Search
- Page Path
- HOME > Search
- Diabetes, obesity and metabolism
- Coronary Artery Calcium Score as a Sensitive Indicator of Cardiovascular Disease in Patients with Type 2 Diabetes Mellitus: A Long-Term Cohort Study
- Dae-Jeong Koo, Mi Yeon Lee, Sun Joon Moon, Hyemi Kwon, Sang Min Lee, Se Eun Park, Cheol-Young Park, Won-Young Lee, Ki Won Oh, Sung Rae Cho, Young-Hoon Jeong, Eun-Jung Rhee
- Endocrinol Metab. 2023;38(5):568-577. Published online October 10, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1770

- 1,506 View
- 112 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Coronary artery calcium score (CACS) has become an important tool for evaluating cardiovascular disease (CVD). This study evaluated the significance of CACS for future CVD through more than 10 years of follow-up in asymptomatic Korean populations with type 2 diabetes mellitus (T2DM) known to have a relatively low CACS burden.
Methods
We enrolled 981 asymptomatic T2DM patients without CVD at baseline who underwent CACS evaluation using multidetector computed tomography between January 2008 and December 2014. They were grouped into five predefined CACS categories based on Agatston scores and followed up by August 2020. The primary endpoint was incident CVD events, including coronary, cerebrovascular, and peripheral arterial disease.
Results
The relative risk of CVD was significantly higher in patients with CACS ≥10, and the significance persisted after adjustment for known confounders. A higher CACS category indicated a higher incidence of future CVD: hazard ratio (95% confidence interval) 4.09 (1.79 to 9.36), 12.00 (5.61 to 25.69), and 38.79 (16.43 to 91.59) for 10≤ CACS <100, 100≤ CACS <400, and CACS ≥400, respectively. During the 12-year follow-up period, the difference in event-free survival more than doubled as the category increased. Patients with CACS below 10 had very low CVD incidence throughout the follow-up. The receiver operating characteristic analysis showed better area under curve when the CACS cutoff was 10 than 100.
Conclusion
CACS can be a sensitive marker of CVD risk. Specifically, CACS above 10 is an indicator of CVD high-risk requiring more intensive medical treatment in Koreans with T2DM.

- Calcium & bone metabolism
- Age-Dependent Association of Height Loss with Incident Fracture Risk in Postmenopausal Korean Women
- Chaewon Lee, Hye-Sun Park, Yumie Rhee, Namki Hong
- Endocrinol Metab. 2023;38(6):669-678. Published online September 1, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1734
- 1,470 View
- 86 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Height loss is a simple clinical measure associated with increased fracture risk. However, limited data exists on the association between height loss and fracture risk in postmenopausal Korean women. It is unknown whether this association varies with age.
Methods
Data on height loss over a 6-year period were collected from a community-based longitudinal follow-up cohort (Ansung cohort of the Korean Genome and Epidemiology Study). Incident fractures were defined based on self-reported fractures after excluding those due to severe trauma or toes/fingers. The association between incident fractures and height loss was investigated using a Cox proportional hazards model.
Results
During a median follow-up of 10 years after the second visit, 259/1,806 participants (median age, 64 years) experienced incident fractures. Overall, a 1 standard deviation (SD) decrease in height (1.6 cm/median 5.8 years) was associated with 9% increased risk of fracture (hazard ratio [HR], 1.09; P=0.037), which lost statistical significance after adjustment for covariates. When stratified into age groups (50–59, 60–69, 70 years or older), a 1 SD decrease in height remained a robust predictor of fracture in the 50 to 59 years age group after adjusting for covariates (adjusted hazard ratio [aHR], 1.52; P=0.003), whereas height loss was not an independent predictor of fracture in the 60 to 69 (aHR, 1.06; P=0.333) or the 70 years or older age groups (aHR, 1.05; P=0.700; P for interaction <0.05, for all).
Conclusion
Height loss during the previous 6 years was associated with an increased 10-year fracture risk in postmenopausal women in their 50s.

- Diabetes, Obesity and Metabolism
- Sleep Duration and the Risk of Type 2 Diabetes: A Community-Based Cohort Study with a 16-Year Follow-up
- Da Young Lee, Inha Jung, So Young Park, Ji Hee Yu, Ji A Seo, Kyeong Jin Kim, Nam Hoon Kim, Hye Jin Yoo, Sin Gon Kim, Kyung Mook Choi, Sei Hyun Baik, Seung Ku Lee, Chol Shin, Nan Hee Kim
- Endocrinol Metab. 2023;38(1):146-155. Published online February 6, 2023
- DOI: https://doi.org/10.3803/EnM.2022.1582
- 2,587 View
- 164 Download
- 5 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
We aimed to investigate the moderating effects of obesity, age, and sex on the association between sleep duration and the development of diabetes in Asians.
Methods
We analyzed data from a cohort of the Korean Genome and Epidemiology Study conducted from 2001 to 2020. After excluding shift workers and those with diabetes at baseline, 7,407 participants were stratified into three groups according to sleep duration: ≤5 hours/night, >5 to 7 hours/night (reference), and >7 hours/night. The Cox proportional hazards analyses were used to calculate the hazard ratios (HRs) and 95% confidence intervals (CIs) for incident type 2 diabetes mellitus (T2DM). Subgroup analyses were performed according to obesity, age, and sex.
Results
During 16 years of follow-up, 2,024 cases of T2DM were identified. Individuals who slept ≤5 h/night had a higher risk of incident diabetes than the reference group (HR, 1.17; 95% CI, 1.02 to 1.33). The subgroup analysis observed a valid interaction with sleep duration only for obesity. A higher risk of T2DM was observed in the ≤5 hours/night group in non-obese individuals, men, and those aged <60 years, and in the >7 hours/night group in obese individuals (HRs were 1.34 [95% CI, 1.11 to 1.61], 1.22 [95% CI, 1 to 1.49], and 1.18 [95% CI, 1.01 to 1.39], respectively).
Conclusion
This study confirmed the effect of sleep deprivation on the risk of T2DM throughout the 16-year follow-up period. This impact was confined to non-obese or young individuals and men. We observed a significant interaction between sleep duration and obesity. -
Citations
Citations to this article as recorded by- Attention to Innate Circadian Rhythm and the Impact of Its Disruption on Diabetes
Da Young Lee, Inha Jung, So Young Park, Ji Hee Yu, Ji A Seo, Kyeong Jin Kim, Nam Hoon Kim, Hye Jin Yoo, Sin Gon Kim, Kyung Mook Choi, Sei Hyun Baik, Nan Hee Kim
Diabetes & Metabolism Journal.2024; 48(1): 37. CrossRef - Role of Sleep and Sleep Disorders in Cardiometabolic Risk: a Review and Update
Shaden O. Qasrawi, Ahmed S. BaHammam
Current Sleep Medicine Reports.2024; 10(1): 34. CrossRef - Evaluating reliability in wearable devices for sleep staging
Vera Birrer, Mohamed Elgendi, Olivier Lambercy, Carlo Menon
npj Digital Medicine.2024;[Epub] CrossRef - All That Glitters Is Not Gold: The Same Sleep Time, but Different Diabetogenic Outcomes
Bohye Kim, Obin Kwon
Endocrinology and Metabolism.2023; 38(1): 78. CrossRef - The Link Between Sleeping and Type 2 Diabetes: A Systematic Review
Ali Darraj
Cureus.2023;[Epub] CrossRef
- Attention to Innate Circadian Rhythm and the Impact of Its Disruption on Diabetes

- Diabetes, Obesity and Metabolism
Big Data Articles (National Health Insurance Service Database) - Metformin and Cervical Cancer Risk in Patients with Newly Diagnosed Type 2 Diabetes: A Population-Based Study in Korea
- Hyun Min Kim, Min Jin Kang, Sun Ok Song
- Endocrinol Metab. 2022;37(6):929-937. Published online December 26, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1613
- Correction in: Endocrinol Metab 2023;38(1):174
- 2,430 View
- 217 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Cervical cancer is a prevalent malignancy that is a major health problem for women worldwide. The cancer-preventive properties of metformin are well-known, but insufficient data have been reported regarding its relationship to cervical cancer. Therefore, in a nationwide population-based study, we investigated the association between metformin use and cervical cancer incidence in patients with newly diagnosed type 2 diabetes.
