Search
- Page Path
- HOME > Search
- Thyroid
Big Data Articles (National Health Insurance Service Database) - Prevalence, Treatment Status, and Comorbidities of Hyperthyroidism in Korea from 2003 to 2018: A Nationwide Population Study
- Hwa Young Ahn, Sun Wook Cho, Mi Young Lee, Young Joo Park, Bon Seok Koo, Hang-Seok Chang, Ka Hee Yi
- Endocrinol Metab. 2023;38(4):436-444. Published online July 12, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1684
- 1,791 View
- 126 Download
- 1 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
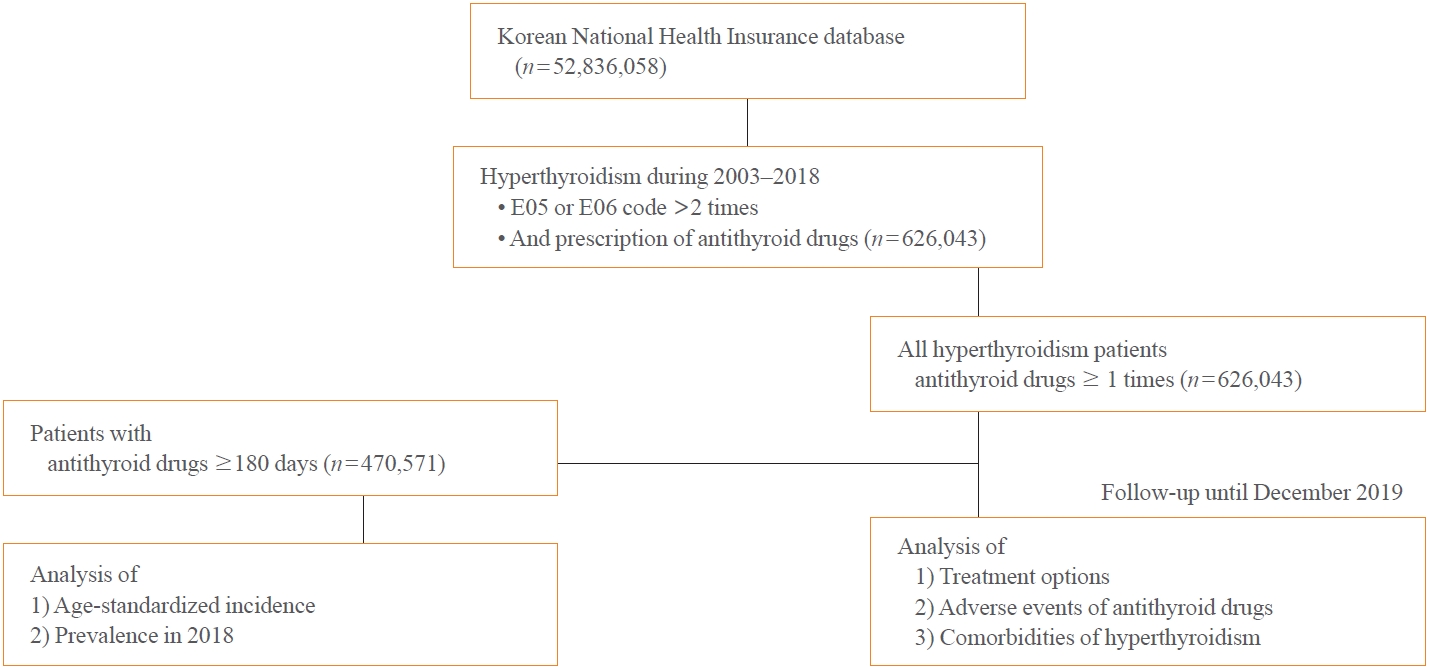
This study aimed to investigate the changes of incidence and treatment of choice for hyperthyroidism from 2003 to 2018 and explore the treatment-related complications and concomitant comorbidities in South Korea using data from the National Health Insurance Service.
Methods
This is a retrospective observational study. Hyperthyroidism was defined as a case having two or more diagnostic codes of thyrotoxicosis, with antithyroid drug intake for more than 6 months.
Results
The average age-standardized incidence of hyperthyroidism from 2003 to 2018 was 42.23 and 105.13 per 100,000 men and women, respectively. In 2003 to 2004, hyperthyroidism was most often diagnosed in patients in their 50s, but in 2017 to 2018, people were most often diagnosed in their 60s. During the entire period, about 93.7% of hyperthyroidism patients were prescribed with antithyroid drugs, and meanwhile, the annual rates of ablation therapy decrease from 7.68% in 2008 to 4.56% in 2018. Antithyroid drug-related adverse events, mainly agranulocytosis and acute hepatitis, as well as complications of hyperthyroidism such as atrial fibrillation or flutter, osteoporosis, and fractures, occurred more often in younger patients.
Conclusion
In Korea, hyperthyroidism occurred about 2.5 times more in women than in men, and antithyroid drugs were most preferred as the first-line treatment. Compared to the general population, hyperthyroid patients may have a higher risk of atrial fibrillation or flutter, osteoporosis, and fractures at a younger age. -
Citations
Citations to this article as recorded by- Long-term effect of thyrotropin-binding inhibitor immunoglobulin on atrial fibrillation in euthyroid patients
Jung-Chi Hsu, Kang-Chih Fan, Ting-Chuan Wang, Shu-Lin Chuang, Ying-Ting Chao, Ting-Tse Lin, Kuan-Chih Huang, Lian-Yu Lin, Lung-Chun Lin
Endocrine Practice.2024;[Epub] CrossRef - The Current Status of Hyperthyroidism in Korea
Hyemi Kwon
Endocrinology and Metabolism.2023; 38(4): 392. CrossRef - Is Thyroid Dysfunction Associated with Unruptured Intracranial Aneurysms? A Population-Based, Nested Case–Control Study from Korea
Hyeree Park, Sun Wook Cho, Sung Ho Lee, Kangmin Kim, Hyun-Seung Kang, Jeong Eun Kim, Aesun Shin, Won-Sang Cho
Thyroid®.2023; 33(12): 1483. CrossRef
- Long-term effect of thyrotropin-binding inhibitor immunoglobulin on atrial fibrillation in euthyroid patients

- Thyroid
- The Early Changes in Thyroid-Stimulating Immunoglobulin Bioassay over Anti-Thyroid Drug Treatment Could Predict Prognosis of Graves’ Disease
- Jin Yu, Han-Sang Baek, Chaiho Jeong, Kwanhoon Jo, Jeongmin Lee, Jeonghoon Ha, Min Hee Kim, Jungmin Lee, Dong-Jun Lim
- Endocrinol Metab. 2023;38(3):338-346. Published online June 9, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1664
- 1,716 View
- 101 Download
- 1 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
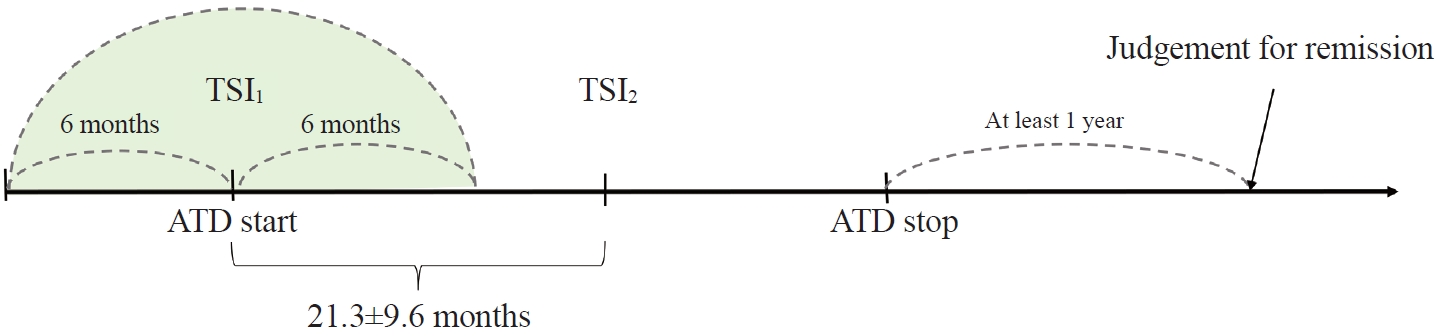
To determine whether baseline thyroid-stimulating immunoglobulin (TSI) bioassay or its early response upon treatment with an anti-thyroid drug (ATD) can predict prognosis of Graves’ disease (GD) in real-world practice.
