Most cited
- Page Path
- HOME > BROWSE ARTICLES > Most cited
From articles published in Endocrinology and Metabolism during the past two years (2022 ~ ).
Review Article
- Diabetes, Obesity and Metabolism
- Human Tissue-Engineered Skeletal Muscle: A Tool for Metabolic Research
- Ji-Hoon Kim, Seung-Min Yu, Jang Won Son
- Endocrinol Metab. 2022;37(3):408-414. Published online June 29, 2022
- DOI: https://doi.org/10.3803/EnM.2022.302
- 3,931 View
- 162 Download
- 1 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
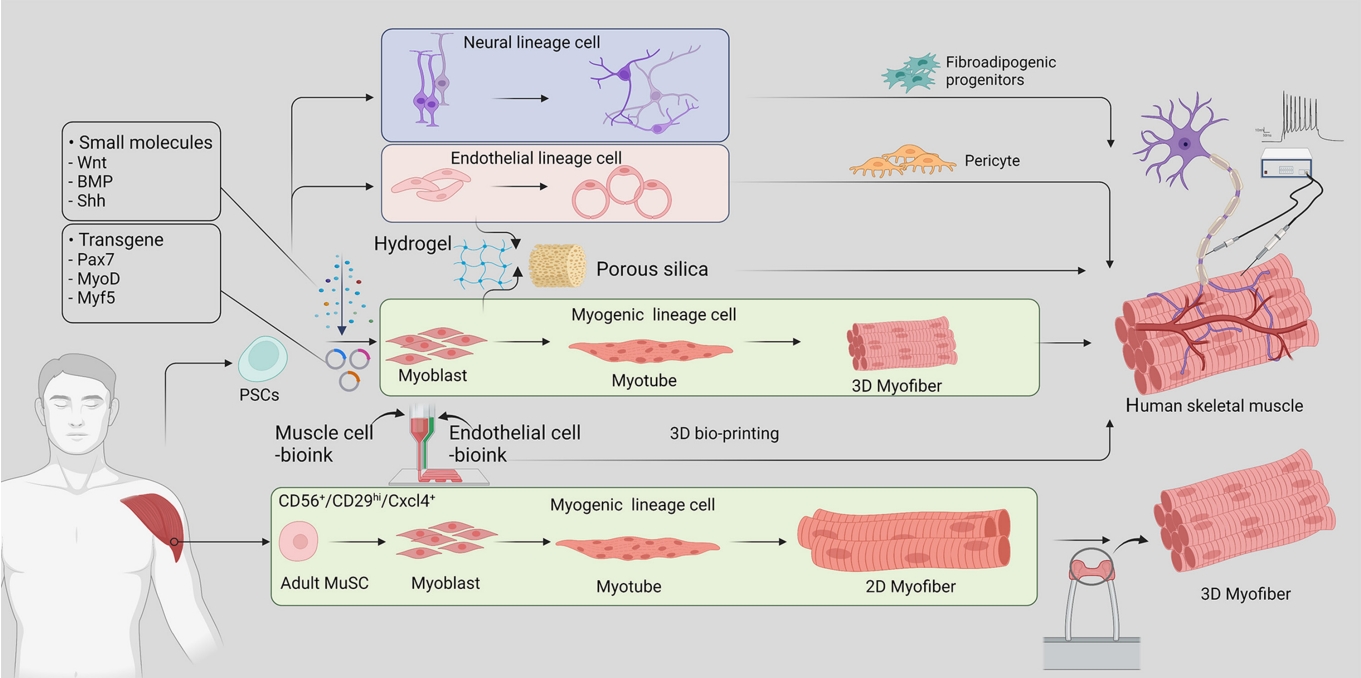
ePub - Skeletal muscle is now regarded as an endocrine organ based on its secretion of myokines and exerkines, which, in response to metabolic stimuli, regulate the crosstalk between the skeletal muscle and other metabolic organs in terms of systemic energy homeostasis. This conceptual basis of skeletal muscle as a metabolically active organ has provided insights into the potential role of physical inactivity and conditions altering muscle quality and quantity in the development of multiple metabolic disorders, including insulin resistance, obesity, and diabetes. Therefore, it is important to understand human muscle physiology more deeply in relation to the pathophysiology of metabolic diseases. Since monolayer cell lines or animal models used in conventional research differ from the pathophysiological features of the human body, there is increasing need for more physiologically relevant in vitro models of human skeletal muscle. Here, we introduce recent studies on in vitro models of human skeletal muscle generated from adult myogenic progenitors or pluripotent stem cells and summarize recent progress in the development of three-dimensional (3D) bioartificial muscle, which mimics the physiological complexity of native skeletal muscle tissue in terms of maturation and functionality. We then discuss the future of skeletal muscle 3D-organoid culture technology in the field of metabolic research for studying pathological mechanisms and developing personalized therapeutic strategies.