Methods
This retrospective cohort study used the Korean National Health Insurance claims database. Individuals newly diagnosed with type 2 diabetes between January 2005 and December 2009 were included. The occurrence of cervical cancer was explored by matching for age, economic status, region of residence, and use of anti-diabetic medication.
Results
In total, 66,013 metformin users and 64,756 non-users were analyzed. Cervical cancer occurred in 219 metformin users (0.33%) and 274 metformin non-users (0.42%) (hazard ratio [HR], 0.783; 95% confidence interval [CI], 0.655 to 0.036; P=0.007). Moreover, cervical cancer risk was considerably reduced in those treated with a high dose (>1,200,000 mg) or for an extended period (≥2,000 days) compared to non-users (HR, 0.151; 95% CI, 0.093 to 0.243; P<0.001; and HR, 0.141; 95% CI, 0.077 to 0.258; P<0.001). The incidence was also significantly lower in metformin users among those over 50 years old (HR, 0.791; 95% CI, 0.650 to 0.961; P<0.001).
Conclusion
Metformin use in patients with newly diagnosed diabetes was associated with a lower risk of cervical cancer in Korea. Furthermore, a significant association was found between the use of metformin and cervical cancer in a dose- and duration-dependent manner and among those over 50 years old. -
Citations
Citations to this article as recorded by- Repurposing of Chronically Used Drugs in Cancer Therapy: A Chance to Grasp
Mohamad Ali Hijazi, André Gessner, Nahed El-Najjar
Cancers.2023; 15(12): 3199. CrossRef - Network-based drug repurposing for HPV-associated cervical cancer
Faheem Ahmed, Young Jin Yang, Anupama Samantasinghar, Young Woo Kim, Jeong Beom Ko, Kyung Hyun Choi
Computational and Structural Biotechnology Journal.2023; 21: 5186. CrossRef - The Use of Metformin and Postoperative Insulin Pump Were Predictive Factors for Outcomes of Diabetic Colorectal Cancer Patients after Surgery
Xu-Rui Liu, Fei Liu, Zi-Wei Li, Quan Lv, Xin-Peng Shu, Lian-Shuo Li, Yue Tong, Wei Zhang, Dong Peng
Nutrition and Cancer.2023; 75(10): 1926. CrossRef
- Repurposing of Chronically Used Drugs in Cancer Therapy: A Chance to Grasp

- Diabetes, Obesity and Metabolism
Big Data Articles (National Health Insurance Service Database) - Risk and Risk Factors for Postpartum Type 2 Diabetes Mellitus in Women with Gestational Diabetes: A Korean Nationwide Cohort Study
- Mi Jin Choi, Jimi Choi, Chae Weon Chung
- Endocrinol Metab. 2022;37(1):112-123. Published online February 28, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1276

- 4,073 View
- 171 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
There are differences in risk and risk factor findings of postpartum type 2 diabetes mellitus (T2DM) after gestational diabetes depending on study design and subjects of previous studies. This study aimed to assess these risk and risk factors more accurately through a population-based study to provide basic data for prevention strategies.
Methods
This open retrospective cohort included data of 419,101 women with gestational diabetes and matched 1,228,802 control women who delivered between 2004 and 2016 from the South Korea National Health Information Database of the National Health Insurance Service. Following 14 (median 5.9) years of follow-up, the incidence and hazard ratio (HR) of postpartum T2DM were evaluated using Kaplan-Meier curves and Cox proportional regression models.
Results
The incidence and HR of postpartum T2DM in women with gestational diabetes (compared to women without gestational diabetes) after the 14-year follow-up was 21.3% and 2.78 (95% confidence interval [CI], 2.74 to 2.82), respectively. Comorbid obesity (body mass index [BMI] ≥25 kg/m2) increased postpartum T2DM risk 7.59 times (95% CI, 7.33 to 7.86). Significant risk factors for postpartum T2DM were fasting glucose level, BMI, age, family history of diabetes, hypertension, and insulin use during pregnancy.
Conclusion
This population-based study showed higher postpartum T2DM risk in women with gestational diabetes than in those without, which was further increased by comorbid obesity. BMI and fasting glucose level were important postpartum risk factors. The management of obesity and glycemic control may be important strategies to prevent the incidence of diabetes after delivery. -
Citations
Citations to this article as recorded by- Antenatal factors and risk of postpartum hyperglycemia in women with gestational diabetes mellitus: A central India prospective cohort study
Nilajkumar Bagde, Madhuri Bagde, Vijayalakshmi Shanbhag, Pragati Trigunait, Nagma Sheikh, Sarita Agrawal
Journal of Family Medicine and Primary Care.2024; 13(1): 59. CrossRef - Integration of nutrigenomics, melatonin, serotonin and inflammatory cytokines in the pathophysiology of pregnancy-specific urinary incontinence in women with gestational diabetes mellitus
Danielle Cristina Honorio França, Eduardo Luzía França, Luis Sobrevia, Angélica Mércia Pascon Barbosa, Adenilda Cristina Honorio-França, Marilza Vieira Cunha Rudge
Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease.2023; 1869(6): 166737. CrossRef - Risk factors associated with early postpartum glucose intolerance in women with a history of gestational diabetes mellitus: a systematic review and meta-analysis
Zhe Liu, Qianghuizi Zhang, Leyang Liu, Weiwei Liu
Endocrine.2023; 82(3): 498. CrossRef
- Antenatal factors and risk of postpartum hyperglycemia in women with gestational diabetes mellitus: A central India prospective cohort study

- Diabetes, Obesity and Metabolism
Big Data Articles (National Health Insurance Service Database) - Risk of Diabetes in Subjects with Positive Fecal Immunochemical Test: A Nationwide Population-Based Study
- Kwang Woo Kim, Hyun Jung Lee, Kyungdo Han, Jung Min Moon, Seung Wook Hong, Eun Ae Kang, Jooyoung Lee, Hosim Soh, Seong-Joon Koh, Jong Pil Im, Joo Sung Kim
- Endocrinol Metab. 2021;36(5):1069-1077. Published online October 28, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1119
- 3,611 View
- 97 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Positive fecal immunochemical test (FIT) results have been recently suggested as a risk factor for systemic inflammation. Diabetes induces inflammation in the gastrointestinal tract via several ways. We investigated the association between FIT results and the incidence of diabetes.
Methods
A total of 7,946,393 individuals aged ≥50 years from the National Cancer Screening Program database who underwent FIT for colorectal cancer (CRC) screening from 2009 to 2012 were enrolled. The primary outcome was newly diagnosed diabetes based on the International Classification of Disease 10th revision codes and administration of anti-diabetic medication during the follow-up period.
Results
During a mean follow-up of 6.5 years, the incidence rates of diabetes were 11.97, 13.60, 14.53, and 16.82 per 1,000 personyears in the FIT negative, one-positive, two-positive, and three-positive groups, respectively. The hazard ratios (HRs) for the incidence of diabetes were 1.14 (95% confidence interval [CI], 1.12 to 1.16; HR, 1.21; 95% CI, 1.16 to 1.27; and HR, 1.40; 95% CI, 1.28 to 1.55) in the one-positive, two-positive, and three-positive FIT groups compared with the FIT negative group, respectively. The effect was consistent in individuals with normal fasting blood glucose (adjusted HR 1.55 vs. 1.14, P for interaction <0.001).