Methods
This retrospective study enrolled GD patients who had previous ATD treatment with TSI bioassay checked at baseline and at follow-up from April 2010 to November 2019 in one referral hospital. The study population were divided into two groups: patients who experienced relapse or continued ATD (relapse/persistence), and patients who experienced no relapse after ATD discontinuation (remission). The slope and area under the curve at 1st year (AUC1yr) of thyroid-stimulating hormone receptor antibodies including TSI bioassay and thyrotropin-binding inhibitory immunoglobulin (TBII) were calculated as differences between baseline and second values divided by time duration (year).
Results
Among enrolled 156 study subjects, 74 (47.4%) had relapse/persistence. Baseline TSI bioassay values did not show significant differences between the two groups. However, the relapse/persistence group showed less decremental TSI bioassay in response to ATD than the remission group (–84.7 [TSI slope, –198.2 to 8.2] vs. –120.1 [TSI slope, –204.4 to –45.9], P=0.026), whereas the TBII slope was not significantly different between the two groups. The relapse/persistence group showed higher AUC1yr of TSI bioassay and TBII in the 1st year during ATD treatment than the remission group (AUC1yr for TSI bioassay, P=0.0125; AUC1yr for TBII,P =0.001).
Conclusion
Early changes in TSI bioassay can better predict prognosis of GD than TBII. Measurement of TSI bioassay at beginning and follow-up could help predict GD prognosis. -
Citations
Citations to this article as recorded by- Enhanced predictive validity of integrative models for refractory hyperthyroidism considering baseline and early therapy characteristics: a prospective cohort study
Xinpan Wang, Tiantian Li, Yue Li, Qiuyi Wang, Yun Cai, Zhixiao Wang, Yun Shi, Tao Yang, Xuqin Zheng
Journal of Translational Medicine.2024;[Epub] CrossRef - Long-term effect of thyrotropin-binding inhibitor immunoglobulin on atrial fibrillation in euthyroid patients
Jung-Chi Hsu, Kang-Chih Fan, Ting-Chuan Wang, Shu-Lin Chuang, Ying-Ting Chao, Ting-Tse Lin, Kuan-Chih Huang, Lian-Yu Lin, Lung-Chun Lin
Endocrine Practice.2024;[Epub] CrossRef
- Enhanced predictive validity of integrative models for refractory hyperthyroidism considering baseline and early therapy characteristics: a prospective cohort study

- Thyroid
Big Data Articles (National Health Insurance Service Database) - Graves’ Disease and the Risk of End-Stage Renal Disease: A Korean Population-Based Study
- Yoon Young Cho, Bongseong Kim, Dong Wook Shin, Hye Ryoun Jang, Bo-Yeon Kim, Chan-Hee Jung, Jae Hyeon Kim, Sun Wook Kim, Jae Hoon Chung, Kyungdo Han, Tae Hyuk Kim
- Endocrinol Metab. 2022;37(2):281-289. Published online April 6, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1333
- 3,864 View
- 133 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Hyperthyroidism is associated with an increased glomerular filtration rate (GFR) in the hyperdynamic state, which is reversible after restoring euthyroidism. However, long-term follow-up of renal dysfunction in patients with hyperthyroidism has not been performed.