-
Citations
Citations to this article as recorded by- Human‐based new approach methodologies to accelerate advances in nutrition research
Manuela Cassotta, Danila Cianciosi, Maria Elexpuru‐Zabaleta, Inaki Elio Pascual, Sandra Sumallo Cano, Francesca Giampieri, Maurizio Battino
Food Frontiers.2024;[Epub] CrossRef - Key indicators of beef safety and quality as important aspects of conservation
S. V. Furman, I. M. Sokulskyi, D. V. Lisohurska, O. V. Lisohurska, B. V. Gutyj
Ukrainian Journal of Veterinary and Agricultural Sciences.2024; 7(1): 68. CrossRef
- Human‐based new approach methodologies to accelerate advances in nutrition research

Brief Reports
- Diabetes, Obesity and Metabolism
- Identification of Healthy and Unhealthy Lifestyles by a Wearable Activity Tracker in Type 2 Diabetes: A Machine Learning-Based Analysis
- Kyoung Jin Kim, Jung-Been Lee, Jimi Choi, Ju Yeon Seo, Ji Won Yeom, Chul-Hyun Cho, Jae Hyun Bae, Sin Gon Kim, Heon-Jeong Lee, Nam Hoon Kim
- Endocrinol Metab. 2022;37(3):547-551. Published online June 29, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1479

- 2,911 View
- 122 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Lifestyle is a critical aspect of diabetes management. We aimed to define a healthy lifestyle using objectively measured parameters obtained from a wearable activity tracker (Fitbit) in patients with type 2 diabetes. This prospective observational study included 24 patients (mean age, 46.8 years) with type 2 diabetes. Expectation–maximization clustering analysis produced two groups: A (n=9) and B (n=15). Group A had a higher daily step count, lower resting heart rate, longer sleep duration, and lower mean time differences in going to sleep and waking up than group B. A Shapley additive explanation summary analysis indicated that sleep-related factors were key elements for clustering. The mean hemoglobin A1c level was 0.3 percentage points lower at the end of follow-up in group A than in group B. Factors related to regular sleep patterns could be possible determinants of lifestyle clustering in patients with type 2 diabetes.
-
Citations