Conclusion
Positive FIT results were associated with a significantly higher risk of diabetes, suggesting that the FIT can play a role not only as a CRC screening tool, but also as a surrogate marker of systemic inflammation; thus, increasing the diabetes risk. -
Citations
Citations to this article as recorded by- Uncovering a dose-response relationship between positive fecal immunochemical test (FIT) and all-cause, cardiovascular and cancer-related mortality
Chi Pang Wen, Min Kuang Tsai, June Han Lee, Hung Yi Chiou, Christopher Wen, Ta-Wei David Chu, Chien Hua Chen
European Journal of Internal Medicine.2024; 120: 69. CrossRef - Faecal haemoglobin concentrations are associated with all-cause mortality and cause of death in colorectal cancer screening
Lasse Kaalby, Ulrik Deding, Issam Al-Najami, Gabriele Berg-Beckhoff, Thomas Bjørsum-Meyer, Tinne Laurberg, Aasma Shaukat, Robert J. C. Steele, Anastasios Koulaouzidis, Morten Rasmussen, Morten Kobaek-Larsen, Gunnar Baatrup
BMC Medicine.2023;[Epub] CrossRef - Positive Results from the Fecal Immunochemical Test Can Be Related to Dementia: A Nationwide Population-Based Study in South Korea
Yu Kyung Jun, Seung Woo Lee, Kwang Woo Kim, Jung Min Moon, Seong-Joon Koh, Hyun Jung Lee, Joo Sung Kim, Kyungdo Han, Jong Pil Im
Journal of Alzheimer's Disease.2023; 91(4): 1515. CrossRef - Faecal Haemoglobin Estimated by Faecal Immunochemical Tests—An Indicator of Systemic Inflammation with Real Clinical Potential
Karen N. Barnett, Gavin R. C. Clark, Robert J. C. Steele, Callum G. Fraser
Diagnostics.2021; 11(11): 2093. CrossRef
- Uncovering a dose-response relationship between positive fecal immunochemical test (FIT) and all-cause, cardiovascular and cancer-related mortality

- Diabetes, Obesity and Metabolism
- Changes in Insulin Resistance Index and the Risk of Liver Fibrosis in Patients with Nonalcoholic Fatty Liver Disease without Diabetes: Kangbuk Samsung Health Study
- Dae-Jeong Koo, Mi Yeon Lee, Inha Jung, Sun Joon Moon, Hyemi Kwon, Se Eun Park, Eun-Jung Rhee, Won-Young Lee
- Endocrinol Metab. 2021;36(5):1016-1028. Published online October 21, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1110
- 4,130 View
- 128 Download
- 5 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
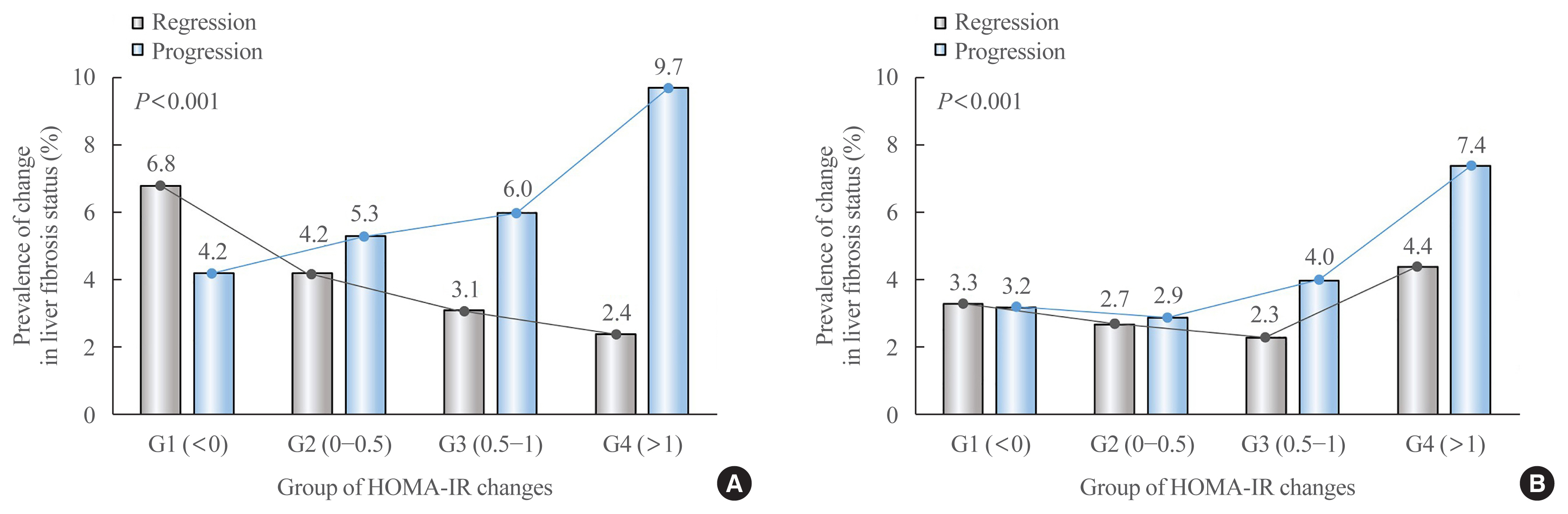
Fibrosis is the most important prognostic factor for nonalcoholic fatty liver disease (NAFLD). Insulin resistance plays a key role of fibrosis progression. We evaluated the association between changes in homeostasis model assessment of insulin resistance (HOMA-IR) values and changes in fibrosis status in NAFLD.
Methods
We analyzed the data of 15,728 participants with NAFLD (86% men, mean age 40.5 years) who had no diabetes at baseline and visited our centers for health check-ups both in 2012 and 2016. The participants were classified into four groups according to the degree of change in HOMA-IR values from baseline to the end of follow-up: G1 (<0), G2 (0–0.50), G3 (0.51–1.00), and G4 (>1.00). NAFLD was assessed by ultrasonography, and fibrosis status was evaluated by the NAFLD fibrosis score (NFS) and the aspartate aminotransferase to platelet ratio index (APRI).
Results
After the 4-year follow-up, the multivariable-adjusted odds ratio (OR) for progression of fibrosis probability increased with increasing HOMA-IR values (OR, 2.25; 95% confidence interval [CI], 1.87 to 2.71 for NFS; and OR, 2.55; 95% CI, 2.05 to 3.18 for APRI, G4). This tendency remained consistent throughout the subgroup analyses, except in those for female sex and a body mass index <25 kg/m2. The OR for regression of fibrosis probability decreased with increasing HOMA-IR values (OR, 0.33; 95% CI, 0.25 to 0.43 for NFS, G4).
Conclusion
Changes in HOMA-IR values were associated with changes in fibrosis status in patients with NAFLD without diabetes, which underscores the role of insulin resistance in liver fibrosis. -
Citations
Citations to this article as recorded by- Insulin Resistance/Sensitivity Measures as Screening Indicators of Metabolic-Associated Fatty Liver Disease and Liver Fibrosis
Mohammad E. Khamseh, Mojtaba Malek, Soodeh Jahangiri, Sohrab Nobarani, Azita Hekmatdoost, Marieh Salavatizadeh, Samira Soltanieh, Haleh Chehrehgosha, Hoda Taheri, Zeinab Montazeri, Fereshteh Attaran, Faramarz Ismail-Beigi, Fariba Alaei-Shahmiri
Digestive Diseases and Sciences.2024; 69(4): 1430. CrossRef - Association between nonalcoholic fatty liver disease and left ventricular diastolic dysfunction: A 7-year retrospective cohort study of 3,496 adults using serial echocardiography
Gyuri Kim, Tae Yang Yu, Jae Hwan Jee, Ji Cheol Bae, Mira Kang, Jae Hyeon Kim
Diabetes & Metabolism.2024; : 101534. CrossRef - Factors Associated with Liver Fibrosis in Chinese Patients with Type 2 Diabetes Mellitus and Non-Alcoholic Fatty Liver Disease
Yu Luo, Cuiyu Wang, Tian Zhang, Xiaoyu He, Jianan Hao, Andong Shen, Hang Zhao, Shuchun Chen, Luping Ren
International Journal of General Medicine.2023; Volume 16: 293. CrossRef - Impact of COVID-19 Lockdown on Non-Alcoholic Fatty Liver Disease and Insulin Resistance in Adults: A before and after Pandemic Lockdown Longitudinal Study
Ángel Arturo López-González, Bárbara Altisench Jané, Luis Masmiquel Comas, Sebastiana Arroyo Bote, Hilda María González San Miguel, José Ignacio Ramírez Manent
Nutrients.2022; 14(14): 2795. CrossRef - Metabolic Score for Insulin Resistance Is Inversely Related to Incident Advanced Liver Fibrosis in Patients with Non-Alcoholic Fatty Liver Disease
Jun-Hyuk Lee, Yu-Jin Kwon, Kyongmin Park, Hye Sun Lee, Hoon-Ki Park, Jee Hye Han, Sang Bong Ahn
Nutrients.2022; 14(15): 3039. CrossRef - Machine learning models including insulin resistance indexes for predicting liver stiffness in United States population: Data from NHANES
Kexing Han, Kexuan Tan, Jiapei Shen, Yuting Gu, Zilong Wang, Jiayu He, Luyang Kang, Weijie Sun, Long Gao, Yufeng Gao
Frontiers in Public Health.2022;[Epub] CrossRef - The crosstalk between insulin resistance and nonalcoholic fatty liver disease/metabolic dysfunction-associated fatty liver disease: a culprit or a consequence?