Methods
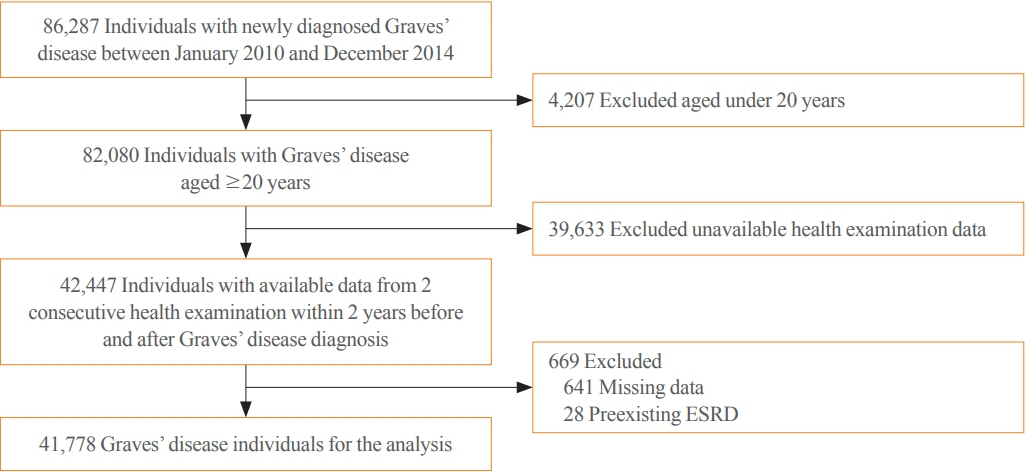
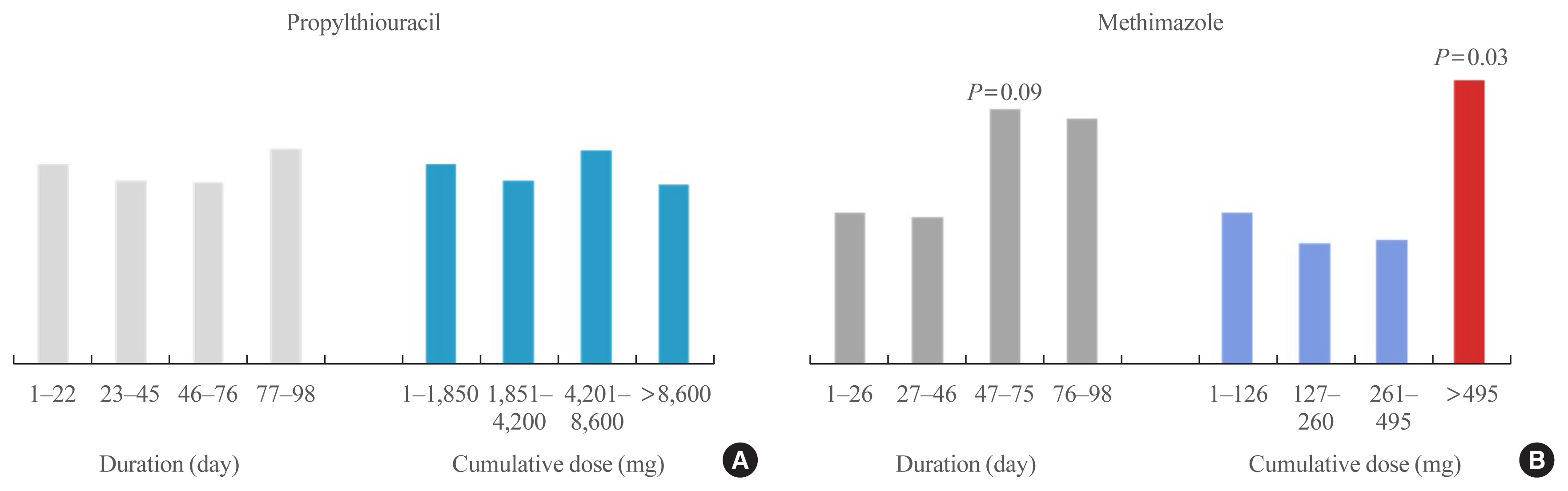
This was a retrospective cohort study using the Korean National Health Insurance database and biannual health checkup data. We included 41,778 Graves’ disease (GD) patients and 41,778 healthy controls, matched by age and sex. The incidences of end-stage renal disease (ESRD) were calculated in GD patients and controls. The cumulative dose and duration of antithyroid drugs (ATDs) were calculated for each patient and categorized into the highest, middle, and lowest tertiles.
Results
Among 41,778 GD patients, 55 ESRD cases occurred during 268,552 person-years of follow-up. Relative to the controls, regardless of smoking, drinking, or comorbidities, including chronic kidney disease, GD patients had a 47% lower risk of developing ESRD (hazard ratio [HR], 0.53; 95% confidence interval [CI], 0.37 to 0.76). In particular, GD patients with a higher baseline GFR (≥90 mL/min/1.73 m2; HR, 0.33; 95% CI, 0.11 to 0.99), longer treatment duration (>33 months; HR, 0.31; 95% CI, 0.17 to 0.58) or higher cumulative dose (>16,463 mg; HR, 0.29; 95% CI, 0.15 to 0.57) of ATDs had a significantly reduced risk of ESRD.
Conclusion
This was the first epidemiological study on the effect of GD on ESRD, and we demonstrated that GD population had a reduced risk for developing ESRD. -
Citations
Citations to this article as recorded by- Renal function changes in patients with subclinical hyperthyroidism: a novel postulated mechanism
Magdy Mohamed Allam, Hanaa Tarek El-Zawawy, Tarek Hussein El-Zawawy
Endocrine.2023; 82(1): 78. CrossRef - Effect of Hyperthyroidism on Preventing Renal Insufficiency
Tae Yong Kim
Endocrinology and Metabolism.2022; 37(2): 220. CrossRef - Effects and Clinical Value of Peritoneal Dialysis on Water and Water Balance, Adverse Reactions, Quality of Life, and Clinical Prognosis in Patients with Decompensated Chronic Nephropathy: A Systematic Review and Meta-Analysis
Xichao Wang, Miaomiao Zhang, Na Sun, Wenxiu Chang, Gang Chen
Computational and Mathematical Methods in Medicine.2022; 2022: 1. CrossRef
- Renal function changes in patients with subclinical hyperthyroidism: a novel postulated mechanism

- Thyroid
Big Data Articles (National Health Insurance Service Database) - Risk of Diabetes in Patients with Long-Standing Graves’ Disease: A Longitudinal Study
- Eyun Song, Min Ji Koo, Eunjin Noh, Soon Young Hwang, Min Jeong Park, Jung A Kim, Eun Roh, Kyung Mook Choi, Sei Hyun Baik, Geum Joon Cho, Hye Jin Yoo
- Endocrinol Metab. 2021;36(6):1277-1286. Published online December 16, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1251
- 5,152 View
- 181 Download
- 9 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
The detrimental effects of excessive thyroid hormone on glucose metabolism have been widely investigated. However, the risk of diabetes in patients with long-standing hyperthyroidism, especially according to treatment modality, remains uncertain, with few longitudinal studies.