Citations to this article as recorded by- Rethink nutritional management in chronic kidney disease care
Fangyue Chen, Krit Pongpirul
Frontiers in Nephrology.2023;[Epub] CrossRef - Effect of a Wearable Device–Based Physical Activity Intervention in North Korean Refugees: Pilot Randomized Controlled Trial
Ji Yoon Kim, Kyoung Jin Kim, Kyeong Jin Kim, Jimi Choi, Jinhee Seo, Jung-Been Lee, Jae Hyun Bae, Nam Hoon Kim, Hee Young Kim, Soo-Kyung Lee, Sin Gon Kim
Journal of Medical Internet Research.2023; 25: e45975. CrossRef
- Rethink nutritional management in chronic kidney disease care

- Diabetes, Obesity and Metabolism
- Sestrin2 Regulates Beneficial β3-Adrenergic Receptor-Mediated Effects Observed in Inguinal White Adipose Tissue and Soleus Muscle
- Min Jeong Park, Joo Won Kim, Eun Roh, Kyung Mook Choi, Sei Hyun Baik, Hwan-Jin Hwang, Hye Jin Yoo
- Endocrinol Metab. 2022;37(3):552-557. Published online June 29, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1421
- 2,597 View
- 105 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
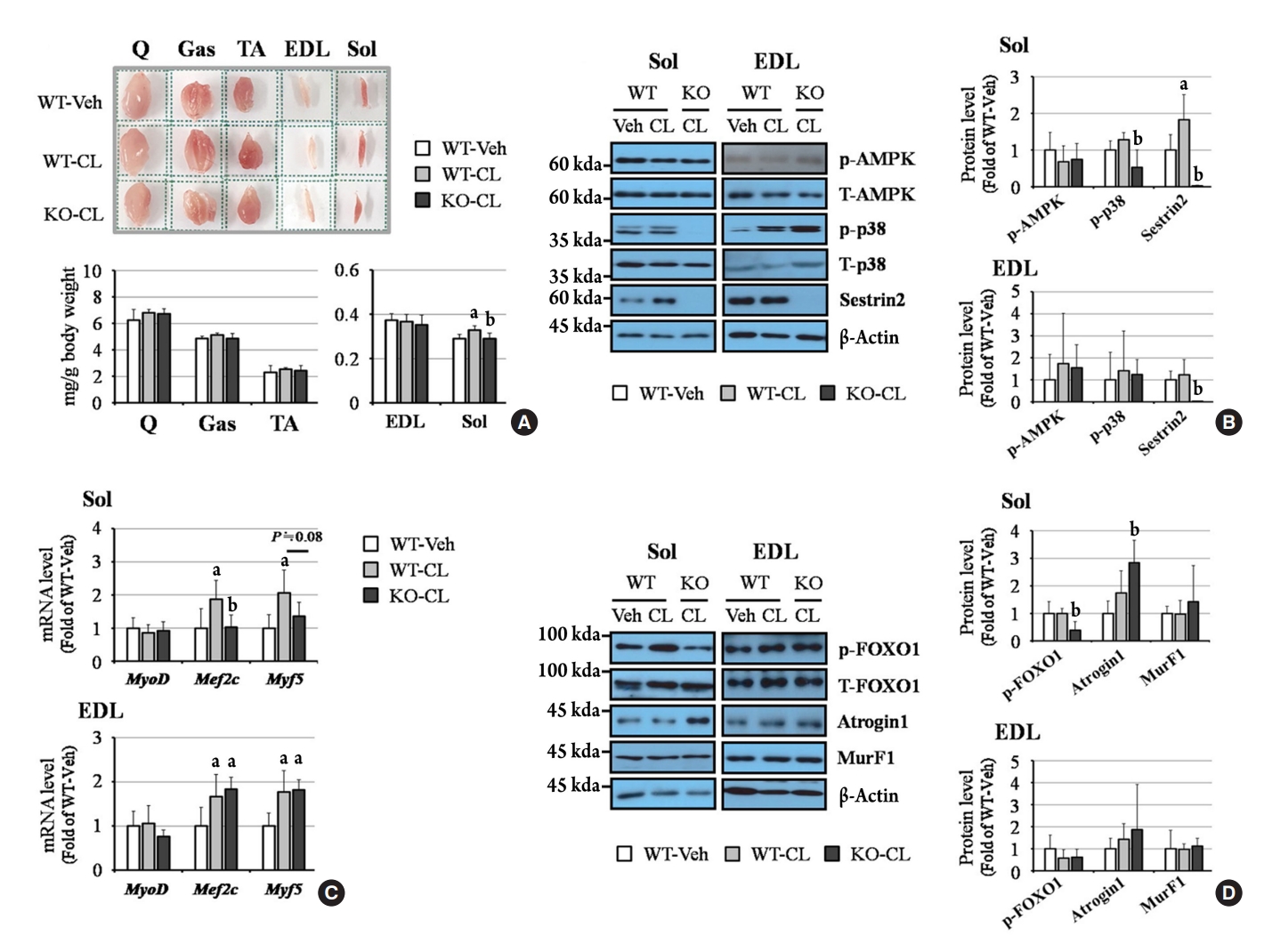
ePub - Sestrin2, a well-known adenosine monophosphate-activated protein kinase (AMPK) regulator, plays a protective role against metabolic stress. The β3-adrenergic receptor (β3AR) induces fat browning and inhibits muscle atrophy in an AMPK-dependent manner. However, no prior research has examined the relationship of sestrin2 with β3AR in body composition changes. In this study, CL 316,243 (CL), a β3AR agonist, was administered to wild-type and sestrin2-knockout (KO) mice for 2 weeks, and fat and muscle tissues were harvested. CL induced AMPK phosphorylation, expression of brown-fat markers, and mitochondrial biogenesis, which resulted in the reduction of lipid droplet size in inguinal white adipose tissue (iWAT). These effects were not observed in sestrin2-KO mice. In CL-treated soleus muscle, sestrin2-KO was related to decreased myogenic gene expression and increased levels of muscle atrophy-related molecules. Our results suggest that sestrin2 is associated with beneficial β3AR-mediated changes in body composition, especially in iWAT and in the soleus.