Dae-Jeong Koo, Won-Young Lee
Cardiovascular Prevention and Pharmacotherapy.2022; 4(4): 132. CrossRef
- Insulin Resistance/Sensitivity Measures as Screening Indicators of Metabolic-Associated Fatty Liver Disease and Liver Fibrosis

- Clinical Study
- Protocol for a Korean Multicenter Prospective Cohort Study of Active Surveillance or Surgery (KoMPASS) in Papillary Thyroid Microcarcinoma
- Min Ji Jeon, Yea Eun Kang, Jae Hoon Moon, Dong Jun Lim, Chang Yoon Lee, Yong Sang Lee, Sun Wook Kim, Min-Hee Kim, Bo Hyun Kim, Ho-Cheol Kang, Minho Shong, Sun Wook Cho, Won Bae Kim
- Endocrinol Metab. 2021;36(2):359-364. Published online March 23, 2021
- DOI: https://doi.org/10.3803/EnM.2020.890
- Correction in: Endocrinol Metab 2022;37(1):181
- 5,781 View
- 201 Download
- 14 Web of Science
- 17 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
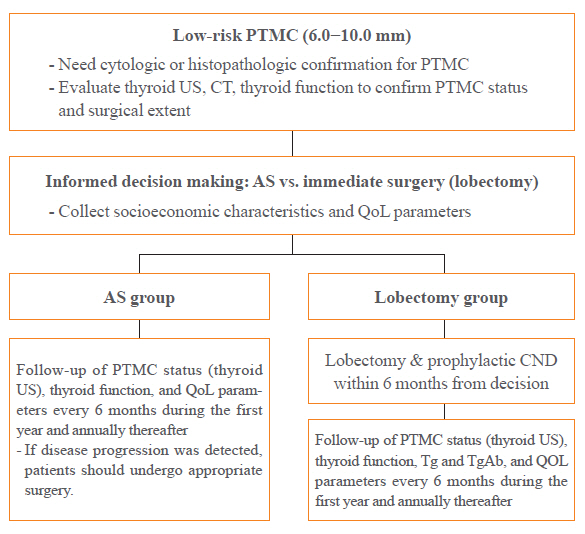
A Korean Multicenter Prospective cohort study of Active Surveillance or Surgery (KoMPASS) for papillary thyroid microcarcinomas (PTMCs) has been initiated. The aim is to compare clinical outcomes between active surveillance (AS) and an immediate lobectomy for low-risk PTMCs. We here outline the detailed protocol for this study.
Methods
Adult patients with a cytopathologically confirmed PTMC sized 6.0 to 10.0 mm by ultrasound (US) will be included. Patients will be excluded if they have a suspicious extra-thyroidal extension or metastasis of a PTMC or multiple thyroid nodules or other thyroid diseases which require a total thyroidectomy. Printed material describing the prognosis of PTMCs, and the pros and cons of each management option, will be provided to eligible patients to select their preferred intervention. For the AS group, thyroid US, thyroid function, and quality of life (QoL) parameters will be monitored every 6 months during the first year, and then annually thereafter. Disease progression will be defined as a ≥3 mm increase in maximal diameter of a PTMC, or the development of new thyroid cancers or metastases. If progression is detected, patients should undergo appropriate surgery. For the lobectomy group, a lobectomy with prophylactic central neck dissection will be done within 6 months. After initial surgery, thyroid US, thyroid function, serum thyroglobulin (Tg), anti-Tg antibody, and QoL parameters will be monitored every 6 months during the first year and annually thereafter. Disease progression will be defined in these cases as the development of new thyroid cancers or metastases.
Conclusion
KoMPASS findings will help to confirm the role of AS, and develop individualized management strategies, for low-risk PTMCs. -
Citations
Citations to this article as recorded by- Active Surveillance for Low-Risk Thyroid Cancers: A Review of Current Practice Guidelines
Min Joo Kim, Jae Hoon Moon, Eun Kyung Lee, Young Shin Song, Kyong Yeun Jung, Ji Ye Lee, Ji-hoon Kim, Kyungsik Kim, Sue K. Park, Young Joo Park
Endocrinology and Metabolism.2024; 39(1): 47. CrossRef - It Is Time to Understand the Additional Benefits of Active Surveillance for Low-Risk Papillary Thyroid Carcinoma
Kyeong Jin Kim
Endocrinology and Metabolism.2024; 39(1): 95. CrossRef - Active Surveillance for Low-Risk Papillary Thyroid Carcinoma as an Acceptable Management Option with Additional Benefits: A Comprehensive Systematic Review
Jee Hee Yoon, Wonsuk Choi, Ji Yong Park, A Ram Hong, Hee Kyung Kim, Ho-Cheol Kang
Endocrinology and Metabolism.2024; 39(1): 152. CrossRef - Active Surveillance for Low-Risk Papillary Thyroid Carcinoma as an Acceptable Management Option with Additional Benefits: A Comprehensive Systematic Review
Jee Hee Yoon, Wonsuk Choi, Ji Yong Park, A Ram Hong, Hee Kyung Kim, Ho-Cheol Kang
Endocrinology and Metabolism.2024; 39(1): 152. CrossRef - Thyroid‐Stimulating Hormone, Age, and Tumor Size are Risk Factors for Progression During Active Surveillance of Low‐Risk Papillary Thyroid Microcarcinoma in Adults
Yasuhiro Ito, Akira Miyauchi, Makoto Fujishima, Takuya Noda, Tsutomu Sano, Takahiro Sasaki, Taketoshi Kishi, Tomohiko Nakamura
World Journal of Surgery.2023; 47(2): 392. CrossRef - Thyroid FNA cytology: The Eastern versus Western perspectives
Mitsuyoshi Hirokawa, Manon Auger, Chan Kwon Jung, Fabiano Mesquita Callegari
Cancer Cytopathology.2023; 131(7): 415. CrossRef - To Screen or Not to Screen?