Methods
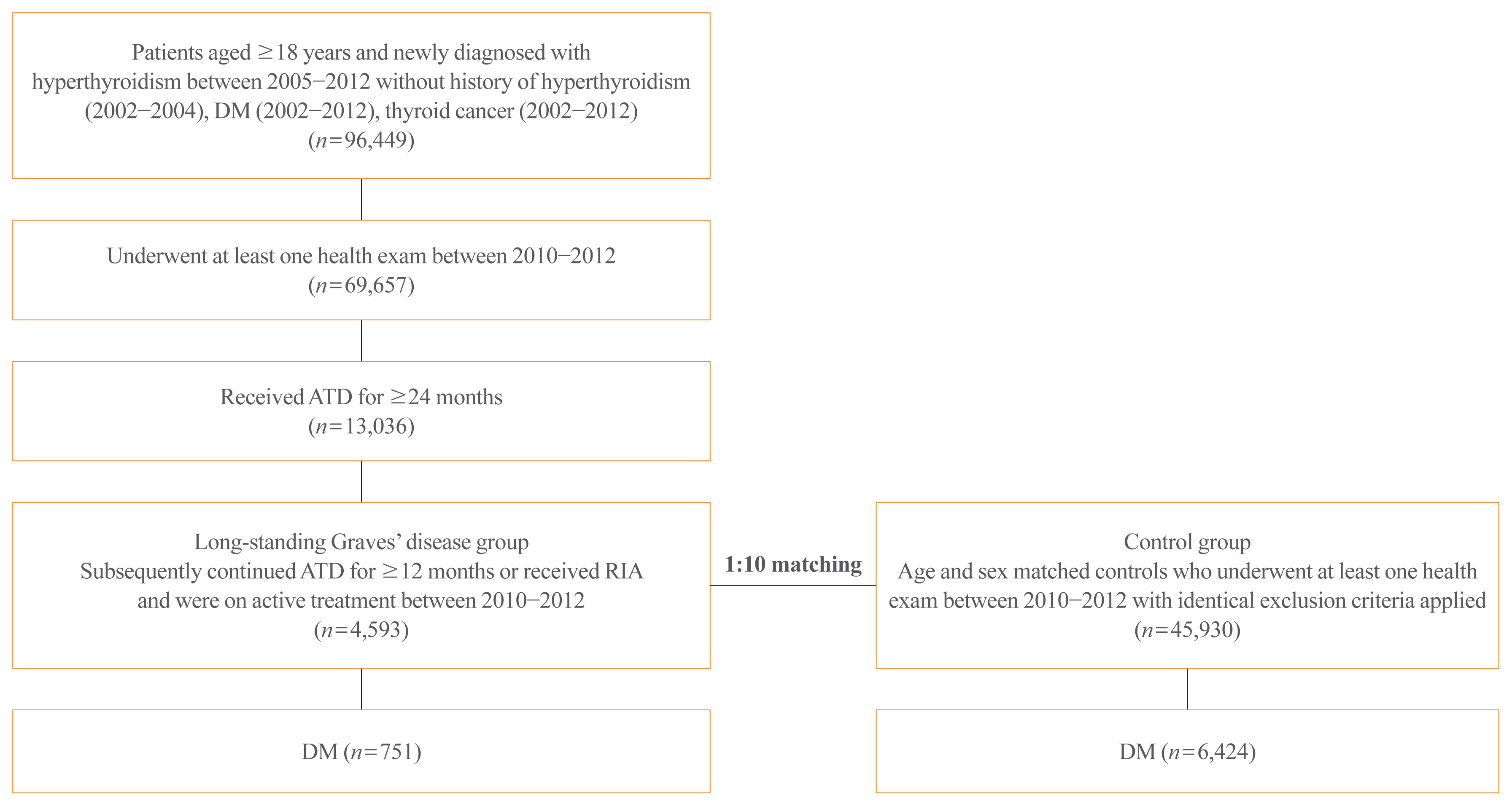
The risk of diabetes in patients with Graves’ disease treated with antithyroid drugs (ATDs) for longer than the conventional duration (≥2 years) was compared with that in age-and sex-matched controls. The risk was further compared according to subsequent treatment modalities after a 24-month course of ATD: continuation of ATD (ATD group) vs. radioactive iodine ablation (RIA) group.
Results
A total of 4,593 patients were included. Diabetes was diagnosed in 751 (16.3%) patients over a follow-up of 7.3 years. The hazard ratio (HR) for diabetes, after adjusting for various known risk factors, was 1.18 (95% confidence interval [CI], 1.10 to 1.28) in patients with hyperthyroidism. Among the treatment modality groups, the RIA group (n=102) had a higher risk of diabetes than the ATD group (n=4,491) with HR of 1.56 (95% CI, 1.01 to 2.42). Further, the risk of diabetes increased with an increase in the ATD treatment duration (P for trend=0.019).
Conclusion
The risk of diabetes was significantly higher in patients with long-standing Graves’ disease than in the general population, especially in patients who underwent RIA and prolonged ATD treatment. Special attention to hyperglycemia during follow-up along with effective control of hyperthyroidism may be necessary to reduce the risk of diabetes in these patients. -
Citations
Citations to this article as recorded by- Safety of non-standard regimen of systemic steroid therapy in patients with Graves’ orbitopathy: a single-centre experience
Nadia Sawicka-Gutaj, Dawid Gruszczyński, Natalia Zawalna, Kacper Nijakowski, Agnieszka Skiba, Mateusz Pochylski, Jerzy Sowiński, Marek Ruchała
Pharmacological Reports.2024; 76(1): 185. CrossRef - Increased risk of diabetes mellitus and hyperlipidemia in patients with differentiated thyroid cancer
Hwa Young Ahn, Jooyoung Lee, Jinmo Kang, Eun Kyung Lee
European Journal of Endocrinology.2024; 190(3): 248. CrossRef - Prevalencia de diabetes en personas con disfunción tiroidea
Juan J. Díez, Pedro Iglesias
Medicina Clínica.2023; 160(8): 333. CrossRef - Control of Thyroid Dysfunction in Spanish Population Registered in
the Primary Care Clinical Database: An Analysis of the Proportion of Patients
with Thyrotropin Values Outside the Reference Range
Juan J. Díez, Pedro Iglesias
Hormone and Metabolic Research.2023; 55(03): 184. CrossRef - Prevalence of thyroid dysfunction and its relationship to income level and employment status: a nationwide population-based study in Spain
Juan J. Díez, Pedro Iglesias
Hormones.2023; 22(2): 243. CrossRef - Prevalence of diabetes in people with thyroid dysfunction
Juan J. Díez, Pedro Iglesias
Medicina Clínica (English Edition).2023; 160(8): 333. CrossRef - Diabetes Mellitus Secondary to Endocrine Diseases: An Update of Diagnostic and Treatment Particularities
Mihaela Simona Popoviciu, Lorena Paduraru, Raluca Marinela Nutas, Alexandra Maria Ujoc, Galal Yahya, Kamel Metwally, Simona Cavalu
International Journal of Molecular Sciences.2023; 24(16): 12676. CrossRef - Thyroid Eye Disease and Its Association With Diabetes Mellitus: A Major Review
Roshmi Gupta, Pramila Kalra, Lakshmi B. Ramamurthy, Suryasnata Rath
Ophthalmic Plastic & Reconstructive Surgery.2023; 39(6S): S51. CrossRef - Metabolite Changes during the Transition from Hyperthyroidism to Euthyroidism in Patients with Graves’ Disease
Ho Yeop Lee, Byeong Chang Sim, Ha Thi Nga, Ji Sun Moon, Jingwen Tian, Nguyen Thi Linh, Sang Hyeon Ju, Dong Wook Choi, Daiki Setoyama, Hyon-Seung Yi
Endocrinology and Metabolism.2022; 37(6): 891. CrossRef - Diabetes and Hyperthyroidism: Is There a Causal Link?