-
Citations
Citations to this article as recorded by- Sestrin2 levels in patients with anxiety and depression myocardial infarction was up-regulated and suppressed inflammation and ferroptosis by LKB1-mediated AMPK activation
Yufeng Qian, Lian Chen, Beibei Gao, Xianhua Ye
Clinical and Experimental Hypertension.2023;[Epub] CrossRef - Sestrin2 in diabetes and diabetic complications
Xiaodan Zhang, Zirui Luo, Jiahong Li, Yaxuan Lin, Yu Li, Wangen Li
Frontiers in Endocrinology.2023;[Epub] CrossRef
- Sestrin2 levels in patients with anxiety and depression myocardial infarction was up-regulated and suppressed inflammation and ferroptosis by LKB1-mediated AMPK activation

Original Articles
- Thyroid
- Clinical Outcomes of Repeated Radioactive Iodine Therapy for Graves’ Disease
- Min Joo Kim, Sun Wook Cho, Ye An Kim, Hoon Sung Choi, Young Joo Park, Do Joon Park, Bo Youn Cho
- Endocrinol Metab. 2022;37(3):524-532. Published online June 16, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1418
- 4,747 View
- 225 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
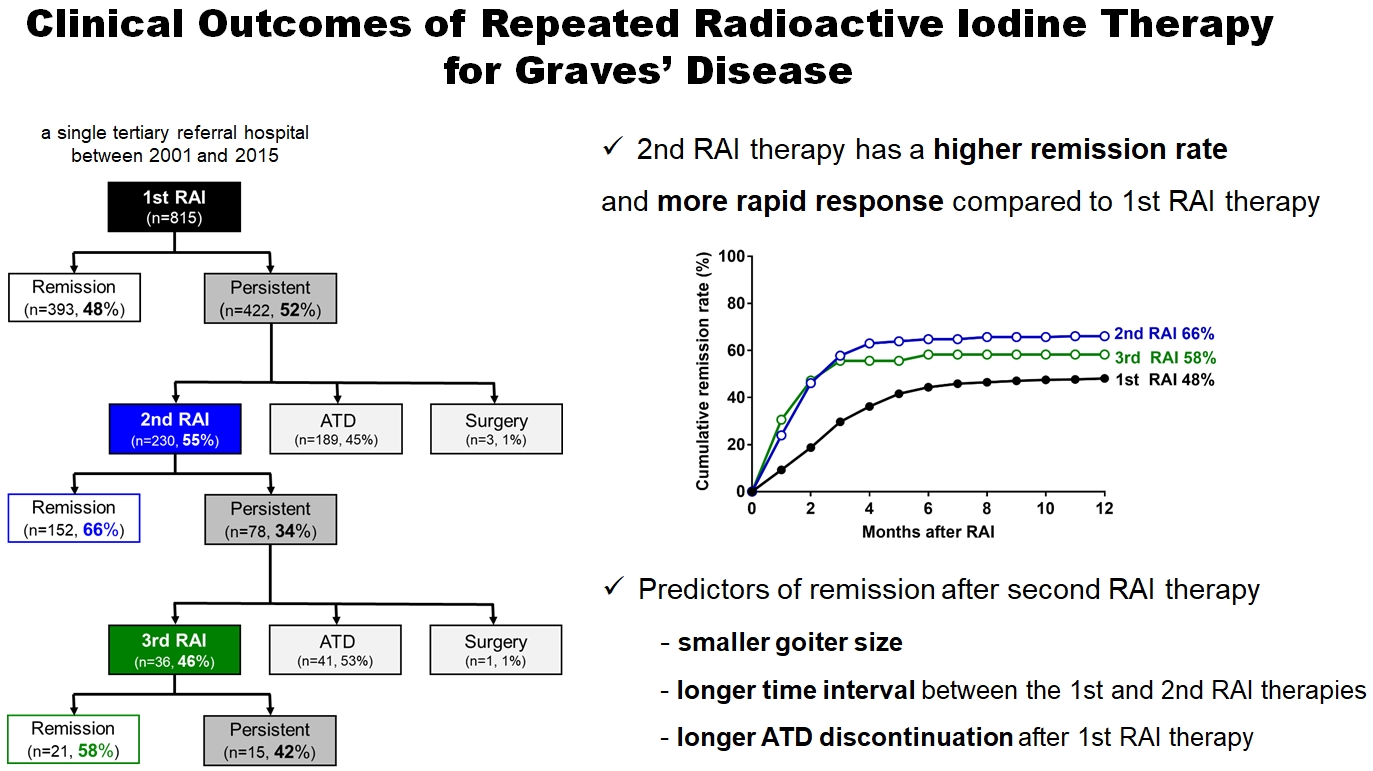
Radioactive iodine (RAI) therapy is a successful therapeutic modality for Graves’ disease. However, RAI therapy can fail, and RAI therapy after antithyroid drugs (ATDs) has a lower remission rate. Therefore, many patients require repeated RAI therapy. This study investigated the clinical outcomes of repeated RAI therapy for Graves’ disease.
Methods
Patients who underwent RAI therapy as second-line therapy after failure of ATD treatment between 2001 and 2015 were reviewed. Remission was defined as hypothyroid or euthyroid status without ATD, and with or without levothyroxine at 12 months after RAI therapy.
Results