Do Joon Park
Endocrinology and Metabolism.2023; 38(1): 69. CrossRef - Lower Thyroid Cancer Mortality in Patients Detected by Screening: A Meta-Analysis
Shinje Moon, Young Shin Song, Kyong Yeun Jung, Eun Kyung Lee, Young Joo Park
Endocrinology and Metabolism.2023; 38(1): 93. CrossRef - Long-Term Outcomes of Active Surveillance and Immediate Surgery for Adult Patients with Low-Risk Papillary Thyroid Microcarcinoma: 30-Year Experience
Akira Miyauchi, Yasuhiro Ito, Makoto Fujishima, Akihiro Miya, Naoyoshi Onoda, Minoru Kihara, Takuya Higashiyama, Hiroo Masuoka, Shiori Kawano, Takahiro Sasaki, Mitsushige Nishikawa, Shuji Fukata, Takashi Akamizu, Mitsuru Ito, Eijun Nishihara, Mako Hisakad
Thyroid®.2023; 33(7): 817. CrossRef - Active Surveillance Outcomes of Patients with Low-Risk Papillary Thyroid Microcarcinoma According to Levothyroxine Treatment Status
Masashi Yamamoto, Akira Miyauchi, Yasuhiro Ito, Makoto Fujishima, Takahiro Sasaki, Takumi Kudo
Thyroid®.2023; 33(10): 1182. CrossRef - Cost-Effectiveness of Active Surveillance Compared to Early Surgery of Small Papillary Thyroid Cancer: A Retrospective Study on a Korean Population
Han-Sang Baek, Jeonghoon Ha, Kwangsoon Kim, Jaseong Bae, Jeong Soo Kim, Sungju Kim, Dong-Jun Lim, Chulmin Kim
Journal of Korean Medical Science.2023;[Epub] CrossRef - Optimal Cutoff Values of the Contact Angle of Tumor on Sonography System for Predicting Extrathyroidal Extension of Papillary Thyroid Carcinoma by Tumor Location
Ik Beom Shin, Do Hoon Koo, Dong Sik Bae
Clinical Medicine Insights: Oncology.2023;[Epub] CrossRef - Thermal ablation for papillary thyroid microcarcinoma located in the isthmus: a study with 3 years of follow-up
Lin Zheng, Fang-yi Liu, Jie Yu, Zhi-gang Cheng, Xiao-ling Yu, Xiao-cong Dong, Zhi-yu Han, Ping Liang
Future Oncology.2022; 18(4): 471. CrossRef - Trends in the Management of Localized Papillary Thyroid Carcinoma in the United States (2000–2018)
Elisa Pasqual, Julie Ann Sosa, Yingxi Chen, Sara J. Schonfeld, Amy Berrington de González, Cari M. Kitahara
Thyroid.2022; 32(4): 397. CrossRef - Management of Low-Risk Thyroid Cancers: Is Active Surveillance a Valid Option? A Systematic Review of the Literature
Renato Patrone, Nunzio Velotti, Stefania Masone, Alessandra Conzo, Luigi Flagiello, Chiara Cacciatore, Marco Filardo, Vincenza Granata, Francesco Izzo, Domenico Testa, Stefano Avenia, Alessandro Sanguinetti, Andrea Polistena, Giovanni Conzo
Journal of Clinical Medicine.2021; 10(16): 3569. CrossRef - Cost-Effectiveness Analysis of Active Surveillance Compared to Early Surgery in Small Papillary Thyroid Cancer: A Systemic Review
Han-sang Baek, Chai-ho Jeong, Jeonghoon Ha, Ja-Seong Bae, Jeong-soo Kim, Dong-Jun Lim, Chul-Min Kim
Cancer Management and Research.2021; Volume 13: 6721. CrossRef - Active Surveillance as an Effective Management Option for Low-Risk Papillary Thyroid Microcarcinoma
Min Ji Jeon, Won Gu Kim, Tae Yong Kim, Young Kee Shong, Won Bae Kim
Endocrinology and Metabolism.2021; 36(4): 717. CrossRef
- Active Surveillance for Low-Risk Thyroid Cancers: A Review of Current Practice Guidelines

- Clinical Study
- Identification of Novel Genetic Variants Related to Trabecular Bone Score in Community-Dwelling Older Adults
- Sung Hye Kong, Ji Won Yoon, Jung Hee Kim, JooYong Park, Jiyeob Choi, Ji Hyun Lee, A Ram Hong, Nam H. Cho, Chan Soo Shin
- Endocrinol Metab. 2020;35(4):801-810. Published online November 24, 2020
- DOI: https://doi.org/10.3803/EnM.2020.735
- 4,602 View
- 112 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
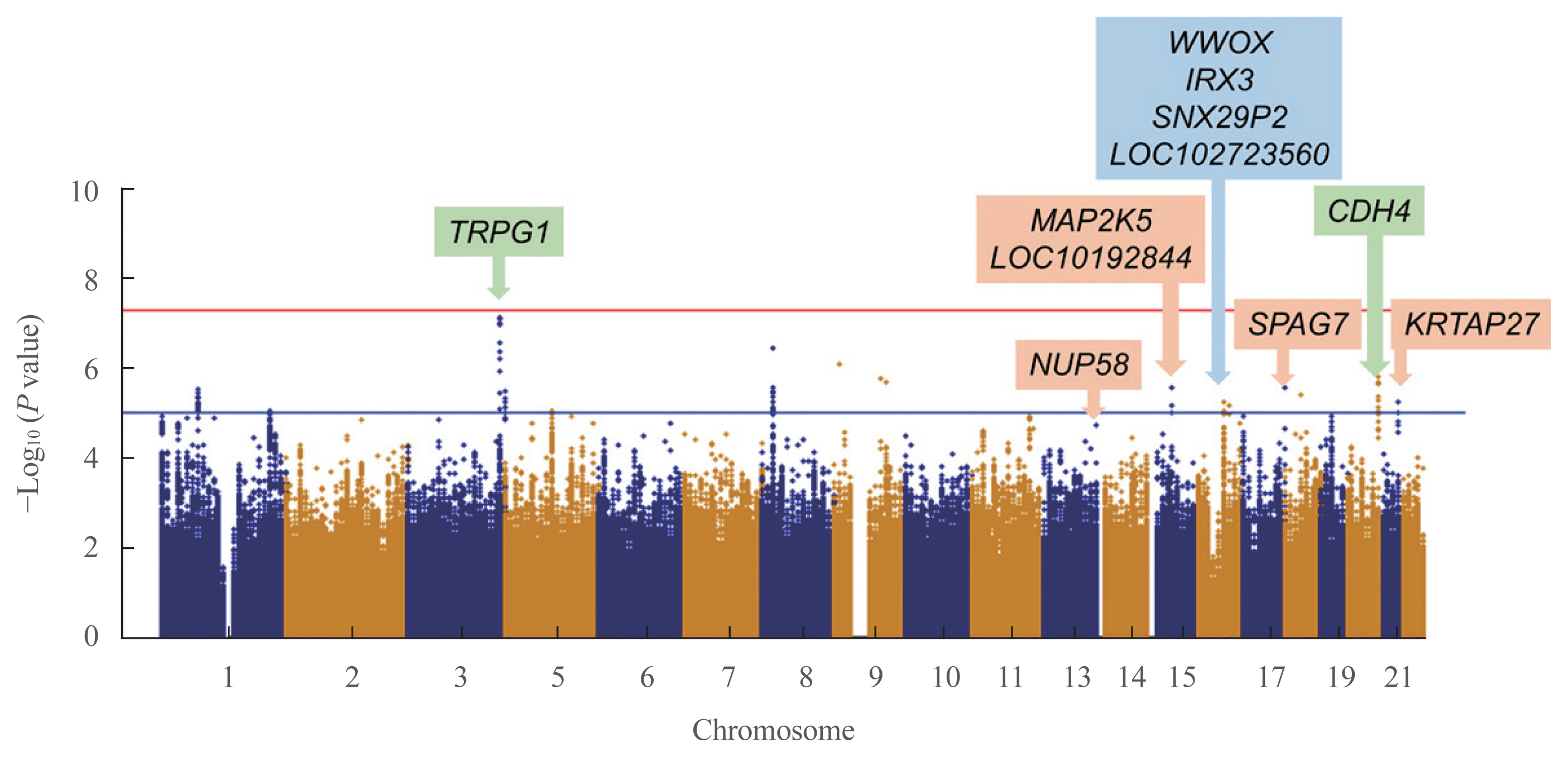
As the genetic variants of trabecular bone microarchitecture are not well-understood, we performed a genome-wide association study to identify genetic determinants of bone microarchitecture analyzed by trabecular bone score (TBS).
Methods
TBS-associated genes were discovered in the Ansung cohort (discovery cohort), a community-based rural cohort in Korea, and then validated in the Gene-Environment Interaction and Phenotype (GENIE) cohort (validation cohort), consisting of subjects who underwent health check-up programs. In the discovery cohort, 2,451 participants were investigated for 1.42 million genotyped and imputed markers.
Results
In the validation cohort, identified as significant variants were evaluated in 2,733 participants. An intronic variant in iroquois homeobox 3 (IRX3), rs1815994, was significantly associated with TBS in men (P=3.74E-05 in the discovery cohort, P=0.027 in the validation cohort). Another intronic variant in mitogen-activated protein kinase kinase 5 (MAP2K5), rs11630730, was significantly associated with TBS in women (P=3.05E-09 in the discovery cohort, P=0.041 in the validation cohort). Men with the rs1815994 variant and women with the rs11630730 variant had lower TBS and lumbar spine bone mineral density. The detrimental effects of the rs1815994 variant in men and rs11630730 variant in women were also identified in association analysis (β=–0.0281, β=–0.0465, respectively).
Conclusion
In this study, the rs1815994 near IRX3 in men and rs11630730 near MAP2K5 in women were associated with deterioration of the bone microarchitecture. It is the first study to determine the association of genetic variants with TBS. Further studies are needed to confirm our findings and identify additional variants contributing to the trabecular bone microarchitecture.