Sang Yong Kim
Endocrinology and Metabolism.2021; 36(6): 1175. CrossRef
- Safety of non-standard regimen of systemic steroid therapy in patients with Graves’ orbitopathy: a single-centre experience

- Thyroid
- Antithyroid Drug Treatment in Graves’ Disease
- Jae Hoon Chung
- Endocrinol Metab. 2021;36(3):491-499. Published online June 16, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1070
- 4,959 View
- 337 Download
- 6 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Graves’ disease is associated with thyrotropin (TSH) receptor stimulating antibody, for which there is no therapeutic agent. This disease is currently treated through inhibition of thyroid hormone synthesis or destruction of the thyroid gland. Recurrence after antithyroid drug (ATD) treatment is common. Recent studies have shown that the longer is the duration of use of ATD, the higher is the remission rate. Considering the relationship between clinical outcomes and iodine intake, recurrence of Graves’ disease is more common in iodine-deficient areas than in iodine-sufficient areas. Iodine restriction in an iodine-excessive area does not improve the effectiveness of ATD or increase remission rates. Recently, Danish and Korean nationwide studies noted significantly higher prevalence of birth defects in newborns exposed to ATD during the first trimester compared to that of those who did not have such exposure. The prevalence of birth defects was lowest when propylthiouracil (PTU) was used and decreased by only 0.15% when methimazole was changed to PTU in the first trimester. Therefore, it is best not to use ATD in the first trimester or to change to PTU before pregnancy.
-
Citations
Citations to this article as recorded by- Выраженность окислительного стресса и энзиматическая активность нейтрофилов крови у пациентов с болезнью Грейвса в зависимости от компенсации гипертиреоза
М. А. Дудина, С. А. Догадин, А. А. Савченко, И. И. Гвоздев
Ateroscleroz.2023; 18(4): 411. CrossRef - Application of oral inorganic iodine in the treatment of Graves’ disease
Yixuan Huang, Yihang Xu, Murong Xu, Xiaotong Zhao, Mingwei Chen
Frontiers in Endocrinology.2023;[Epub] CrossRef - Sex-specific risk factors associated with graves’ orbitopathy in Korean patients with newly diagnosed graves’ disease
Jooyoung Lee, Jinmo Kang, Hwa Young Ahn, Jeong Kyu Lee
Eye.2023; 37(16): 3382. CrossRef - Methimazole, an Effective Neutralizing Agent of the Sulfur Mustard Derivative 2-Chloroethyl Ethyl Sulfide
Albert Armoo, Tanner Diemer, Abigail Donkor, Jerrod Fedorchik, Severine Van slambrouck, Rachel Willand-Charnley, Brian A. Logue
ACS Bio & Med Chem Au.2023; 3(5): 448. CrossRef - Increased risk of incident gout in patients with hyperthyroidism: a nationwide retrospective cohort study
Ju-Yeun Lee, So-Yeon Park, Seo Young Sohn
Rheumatology International.2023; 44(3): 451. CrossRef - The influence of thionamides on intra-thyroidal uptake of 131I during radioiodine-131 treatment of Graves’ disease
Christian Happel, Benjamin Bockisch, Britta Leonhäuser, Amir Sabet, Frank Grünwald, Daniel Groener
Scientific Reports.2023;[Epub] CrossRef - Usefulness of Real-Time Quantitative Microvascular Ultrasonography for Differentiation of Graves’ Disease from Destructive Thyroiditis in Thyrotoxic Patients
Han-Sang Baek, Ji-Yeon Park, Chai-Ho Jeong, Jeonghoon Ha, Moo Il Kang, Dong-Jun Lim
Endocrinology and Metabolism.2022; 37(2): 323. CrossRef - The chemiluminescent and enzymatic activity of blood neutrophils in patients with Graves' disease depending on hyperthyroidism compensation
M. A. Dudina, A. A. Savchenko, S. A. Dogadin, I. I. Gvozdev
Clinical and experimental thyroidology.2022; 18(1): 4. CrossRef - Risk of Diabetes in Patients with Long-Standing Graves’ Disease: A Longitudinal Study
Eyun Song, Min Ji Koo, Eunjin Noh, Soon Young Hwang, Min Jeong Park, Jung A Kim, Eun Roh, Kyung Mook Choi, Sei Hyun Baik, Geum Joon Cho, Hye Jin Yoo
Endocrinology and Metabolism.2021; 36(6): 1277. CrossRef
- Выраженность окислительного стресса и энзиматическая активность нейтрофилов крови у пациентов с болезнью Грейвса в зависимости от компенсации гипертиреоза

- Thyroid
- Graves' Disease: Can It Be Cured?
- Wilmar M. Wiersinga
- Endocrinol Metab. 2019;34(1):29-38. Published online March 21, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.1.29
- 16,104 View
- 511 Download
- 43 Web of Science
- 46 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Whether or not Graves' hyperthyroidism can be really cured, depends on the definition of “cure.” If eradication of thyroid hormone excess suffices for the label “cure,” then all patients can be cured because total thyroidectomy or high doses of 131I will abolish hyperthyroidism albeit at the expense of creating another disease (hypothyroidism) requiring lifelong medication with levothyroxine. I would not call this a “cure,” which I would like to define as a state with stable thyroid stimulating hormone (TSH), free thyroxine, and triiodothyronine serum concentrations in the normal range in the absence of any thyroid medication. Surgery and radioiodine are unlikely to result in so-defined cures, as their preferable aim as stated in guidelines is to cause permanent hypothyroidism. Discontinuation of antithyroid drugs is followed by 50% recurrences within 4 years; before starting therapy the risk of recurrences can be estimated with the Graves' Recurrent Events After Therapy (GREAT) score. At 20-year follow-up about 62% had developed recurrent hyperthyroidism, 8% had subclinical hypothyroidism, and 3% overt hypothyroidism related to TSH receptor blocking antibodies and thyroid peroxidase antibodies. Only 27% was in remission, and might be considered cured. If the definition of “cure” would also include the disappearance of thyroid antibodies in serum, the proportion of cured patients would become even lower.
