation Treatment
Eunhee Jang, Jeonghoon Ha, Ki-Hyun Baek, Moo Il Kang
Endocrinology and Metabolism.2021; 36(6): 1211. CrossRef
- Effects of stepwise administration of osteoprotegerin and parathyroid hormone-related peptide DNA vectors on bone formation in ovariectomized rat model

- Bone Metabolism
- Update on Denosumab Treatment in Postmenopausal Women with Osteoporosis
- Yong-Ki Min
- Endocrinol Metab. 2015;30(1):19-26. Published online March 27, 2015
- DOI: https://doi.org/10.3803/EnM.2015.30.1.19
- 3,743 View
- 38 Download
- 16 Web of Science
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Denosumab, a fully human recombinant monoclonal antibody to the receptor activator of nuclear factor-κB ligand (RANKL), blocks binding of RANKL to the RANK receptor, found on the surface of osteoclasts and osteoclast precursors, resulting in decreased bone resorption. Subcutaneous denosumab administration once every 6 months increases bone mineral density at the lumbar spine, total hip, and/or femoral neck, and reduces markers of bone turnover significantly in postmenopausal women with osteoporosis. Relative to placebo, denosumab treatment reduces the risk of vertebral, nonvertebral, and hip fractures significantly. The benefits of denosumab treatment are generally obvious after the first dose and were continued for up to 8 years of treatment in an extension study. The tolerability profile of denosumab during this extension phase was consistent with that observed during the initial 3-year FREEDOM trial. Postmarketing safety surveillance has not shown any unexpected findings. Ongoing safety surveillance will more fully define the long-term safety of denosumab. The benefits of denosumab would seem to be greater than its risks. Denosumab is an important choice in the treatment of postmenopausal women with osteoporosis at increased risk of fractures, including older patients who have difficulty with oral bisphosphonate intake and patients who are intolerant of, or unresponsive to, other therapies.
-
Citations
Citations to this article as recorded by- Comparative Pharmacokinetic Study of 5 Active Ingredients after Oral Administration of Zuogui Pill in Osteoporotic Rats with Different Syndrome Types
Jiawei Qiu, Yaoyao Zhu, Jing Xing, Ling Wang, Jianhua Zhang, Hua Yin, Suresh Ponnayyan Sulochana
International Journal of Analytical Chemistry.2023; 2023: 1. CrossRef - Benefits of lumican on human bone health: clinical evidence using bone marrow aspirates
Yun Sun Lee, So Jeong Park, Jin Young Lee, Eunah Choi, Beom-Jun Kim
The Korean Journal of Internal Medicine.2022; 37(4): 821. CrossRef - Lumican Inhibits Osteoclastogenesis and Bone Resorption by Suppressing Akt Activity
Jin-Young Lee, Da-Ae Kim, Eun-Young Kim, Eun-Ju Chang, So-Jeong Park, Beom-Jun Kim
International Journal of Molecular Sciences.2021; 22(9): 4717. CrossRef - Potential Biomarkers to Improve the Prediction of Osteoporotic Fractures
Beom-Jun Kim, Seung Hun Lee, Jung-Min Koh
Endocrinology and Metabolism.2020; 35(1): 55. CrossRef - Effect of bisphosphonate on the prevention of bone loss in patients with gastric cancer after gastrectomy: A randomized controlled trial
Jeonghoon Ha, Jung-Min Lee, Yejee Lim, Mee Kyoung Kim, Hyuk-Sang Kwon, Ki-Ho Song, Hae Myung Jeon, Moo Il Kang, Ki-Hyun Baek
Bone.2020; 130: 115138. CrossRef - Vasomotor Symptoms: More Than Temporary Menopausal Symptoms
Ki-Jin Ryu, Hyuntae Park, Jin Seol Park, Yeon Woo Lee, Soo Young Kim, Hayun Kim, Youngmi Jeong, Yong Jin Kim, Kyong Wook Yi, Jung Ho Shin, Jun Young Hur, Tak Kim
Journal of Menopausal Medicine.2020; 26(3): 147. CrossRef - Does the OPG/RANKL system contribute to the bone-vascular axis in chronic kidney disease? A systematic review
Beata Znorko, Ewa Oksztulska-Kolanek, Małgorzata Michałowska, Tomasz Kamiński, Krystyna Pawlak
Advances in Medical Sciences.2017; 62(1): 52. CrossRef - Conservative management of osteoporotic vertebral fractures: an update
A. Slavici, M. Rauschmann, C. Fleege
European Journal of Trauma and Emergency Surgery.2017; 43(1): 19. CrossRef - Denosumab and alendronate treatment in patients with back pain due to fresh osteoporotic vertebral fractures
Tomoko Tetsunaga, Tomonori Tetsunaga, Keiichiro Nishida, Masato Tanaka, Yoshihisa Sugimoto, Tomoyuki Takigawa, Yoshitaka Takei, Toshifumi Ozaki
Journal of Orthopaedic Science.2017; 22(2): 230. CrossRef - Safety and efficacy of denosumab in osteoporotic hemodialysed patients
Francescaromana Festuccia, Maryam Tayefeh Jafari, Alessandra Moioli, Claudia Fofi, Simona Barberi, Stefano Amendola, Salvatore Sciacchitano, Giorgio Punzo, Paolo Menè
Journal of Nephrology.2017; 30(2): 271. CrossRef - Simultaneous bilateral atypical femoral fracture in a patient receiving denosumab: case report and literature review
J. Selga, J. H. Nuñez, J. Minguell, M. Lalanza, M. Garrido
Osteoporosis International.2016; 27(2): 827. CrossRef - Vasomotor symptoms and osteoporosis in Korean postmenopausal women
Ki-Jin Ryu, Hyun-Tae Park, Yong Jin Kim, Kyong Wook Yi, Jung Ho Shin, Jun Young Hur, Tak Kim
Maturitas.2016; 87: 27. CrossRef - Osteoporosis: A Therapeutic Update
Patricia A. Mackey, Michael D. Whitaker
The Journal for Nurse Practitioners.2015; 11(10): 1011. CrossRef - Sulfonylurea: Personalized Medicine for Type 2 Diabetes
You-Cheol Hwang
Endocrinology and Metabolism.2015; 30(4): 467. CrossRef - A Systematic Review of Bone Anti-Resorptive Treatment Toxicity in Innate and Adaptive Immunity Cells: Osteonecrosis of the Jaws and Future Implications
Athanassios Kyrgidis, Maria Yavropoulou, Ioannis Tilaveridis, Charalambos Andreadis, Konstantinos Antoniades, Dimitrios Kouvelas
The Journal of Dentists.2015; 3(2): 50. CrossRef
- Comparative Pharmacokinetic Study of 5 Active Ingredients after Oral Administration of Zuogui Pill in Osteoporotic Rats with Different Syndrome Types


 KES
KES

 First
First Prev
Prev