- Obesity and Metabolism
- Optimal Waist Circumference Cutoff Values for the Diagnosis of Abdominal Obesity in Korean Adults
- Yeong Sook Yoon, Sang Woo Oh
- Endocrinol Metab. 2014;29(4):418-426. Published online December 29, 2014
- DOI: https://doi.org/10.3803/EnM.2014.29.4.418
- 5,832 View
- 69 Download
- 65 Web of Science
- 70 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Abdominal obesity is associated closely with insulin resistance, diabetes, and cardiovascular disease. Waist circumference (WC) is a useful surrogate marker commonly used for abdominal adiposity. The determination of WC cutoff levels is important in the prevention and treatment of obesity, type 2 diabetes, and related cardiovascular diseases. Recent epidemiological evidence suggested that appropriate optimal cutoffs for Koreans ranged over 80 to 89.8 cm in males and 76.1 to 86.5 cm in females. We analyzed the data from two large cohorts using receiver operating characteristic curve analysis with the incidences of diabetes, hypertension, dyslipidemia, cerebrovascular disease, myocardial infarct, angina, coronary artery disease, and multiple metabolic risk factors as outcome variables. Optimal WC cutoff points for Koreans were 85 cm in males and 80 cm in females. However, considering the prevalence of abdominal obesity and the health costs for its prevention and management, 90 cm in males and 85 cm in females are probably more appropriate thresholds for abdominal obesity. These values may be modified once better research is performed through prospective studies using representative populations, common health outcomes, and proper analytical approaches.
-
Citations
Citations to this article as recorded by- The prevalence and factors associated with sarcopenia in Thai older adults: A systematic review and meta-analysis
Phatcharaphon Whaikid, Noppawan Piaseu
International Journal of Nursing Sciences.2024; 11(1): 31. CrossRef - Machine learning analysis for the association between breast feeding and metabolic syndrome in women
Jue Seong Lee, Eun-Saem Choi, Hwasun Lee, Serhim Son, Kwang-Sig Lee, Ki Hoon Ahn
Scientific Reports.2024;[Epub] CrossRef - Association between waist circumference change after smoking cessation and incidence of hypertension in Korean adults
H.J. Lee, J.W. Choi
Public Health.2024; 229: 73. CrossRef - Waist circumference and end‐stage renal disease based on glycaemic status: National Health Insurance Service data 2009–2018
Yun Kyung Cho, Ji Hye Huh, Shinje Moon, Yoon Jung Kim, Yang‐Hyun Kim, Kyung‐do Han, Jun Goo Kang, Seong Jin Lee, Sung‐Hee Ihm
Journal of Cachexia, Sarcopenia and Muscle.2023; 14(1): 585. CrossRef - Simple anthropometric measures to predict visceral adipose tissue area in middle-aged Indonesian men
Sahat Basana Romanti Ezer Matondang, Bennadi Adiandrian, Komang Shary Karismaputri, Cicilia Marcella, Joedo Prihartono, Dicky Levenus Tahapary, Yosuke Yamada
PLOS ONE.2023; 18(1): e0280033. CrossRef - Sleep Quality in Women with Premenstrual Syndrome Is Associated with Metabolic Syndrome-Related Variables
Hyejin Chun, Miae Doo
Healthcare.2023; 11(10): 1492. CrossRef - Gender, Age and Clinical Characteristics of Older Adults with High-Risk of Obstructive Sleep Apnea Assessed by the STOP-Bang Questionnaire
Gyu Lee Kim, Yun Jin Kim, Jeong Gyu Lee, Yu Hyeon Yi, Young Jin Tak, Seung Hun Lee, Young Jin Ra, Sang Yeoup Lee, Young Hye Cho, Eun Ju Park, Youngin Lee, Jung In Choi, Sae Rom Lee, Ryuk Jun Kwon, Soo Min Son
Korean Journal of Clinical Geriatrics.2023; 24(2): 72. CrossRef - Body Composition and Cardiovascular Risk: A Study of Polish Military Flying Personnel
Agata Gaździńska, Stefan Gaździński, Paweł Jagielski, Paweł Kler
Metabolites.2023; 13(10): 1102. CrossRef - Associated Factors with Changes of Metabolic Abnormalities among General Population in COVID-19 Pandemic
Eunjoo Kwon, Eun-Hee Nah, Suyoung Kim, Seon Cho, Hyeran Park
Korean Journal of Health Promotion.2023; 23(2): 55. CrossRef - Effects of Pharmacoacupuncture for Obesity: A Systematic Review and Meta-Analysis
Seyun Kim, Mi-Yeon Song, Won-Seok Chung, Hyungsuk Kim, Woo-Chul Shin, Junhyuk Kang, Joonwon Seo, Sangwoo Seo, Seung Ho Yu, Jung-Hyun Lim, Su-Hwan Ji, Jae-Heung Cho
Journal of Korean Medicine for Obesity Research.2023; 23(2): 112. CrossRef - Associations Between Elevated Growth Differentiation Factor-15 and Sarcopenia Among Community-dwelling Older Adults
Miji Kim, Jeremy D Walston, Chang Won Won, Anne B Newman
The Journals of Gerontology: Series A.2022; 77(4): 770. CrossRef - The association of obesity with thyroid carcinoma risk
Xiao‐Ni Ma, Cheng‐Xu Ma, Li‐Jie Hou, Song‐Bo Fu
Cancer Medicine.2022; 11(4): 1136. CrossRef - A Longitudinal Retrospective Observational Study on Obesity Indicators and the Risk of Impaired Fasting Glucose in Pre- and Postmenopausal Women
Myung Ji Nam, Hyunjin Kim, Yeon Joo Choi, Kyung-Hwan Cho, Seon Mee Kim, Yong-Kyun Roh, Kyungdo Han, Jin-Hyung Jung, Yong-Gyu Park, Joo-Hyun Park, Do-Hoon Kim
Journal of Clinical Medicine.2022; 11(10): 2795. CrossRef - Association of Metabolic Health and Central Obesity with the Risk of Thyroid Cancer: Data from the Korean Genome and Epidemiology Study
Dung N. Nguyen, Jin Hee Kim, Mi Kyung Kim
Cancer Epidemiology, Biomarkers & Prevention.2022; 31(3): 543. CrossRef - Interaction of polygenic variants specific for abdominal obesity risk with energy metabolism in large Korean cohorts
Sunmin Park
Nutrition Bulletin.2022; 47(3): 307. CrossRef - Effects of Oral Health Behavior and Mental Health on Metabolic Syndrome in Korean Adults
Jin-Ah Jung, Hye-Won Cheon, Sang-Eun Moon, Sun-Hwa Hong
Journal of Dental Hygiene Science.2022; 22(2): 90. CrossRef - Relation of Dietary n-3 and n-6 Fatty Acid Intakes to Metabolic Syndrome in Middle-Aged People Depending on the Level of HbA1c: A Review of National Health and Nutrition Survey Data from 2014 to 2016
Seo-Woo Park, Do-Yeong Kim, Gyeong-Tae Bak, Dae-Sung Hyun, Sung-Kyung Kim
Medicina.2022; 58(8): 1017. CrossRef - Synergistic Interaction between Hyperuricemia and Abdominal Obesity as a Risk Factor for Metabolic Syndrome Components in Korean Population
Min Jin Lee, Ah Reum Khang, Yang Ho Kang, Mi Sook Yun, Dongwon Yi
Diabetes & Metabolism Journal.2022; 46(5): 756. CrossRef - Risk of Carotid Atherosclerosis in Subjects with Prediabetes Overlapping Metabolic Syndrome
Seol A Jang, Kyoung Min Kim, Seok Won Park, Chul Sik Kim
Metabolic Syndrome and Related Disorders.2022; 20(10): 599. CrossRef - Association of high body mass index, waist circumference, and body fat percentage with sarcopenia in older women
Myung Chul Yoo, Chang Won Won, Yunsoo Soh