-
Citations
Citations to this article as recorded by- Multifunctional nanoparticle-mediated combining therapy for human diseases
Xiaotong Li, Xiuju Peng, Makhloufi Zoulikha, George Frimpong Boafo, Kosheli Thapa Magar, Yanmin Ju, Wei He
Signal Transduction and Targeted Therapy.2024;[Epub] CrossRef - Prenatal double-hit with aluminium and cadmium mediate testicular atrophy and hypothalamic hypoplasia: the role of oxido-nitrergic stress and endocrine perturbations
Emmanuel Okhue, Helen Ejiro Kadiri, Patrick Chukwuyenum Ichipi-Ifukor, Benneth Ben-Azu, Samuel Ogheneovo Asagba, Fidelis Ifeakachuku Achuba, John Chukwuma Oyem
BioMetals.2024; 37(2): 477. CrossRef - Surgical outcome after thyroidectomy due to Graves’ disease and Lugol iodine treatment: a retrospective register-based cohort study
Fredric Hedberg, Henrik Falhammar, Jan Calissendorff, Robert Bränström
Endocrine.2024;[Epub] CrossRef - Graves disease is associated with increased risk of clinical Alzheimer’s disease: evidence from the Medicare system
Arseniy Pavlovich Yashkin, Stanislav Kolpakov, Svetlana Ukraintseva, Anatoliy Yashin, Igor Akushevich
Clinical Diabetes and Endocrinology.2024;[Epub] CrossRef - A 2023 International Survey of Clinical Practice Patterns in the Management of Graves Disease: A Decade of Change
Danilo Villagelin, David S Cooper, Henry B Burch
The Journal of Clinical Endocrinology & Metabolism.2024;[Epub] CrossRef - Predictors of Prolonged Euthyroidism After Radioactive Iodine Treatment for Graves’ Disease: A Pilot Study
Jin-Ying Lu, Kuan-Hua Chen, Shyang-Rong Shih, Fang-Yu Wen, Wan-Chen Wu, Ting-Chu Chen, Fu-Chang Hu
Endocrine Practice.2023; 29(2): 89. CrossRef - Case of Graves’ disease recovery
Andrey Valerievich Ushakov
Journal of Clinical and Translational Endocrinology: Case Reports.2023; 27: 100139. CrossRef - Outcomes of Radioactive Iodine Versus Surgery for the Treatment of Graves’ Disease: a Systematic Review and Meta-analysis
Mohamed AbdAlla Salman, Mohamed Moustafa Assal, Ahmed Salman, Mohammed Elsherbiney
Indian Journal of Surgery.2023;[Epub] CrossRef - Association between high mobility group box-1 circulation level and Graves' ophthalmopathy
Mohammad Robikhul Ikhsan, Nyoman Kertia, Supanji Supanji, Bambang Udji djoko Rianto, Dhite Bayu Nugroho
F1000Research.2023; 12: 767. CrossRef - New-onset and relapsed Graves’ disease following COVID-19 vaccination: a comprehensive review of reported cases
Kan Chen, Yiyang Gao, Jing Li
European Journal of Medical Research.2023;[Epub] CrossRef - REVIEW OF SARS-CORONAVIRUS-2 REPERCUSSIONS ON THYROID GLAND IN THE CONTEXT OF HYPERTHYROIDISM
SHUBHAM SINGH, MONIKA, RUPA MAZUMDER, AVIJIT MAZUMDER
International Journal of Applied Pharmaceutics.2023; : 17. CrossRef - Effectiveness and potential mechanism of Jiawei-Xiaoyao-San for hyperthyroidism: a systematic review
Wenxin Ma, Xiaowen Zhang, Ruotong Zhao, Yang Tang, Xiaoyun Zhu, Longkun Liu, Mingyuan Xu, Ge Wang, Peiyue Peng, Jianping Liu, Zhaolan Liu
Frontiers in Endocrinology.2023;[Epub] CrossRef - Associations of serum keratin 1 with thyroid function and immunity in Graves’ disease
Chao-Wen Cheng, Wen-Fang Fang, Jiunn-Diann Lin, Appuwawadu Mestri Nipun Lakshitha de Silva
PLOS ONE.2023; 18(11): e0289345. CrossRef - Management of Graves’ hyperthyroidism: present and future
Luigi Bartalena, Eliana Piantanida, Daniela Gallo, Silvia Ippolito, Maria Laura Tanda
Expert Review of Endocrinology & Metabolism.2022; 17(2): 153. CrossRef - The Prediction Model Using Thyroid-stimulating Immunoglobulin Bioassay For Relapse of Graves’ Disease
Han-Sang Baek, Jaejun Lee, Chai-Ho Jeong, Jeongmin Lee, Jeonghoon Ha, Kwanhoon Jo, Min-Hee Kim, Jae Hyoung Cho, Moo Il Kang, Dong-Jun Lim
Journal of the Endocrine Society.2022;[Epub] CrossRef - Efficacy of Radioiodine Therapy in Patients With Primary Hyperthyroidism: An Institutional Review From Pakistan
Asim Munir Alvi, Umal Azmat, Waqas Shafiq, Abdul Hannan Ali Rasheed, Ahmed Imran Siddiqi, Sardar Khan, Sara Ashfaq, Hira Irfan , Humayun Bashir, Muhammad Abu Bakar, Kashif Asghar
Cureus.2022;[Epub] CrossRef - Clinical Outcomes of Repeated Radioactive Iodine Therapy for Graves’ Disease
Min Joo Kim, Sun Wook Cho, Ye An Kim, Hoon Sung Choi, Young Joo Park, Do Joon Park, Bo Youn Cho
Endocrinology and Metabolism.2022; 37(3): 524. CrossRef - Endocrine Surgery and Pediatic Surgery Partnership Reduces Complication Rate of Pediatric Thyroidectomy
Ali Sayan, Mehmet Üstün, Mehmet Mert, Cem Karaali, Gökhan Köylüoğlu
Journal of Dr Behcet Uz Children s Hospital.2022; 12(2): 164. CrossRef - Thyroid-related adverse events induced by immune checkpoint inhibitors
Alexandra Chera, Andreea Lucia Stancu, Octavian Bucur
Frontiers in Endocrinology.2022;[Epub] CrossRef - A case of Hashimoto's thyroiditis following Graves' disease
Ibtissem Oueslati, Salma Salhi, Meriem Yazidi, Fatma Chaker, Melika Chihaoui
Clinical Case Reports.2022;[Epub] CrossRef - Changes in the T and B lymphocyte subset profiles upon treatment of patients with Graves’ disease with radioactive iodine
A. A. Savchenko, M. A. Dudina, S. A. Dogadin, A. G. Borisov, I. V. Kudryavtsev, D. V. Fomina, V. D. Belenyuk
Medical Immunology (Russia).2022; 24(5): 1007. CrossRef - A survey of the young person’s experience of Graves’ disease and its management
Laura Claire Lane, Judith Rankin, Tim Cheetham
Clinical Endocrinology.2021; 94(2): 330. CrossRef - Serum T3 Level and Duration of Minimum Maintenance Dose Therapy Predict Relapse in Methimazole-Treated Graves Disease
Yotsapon Thewjitcharoen, Krittadhee Karndumri, Waralee Chatchomchuan, Sriurai Porramatikul, Sirinate Krittiyawong, Ekgaluck Wanothayaroj, Siriwan Butadej, Soontaree Nakasatien, Rajata Rajatanavin, Thep Himathongkam
Journal of the Endocrine Society.2021;[Epub] CrossRef - Dosimetry-guided radioiodine therapy of hyperthyroidism: long-term experience and implications for guidelines
Thomas Leitha, Manuela Schartel, Ingrid Hurtl, Rudolf Bednar, Franz König, Karl Mayrhofer, Flavia Pietschmann