BMC Geriatrics.2022;[Epub] CrossRef - Relationship between low skeletal muscle mass, sarcopenic obesity and left ventricular diastolic dysfunction in Korean adults
Jee Hee Yoo, Sung Woon Park, Ji Eun Jun, Sang‐Man Jin, Kyu Yeon Hur, Moon‐Kyu Lee, Mira Kang, Gyuri Kim, Jae Hyeon Kim
Diabetes/Metabolism Research and Reviews.2021;[Epub] CrossRef - Association of Early-Life Mental Health With Biomarkers in Midlife and Premature Mortality
George B. Ploubidis, G. David Batty, Praveetha Patalay, David Bann, Alissa Goodman
JAMA Psychiatry.2021; 78(1): 38. CrossRef - A clinical evaluation of noninvasive and contactless radiofrequency technique in the treatment of abdominal fat
Jie Qin, Meng‐er Guo, Xue‐gang Xu, Chao Zhang, Cheng‐qian Yu, Yuan‐hong Li, Hong‐duo Chen
Journal of Cosmetic Dermatology.2021; 20(9): 2765. CrossRef - Exercise training and burdock root (Arctium lappa L.) extract independently improve abdominal obesity and sex hormones in elderly women with metabolic syndrome
Min-Seong Ha, Jang Soo Yook, Minchul Lee, Kazuya Suwabe, Woo-Min Jeong, Jae-Jun Kwak, Hideaki Soya
Scientific Reports.2021;[Epub] CrossRef - Effect of body mass index and abdominal obesity on mortality after percutaneous coronary intervention: a nationwide, population-based study
Woo-Hyuk Song, Eun Hui Bae, Jeong Cheon Ahn, Tae Ryom Oh, Yong-Hyun Kim, Jin Seok Kim, Sun-Won Kim, Soo Wan Kim, Kyung-Do Han, Sang-Yup Lim
The Korean Journal of Internal Medicine.2021; 36(Suppl 1): S90. CrossRef - Individual and Synergistic Relationships of Low Muscle Mass and Low Muscle Function with Depressive Symptoms in Korean Older Adults
Youngyun Jin, Seamon Kang, Hyunsik Kang
International Journal of Environmental Research and Public Health.2021; 18(19): 10129. CrossRef - Association between Metabolic Syndrome and the Number of Remaining Teeth in Postmenopausal Women: A Cross-Sectional Analysis Using the Korean National Health and Nutritional Examination Survey
Jeong-In Kim, Choong-Ho Choi, Ki-Ho Chung
Journal of Clinical Medicine.2021; 10(20): 4759. CrossRef - No Association between Metabolic Syndrome and Periodontitis in Korean Postmenopausal Women
Jeong-In Kim, Choong-Ho Choi, Ki-Ho Chung
International Journal of Environmental Research and Public Health.2021; 18(21): 11110. CrossRef - Relative Lean Body Mass and Waist Circumference for the Identification of Metabolic Syndrome in the Korean General Population
Eunjoo Kwon, Eun-Hee Nah, Suyoung Kim, Seon Cho
International Journal of Environmental Research and Public Health.2021; 18(24): 13186. CrossRef - SVM-based waist circumference estimation using Kinect
Dasom Seo, Euncheol Kang, Yu-mi Kim, Sun-Young Kim, Il-Seok Oh, Min-Gul Kim
Computer Methods and Programs in Biomedicine.2020; 191: 105418. CrossRef - Effects of abdominal obesity on the association between air pollution and kidney function
Su-Min Jeong, Jin-Ho Park, Hyun-Jin Kim, Hyuktae Kwon, Seo Eun Hwang
International Journal of Obesity.2020; 44(7): 1568. CrossRef - Effect of sarcopenic obesity on deterioration of physical function in the elderly
Hyun Ho Kong, Chang Won Won, Won Kim
Archives of Gerontology and Geriatrics.2020; 89: 104065. CrossRef - Effects of low skeletal muscle mass and sarcopenic obesity on albuminuria: a 7-year longitudinal study
Jee Hee Yoo, Gyuri Kim, Sung Woon Park, Min Sun Choi, Jiyeon Ahn, Sang-Man Jin, Kyu Yeon Hur, Moon-Kyu Lee, Mira Kang, Jae Hyeon Kim
Scientific Reports.2020;[Epub] CrossRef A Novel Indicator of Children’s Lipid Accumulation Product Associated with Impaired Fasting Glucose in Chinese Children and Adolescents
Yongting Yuan, Hong Xie, Lili Sun, Bangxuan Wang, Li Zhang, Hui Han, Rongying Yao, Yehuan Sun, Lianguo Fu
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 1653. CrossRef- The Association between the Ratio of Energy Intake to Basal Metabolic Rate and Physical Activity to Sarcopenia: Using the Korea National Health and Nutrition Examination Surveys (2008–2011)
Yu Jin Cho, Mi Hee Cho, Bomi Han, Minji Park, Seolah Bak, Minseon Park
Korean Journal of Family Medicine.2020; 41(3): 167. CrossRef - Waist circumference as a vital sign in clinical practice: a Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity
Robert Ross, Ian J. Neeland, Shizuya Yamashita, Iris Shai, Jaap Seidell, Paolo Magni, Raul D. Santos, Benoit Arsenault, Ada Cuevas, Frank B. Hu, Bruce A. Griffin, Alberto Zambon, Philip Barter, Jean-Charles Fruchart, Robert H. Eckel, Yuji Matsuzawa, Jean-
Nature Reviews Endocrinology.2020; 16(3): 177. CrossRef - Lung function as a predictor of incident type 2 diabetes in community-dwelling adults: A longitudinal finding over 12 years from the Korean Genome and Epidemiology Study
J.H. Lee, H.S. Lee, Y.J. Lee
Diabetes & Metabolism.2020; 46(5): 392. CrossRef - Sex- and age-specific effects of energy intake and physical activity on sarcopenia
Yu Jin Cho, Youn-Hee Lim, Jae Moon Yun, Hyung-Jin Yoon, Minseon Park
Scientific Reports.2020;[Epub] CrossRef - Protective effect of smoking cessation on subsequent myocardial infarction and ischemic stroke independent of weight gain: A nationwide cohort study
Jung-Hwan Cho, Hye-Mi Kwon, Se-Eun Park, Jin-Hyung Jung, Kyung-Do Han, Yong-Gyu Park, Yang-Hyun Kim, Eun-Jung Rhee, Won-Young Lee, Michael Cummings
PLOS ONE.2020; 15(7): e0235276. CrossRef - Optimal Cutoff Values for Anthropometric Adiposity Measures of Sri Lankan Adult Women
Nirmala Rathnayake, Gayani Alwis, Janaka Lenora, Sarath Lekamwasam
Journal of Obesity.2020; 2020: 1. CrossRef Differences in the Association Among the Vitamin D Concentration, Dietary Macronutrient Consumption, and Metabolic Syndrome Depending on Pre- and Postmenopausal Status in Korean Women: A Cross-Sectional Study
Hyejin Chun, Gi Dae Kim, Miae Doo
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 3601. CrossRef- Patterns of change in cardiovascular risks of Korean male workers: a 10-year cohort analysis using the National Health Insurance Service–National Sample Cohort (NHIS-NSC) 2.0 database
Hosihn Ryu, Jiyeon Jung, Jihyun Moon
BMJ Open.2020; 10(11): e038446. CrossRef - Predictive Performance of Glycated Hemoglobin for Incident Diabetes Compared with Glucose Tolerance Test According to Central Obesity
Suji Yoo, Jaehoon Jung, Hosu Kim, Kyoung Young Kim, Soo Kyoung Kim, Jungwha Jung, Jong Ryeal Hahm, Jong Ha Baek
Endocrinology and Metabolism.2020; 35(4): 873. CrossRef - Metabolic Syndrome and Risk of Lung Cancer: An Analysis of Korean National Health Insurance Corporation Database
Sooim Sin, Chang-Hoon Lee, Sun Mi Choi, Kyung-Do Han, Jinwoo Lee
The Journal of Clinical Endocrinology & Metabolism.2020; 105(11): e4102. CrossRef - Association of body mass index with bladder cancer risk in men depends on abdominal obesity