Nuclear Medicine Communications.2021; 42(2): 150. CrossRef - Practice patterns and outcomes in the management of Thai patients with Graves’ disease
Yotsapon Thewjitcharoen, Krittadhee Karndumri, Waralee Chatchomchuan, Sriurai Porramatikul, Sirinate Krittiyawong, Ekgaluck Wanathayanoroj, Nampetch Lekpittaya, Worawit Kittipoom, Tawee Anuntakulnatee, Somboon Vongterapak, Siriwan Butadej, Soontaree Nakas
Thyroid Research.2021;[Epub] CrossRef - Un case report letterario di tireotossicosi in La coscienza di Zeno di Italo Svevo
Francesco Trimarchi, Luigi Bartalena, Stefano Arieti, Roberto Toni
L'Endocrinologo.2021; 22(2): 149. CrossRef - Medical treatment of thyrotoxicosis
Lorenzo SCAPPATICCIO, Giuseppe BELLASTELLA, Maria I. MAIORINO, Luca GIOVANELLA, Katherine ESPOSITO
The Quarterly Journal of Nuclear Medicine and Molecular Imaging.2021;[Epub] CrossRef - Hiccups as a Rare Presentation of Thyrotoxicosis Triaged by an Epidural Steroid Injection
Omar Al-Radideh, Iyad Farouji, Theodore DaCosta, Hossam Abed, Nicholas Baranestky
Cureus.2021;[Epub] CrossRef - Long-term antithyroid drug therapy
David S. Cooper
Current Opinion in Endocrinology, Diabetes & Obesity.2021; 28(5): 510. CrossRef - The Continuum of Thyroid Disorders Related to Immune Checkpoint Inhibitors: Still Many Pending Queries
Maria V. Deligiorgi, Sofia Sagredou, Lampros Vakkas, Dimitrios T. Trafalis
Cancers.2021; 13(21): 5277. CrossRef - Recurrence of Graves’ Disease: What Genetics of HLA and PTPN22 Can Tell Us
Daniela Vejrazkova, Josef Vcelak, Eliska Vaclavikova, Marketa Vankova, Katerina Zajickova, Jana Vrbikova, Michaela Duskova, Petra Pacesova, Zdenek Novak, Bela Bendlova
Frontiers in Endocrinology.2021;[Epub] CrossRef - Most Patients with Graves’ Disease Treated with Antithyroid Drugs Eventually Require Additional Therapies
Mary H. Samuels
Clinical Thyroidology.2020; 32(1): 9. CrossRef - Patterns of Use, Efficacy, and Safety of Treatment Options for Patients with Graves' Disease: A Nationwide Population-Based Study
Juan P. Brito, Stephanie Payne, Naykky Singh Ospina, Rene Rodriguez-Gutierrez, Spyridoula Maraka, Lindsey R. Sangaralingham, Nicole M. Iñiguez-Ariza, Victor M. Montori, Marius N. Stan
Thyroid.2020; 30(3): 357. CrossRef - Long-Term Treatment of Hyperthyroidism with Antithyroid Drugs: 35 Years of Personal Clinical Experience
Fereidoun Azizi
Thyroid.2020; 30(10): 1451. CrossRef - Predictive factors for early hypothyroidism following the radioactive iodine therapy in Graves’ disease patients
Rui-Ting Hu, De-Shan Liu, Bin Li
BMC Endocrine Disorders.2020;[Epub] CrossRef - The Concept of Cure in Thyroid Diseases
Fereidoun Azizi
International Journal of Endocrinology and Metabolism.2020;[Epub] CrossRef - Der Biomarker TSH bei Schilddrüsenautonomien
K. Passek, N. Zulauf, E. Wanke, G. M. Oremek
Zentralblatt für Arbeitsmedizin, Arbeitsschutz und Ergonomie.2020; 70(4): 177. CrossRef - Management of Graves’ Hyperthyroidism: More Than a Century of Progression
Hengameh Abdi, Atieh Amouzegar
International Journal of Endocrinology and Metabolism.2020;[Epub] CrossRef - Corticosteroid Pulse Therapy for Graves' Ophthalmopathy Reduces the Relapse Rate of Graves' Hyperthyroidism
Rosario Le Moli, Pasqualino Malandrino, Marco Russo, Fabrizio Lo Giudice, Francesco Frasca, Antonino Belfiore, Riccardo Vigneri
Frontiers in Endocrinology.2020;[Epub] CrossRef - Prediction of Relapse After Antithyroid Drugs Withdrawal: A Narrative Review
Pei-Wen Wang
International Journal of Endocrinology and Metabolism.2020;[Epub] CrossRef - Radioiodine-131 therapy (RIT) in benign thyroid diseases: Personalized prescription based on objectives with optional use of pharmacological modulators
J. Clerc
Médecine Nucléaire.2020; 44(4): 250. CrossRef - Predicting the Risk of Graves Disease Relapse: Commentary on “Thyroid Peroxidase Antibody Positivity is Associated with Relapse-Free Survival Following Antithyroid Drug Treatment for Graves Disease”
D. Gallo, M.L. Tanda, E. Piantanida
Endocrine Practice.2020; 26(9): 1039. CrossRef - Integrating Five Feature Types Extracted From Ultrasonograms to Improve the Prediction of Thyroid Papillary Carcinoma
Renxiang Zhu, Zhongyu Wang, Yifan Zhang, Bingxin Yu, Mingran Qi, Xin Feng, Chenjun Wu, Yuxuan Cui, Lan Huang, Fan Li, Fengfeng Zhou
IEEE Access.2019; 7: 101820. CrossRef - Serum TSH Receptor Antibodies Fall Gradually and Only Rarely Switch Functional Activity in Treated Graves’ Disease
Mary H. Samuels
Clinical Thyroidology.2019; 31(8): 330. CrossRef - Changes in Thyroid Peroxidase and Thyroglobulin Antibodies Might Be Associated with Graves' Disease Relapse after Antithyroid Drug Therapy
Yun Mi Choi, Mi Kyung Kwak, Sang Mo Hong, Eun-Gyoung Hong
Endocrinology and Metabolism.2019; 34(3): 268. CrossRef - A transgenic mouse that spontaneously develops pathogenic TSH receptor antibodies will facilitate study of antigen-specific immunotherapy for human Graves’ disease
Sandra M. McLachlan, Basil Rapoport
Endocrine.2019; 66(2): 137. CrossRef
- Multifunctional nanoparticle-mediated combining therapy for human diseases

- Clinical Study
- Characteristics of Korean Patients with Antithyroid Drug-Induced Agranulocytosis: A Multicenter Study in Korea
- Hee Kyung Kim, Jee Hee Yoon, Min Ji Jeon, Tae Yong Kim, Young Kee Shong, Min Jin Lee, Bo Hyun Kim, In Joo Kim, Ji Young Joung, Sun Wook Kim, Jae Hoon Chung, Ho-Cheol Kang
- Endocrinol Metab. 2015;30(4):475-480. Published online December 31, 2015
- DOI: https://doi.org/10.3803/EnM.2015.30.4.475
- 4,191 View
- 58 Download
- 16 Web of Science
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Antithyroid drugs (ATDs) can lead to the development of agranulocytosis, which is the most serious adverse effect. Characteristics of ATD-induced agranulocytosis (AIA) have seldom been reported due to the rarity. In this study, we characterized the clinical features for AIA in Korean patients.
Methods We retrospectively reviewed data from patients with AIA diagnosed between 1997 and 2014 at four tertiary hospitals. Agranulocytosis was defined as an absolute neutrophil count (ANC) below 500/mm3.
Results The mean age of the patients (11 males, 43 females) was 38.2±14.9 years. Forty-eight patients (88.9%) with AIA had fever and sore throat on initial presentation, 20.4% of patients developed AIA during the second course of treatment, and 75.9% of patients suffered AIA within 3 months after initiation of ATD. The patients taking methimazole (
n =39) showed lower levels of ANC and more frequent use of granulocyte-macrophage colony-stimulating factor than propylthiouracil (n =15) users. The median duration of agranulocytosis was 5.5 days (range, 1 to 20). No differences were observed between the long (≥6 days) and short recovery time (≤5 days) groups in terms of age, gender, ATDs, duration of ATDs, or initial ANC levels. Four patients (7.4%) who were taking ATDs for less than 2 months died of sepsis on the first or second day of hospitalization.Conclusion The majority of AIA incidents occur in the early treatment period. Considering the high fatality rate of AIA, an early aggressive therapeutic approach is critical and patients should be well informed regarding the warning symptoms of the disease.
-
Citations
Citations to this article as recorded by- Novel Association of KLRC4-KLRK1 Gene Polymorphisms with
Susceptibility and Progression of Antithyroid Drug-Induced
Agranulocytosis
Yayi He, Pan Ma, Yuanlin Luo, Xiaojuan Gong, Jiayang Gao, Yuxin Sun, Pu Chen, Suliang Zhang, Yuxin Tian, Bingyin Shi, Bao Zhang
Experimental and Clinical Endocrinology & Diabetes.2024; 132(01): 17. CrossRef - A Disproportionality Analysis of the Adverse Effect Profiles of Methimazole and Propylthiouracil in Patients with Hyperthyroidism Using the Japanese Adverse Drug Event Report Database
Masanori Arai, Takahiro Tsuno, Hiromi Konishi, Kuniyuki Nishiyama, Yasuo Terauchi, Ryota Inoue, Jun Shirakawa
Thyroid®.2023; 33(7): 804. CrossRef - The Current Status of Hyperthyroidism in Korea
Hyemi Kwon
Endocrinology and Metabolism.2023; 38(4): 392. CrossRef - Clinical characteristics of neutropenic patients under antithyroid drug: Twelve-year experience in a medical center
Chih-Hsueh Tseng, Chi-Lung Tseng, Harn-Shen Chen, Pei-Lung Chen, Chun-Jui Huang
Journal of the Chinese Medical Association.2023; 86(9): 826. CrossRef - Association of MICA gene polymorphisms with thionamide-induced agranulocytosis
P. Ma, P. Chen, J. Gao, H. Guo, S. Li, J. Yang, J. Lai, X. Yang, B. Zhang, Y. He
Journal of Endocrinological Investigation.2021; 44(2): 363. CrossRef - Efficacy and adverse events related to the initial dose of methimazole in children and adolescents with Graves’ disease
Hyun Gyung Lee, Eun Mi Yang, Chan Jong Kim
Annals of Pediatric Endocrinology & Metabolism.2021; 26(3): 199. CrossRef - MICA polymorphisms associated with antithyroid drug‐induced agranulocytosis in the Chinese Han population
Xiaojuan Gong, Pu Chen, Pan Ma, Jiayang Gao, Jingsi Yang, Hui Guo, Chunxia Yan, Bao Zhang, Yayi He
Immunity, Inflammation and Disease.2020; 8(4): 695. CrossRef - The Management of Thyroid Disease in COVID-19 Pandemic
Won Sang Yoo, Hyun-Kyung Chung
International Journal of Thyroidology.2020; 13(2): 65. CrossRef - Increased Risk of Antithyroid Drug Agranulocytosis Associated with Amiodarone-Induced Thyrotoxicosis: A Population-Based Cohort Study
Michal Gershinsky, Walid Saliba, Idit Lavi, Chen Shapira, Naomi Gronich
Thyroid.2019; 29(2): 193. CrossRef - A Case of Acute Supraglottitis Following Anti-Thyroid Drug-Induced Agranulocytosis
Jung Jun Lee, Dong Young Kim, Jeon Yeob Jang
Journal of The Korean Society of Laryngology, Phoniatrics and Logopedics.2019; 30(2): 128. CrossRef - Association of HLA-B∗38:02 with Antithyroid Drug-Induced Agranulocytosis in Kinh Vietnamese Patients
Mai Phuong Thao, Pham Vo Anh Tuan, Le Gia Hoang Linh, Lam Van Hoang, Phan Huu Hen, Le Tuyet Hoa, Hoang Anh Vu, Do Duc Minh
International Journal of Endocrinology.2018; 2018: 1. CrossRef - Severe Gingival Ulceration and Necrosis Caused by an Antithyroid Drug: One Case Report and Proposed Clinical Approach
Ying‐Ying Chang, Chih‐Wen Tseng, Kuo Yuan
Clinical Advances in Periodontics.2018; 8(1): 11. CrossRef - Emphasis on the early diagnosis of antithyroid drug-induced agranulocytosis: retrospective analysis over 16 years at one Chinese center
Y. He, J. Li, J. Zheng, Z. Khan, W. Qiang, F. Gao, Y. Zhao, B. Shi
Journal of Endocrinological Investigation.2017; 40(7): 733. CrossRef - Association of HLA-B and HLA-DRB1 polymorphisms with antithyroid drug-induced agranulocytosis in a Han population from northern China
Yayi He, Jie Zheng, Qian Zhang, Peng Hou, Feng Zhu, Jian Yang, Wenhao Li, Pu Chen, Shu Liu, Bao Zhang, Bingyin Shi
Scientific Reports.2017;[Epub] CrossRef - Use of granulocyte colony‐stimulating factor in the treatment of methimazole‐induced agranulocytosis: a case report
Asha Birmingham, Carissa Mancuso, Craig Williams
Clinical Case Reports.2017; 5(10): 1701. CrossRef - 2016 American Thyroid Association Guidelines for Diagnosis and Management of Hyperthyroidism and Other Causes of Thyrotoxicosis
Douglas S. Ross, Henry B. Burch, David S. Cooper, M. Carol Greenlee, Peter Laurberg, Ana Luiza Maia, Scott A. Rivkees, Mary Samuels, Julie Ann Sosa, Marius N. Stan, Martin A. Walter
Thyroid.2016; 26(10): 1343. CrossRef
- Novel Association of KLRC4-KLRK1 Gene Polymorphisms with
Susceptibility and Progression of Antithyroid Drug-Induced
Agranulocytosis


 KES
KES

 First
First Prev
Prev