Jin Bong Choi, Jung Ho Kim, Sung-Hoo Hong, Kyung-Do Han, U-Syn Ha
World Journal of Urology.2019; 37(11): 2393. CrossRef - Lower Leg Fat Depots Are Associated with Albuminuria Independently of Obesity, Insulin Resistance, and Metabolic Syndrome (Korea National Health and Nutrition Examination Surveys 2008 to 2011)
Eugene Han, Nan Hee Cho, Mi Kyung Kim, Hye Soon Kim
Diabetes & Metabolism Journal.2019; 43(4): 461. CrossRef - The Risk of Myocardial Infarction and Ischemic Stroke According to Waist Circumference in 21,749,261 Korean Adults: A Nationwide Population-Based Study
Jung-Hwan Cho, Eun-Jung Rhee, Se-Eun Park, Hyemi Kwon, Jin-Hyung Jung, Kyung-Do Han, Yong-Gyu Park, Hye Soon Park, Yang-Hyun Kim, Soon-Jib Yoo, Won-Young Lee
Diabetes & Metabolism Journal.2019; 43(2): 206. CrossRef - Association between Serum Gamma-Glutamyltransferase and Prevalence of Metabolic Syndrome Using Data from the Korean Genome and Epidemiology Study
Mi Young Lee, Dae Sung Hyon, Ji Hye Huh, Hae Kyung Kim, Sul Ki Han, Jang Young Kim, Sang Baek Koh
Endocrinology and Metabolism.2019; 34(4): 390. CrossRef - The Association between Obesity Phenotypes and Early Renal Function Decline in Adults without Hypertension, Dyslipidemia, and Diabetes
Jung In Choi, Young Hye Cho, Sang Yeoup Lee, Dong Wook Jeong, Jeong Gyu Lee, Yu Hyeon Yi, Young Jin Tak, Seung Hun Lee, Hye Rim Hwang, Eun Ju Park
Korean Journal of Family Medicine.2019; 40(3): 176. CrossRef - Sex differences in the association between asthma incidence and modifiable risk factors in Korean middle-aged and older adults: NHIS-HEALS 10-year cohort
Susan Park, Sun-Young Jung, Jin-Won Kwon
BMC Pulmonary Medicine.2019;[Epub] CrossRef - Plasma sphingomyelins increase in pre-diabetic Korean men with abdominal obesity
Seung-Soon Im, Hyeon Young Park, Jong Cheol Shon, In-Sung Chung, Ho Chan Cho, Kwang-Hyeon Liu, Dae-Kyu Song, Kyoung Heon Kim
PLOS ONE.2019; 14(3): e0213285. CrossRef - Estimating the Cutoff Points of Time-Dependent Risk Factors by Using Joint Modeling of Longitudinal and Time-to-Event Data: A 14-Year Follow-up Study—Tehran Lipid and Glucose Study
Nezhat Shakeri, Fereidoun Azizi
Asia Pacific Journal of Public Health.2019; 31(8): 728. CrossRef - Metabolic Obesity Phenotypes and Thyroid Cancer Risk: A Cohort Study
Hyemi Kwon, Yoosoo Chang, Ara Cho, Jiin Ahn, Se Eun Park, Cheol-Young Park, Won-Young Lee, Ki-Won Oh, Sung-Woo Park, Hocheol Shin, Seungho Ryu, Eun-Jung Rhee
Thyroid.2019; 29(3): 349. CrossRef - Trends and Cut-Point Changes in Obesity Parameters by Age Groups Considering Metabolic Syndrome
Hyung Jun Park, Young Ho Hong, Yun Jung Cho, Ji Eun Lee, Jae Moon Yun, Hyuktae Kwon, Sang Hyuck Kim
Journal of Korean Medical Science.2018;[Epub] CrossRef - Difference in prostate cancer incidence around sixty years: effects of age and metabolic diseases
Jin Bong Choi, Jung Ho Kim, Sung‐Hoo Hong, Kyung‐Do Han, U‐Syn Ha
Cancer Medicine.2018; 7(6): 2736. CrossRef - The Association of Low Back Pain with Obesity and Abdominal Obesity among Koreans Aged 50 Years or More
Eun Young Choi
Korean Journal of Health Promotion.2018; 18(3): 119. CrossRef - Association between oral health and colorectal adenoma in a screening population
Donghyoun Lee, Kyung Uk Jung, Hyung Ook Kim, Hungdai Kim, Ho-Kyung Chun
Medicine.2018; 97(37): e12244. CrossRef - An association of metabolic syndrome and chronic kidney disease from a 10-year prospective cohort study
Ji Hye Huh, Dhananjay Yadav, Jae Seok Kim, Jung-Woo Son, Eunhee Choi, Seong Hwan Kim, Chol Shin, Ki-Chul Sung, Jang Young Kim
Metabolism.2017; 67: 54. CrossRef - Anatomic fat depots and cardiovascular risk: a focus on the leg fat using nationwide surveys (KNHANES 2008–2011)
Eugene Han, Yong-ho Lee, Byung-Wan Lee, Eun Seok Kang, In-Kyu Lee, Bong-Soo Cha
Cardiovascular Diabetology.2017;[Epub] CrossRef - Association between Body Weight Changes and Menstrual Irregularity: The Korea National Health and Nutrition Examination Survey 2010 to 2012
Kyung Min Ko, Kyungdo Han, Youn Jee Chung, Kun-Ho Yoon, Yong Gyu Park, Seung-Hwan Lee
Endocrinology and Metabolism.2017; 32(2): 248. CrossRef - Low muscle mass and risk of type 2 diabetes in middle-aged and older adults: findings from the KoGES
Jang Won Son, Seong Su Lee, Sung Rae Kim, Soon Jib Yoo, Bong Yun Cha, Ho Young Son, Nam H. Cho
Diabetologia.2017; 60(5): 865. CrossRef - Safety and efficacy of a non-contact radiofrequency device for body contouring in Asians
Dong Hye Suh, Chang Min Kim, Sang Jun Lee, Hyunjoo Kim, Suk Keu Yeom, Hwa Jung Ryu
Journal of Cosmetic and Laser Therapy.2017; 19(2): 89. CrossRef - Arterial stiffness and its association with clustering of metabolic syndrome risk factors
Wanda R. P. Lopes-Vicente, Sara Rodrigues, Felipe X. Cepeda, Camila Paixão Jordão, Valéria Costa-Hong, Akothirene C. B. Dutra-Marques, Jefferson C. Carvalho, Maria Janieire N. N. Alves, Luiz A. Bortolotto, Ivani C. Trombetta
Diabetology & Metabolic Syndrome.2017;[Epub] CrossRef - Associations of sitting time and occupation with metabolic syndrome in South Korean adults: a cross-sectional study
Jin Young Nam, Juyoung Kim, Kyung Hee Cho, Young Choi, Jaewoo Choi, Jaeyong Shin, Eun-Cheol Park
BMC Public Health.2016;[Epub] CrossRef - Associations of Obesity and Dyslipidemia with Intake of Sodium, Fat, and Sugar among Koreans: a Qualitative Systematic Review
Yoon Jung Kang, Hye Won Wang, Se Young Cheon, Hwa Jung Lee, Kyung Mi Hwang, Hae Seong Yoon
Clinical Nutrition Research.2016; 5(4): 290. CrossRef - Articles in 'Endocrinology and Metabolism' in 2014
Won-Young Lee
Endocrinology and Metabolism.2015; 30(1): 47. CrossRef - Ambient Temperature and Prevalence of Obesity: A Nationwide Population-Based Study in Korea
Hae Kyung Yang, Kyungdo Han, Jae-Hyoung Cho, Kun-Ho Yoon, Bong-Yun Cha, Seung-Hwan Lee, David Meyre
PLOS ONE.2015; 10(11): e0141724. CrossRef - Acupoint Catgut Embedding for Obesity: Systematic Review and Meta-Analysis
Taipin Guo, Yulan Ren, Jun Kou, Jing Shi, Sun Tianxiao, Fanrong Liang
Evidence-Based Complementary and Alternative Medicine.2015; 2015: 1. CrossRef - Elderly men over 65 years of age with late-onset hypogonadism benefit as much from testosterone treatment as do younger men
Farid Saad, Aksam Yassin, Ahmad Haider, Gheorghe Doros, Louis Gooren
Korean Journal of Urology.2015; 56(4): 310. CrossRef - Administration of Hwang-Ryun-Haedok-tang, a Herbal Complex, for Patients With Abdominal Obesity: A Case Series
Seungwon Kwon, WooSang Jung, A Ri Byun, SangKwan Moon, KiHo Cho, KyoungHo Shin
EXPLORE.2015; 11(5): 401. CrossRef
- The prevalence and factors associated with sarcopenia in Thai older adults: A systematic review and meta-analysis


 KES
KES

 First
First Prev
Prev