The 1-year remission rate after 2nd RAI therapy (66%, 152/230) is significantly higher than that after 1st RAI therapy (48%, 393/815) or long-term ATD treatment after 1st RAI therapy failure (42%). The clinical response to 2nd RAI therapy was more rapid. The median time intervals from the 2nd RAI therapy to ATD discontinuation (1.3 months) and to the start of levothyroxine replacement (2.5 months) were significantly shorter than those for the 1st RAI therapy. A smaller goiter size, a longer time interval between the 1st and 2nd RAI therapies, and a longer ATD discontinuation period predicted remission after the 2nd RAI therapy. Finally, in 78 patients who failed the 2nd RAI therapy, the mean ATD dosage significantly reduced 5.1 mg over 12 months.
Conclusion
Repeated RAI therapy can be a good therapeutic option, especially in patients with smaller goiters and those who are more responsive to the 1st RAI therapy. -
Citations
Citations to this article as recorded by- The Early Changes in Thyroid-Stimulating Immunoglobulin Bioassay over Anti-Thyroid Drug Treatment Could Predict Prognosis of Graves’ Disease
Jin Yu, Han-Sang Baek, Chaiho Jeong, Kwanhoon Jo, Jeongmin Lee, Jeonghoon Ha, Min Hee Kim, Jungmin Lee, Dong-Jun Lim
Endocrinology and Metabolism.2023; 38(3): 338. CrossRef - Effect of liver dysfunction on outcome of radioactive iodine therapy for Graves’ disease
Yuyang Ze, Fei Shao, Xuefeng Feng, Shanmei Shen, Yan Bi, Dalong Zhu, Xiaowen Zhang
BMC Endocrine Disorders.2022;[Epub] CrossRef
- The Early Changes in Thyroid-Stimulating Immunoglobulin Bioassay over Anti-Thyroid Drug Treatment Could Predict Prognosis of Graves’ Disease

- Calcium & Bone Metabolism
- Bone Mineral Density Screening Interval and Transition to Osteoporosis in Asian Women
- Hyunju Park, Heera Yang, Jung Heo, Hye Won Jang, Jae Hoon Chung, Tae Hyuk Kim, Yong-Ki Min, Sun Wook Kim
- Endocrinol Metab. 2022;37(3):506-512. Published online June 9, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1429

- 2,992 View
- 102 Download
- 1 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Bone mineral density (BMD) testing is indicated for women aged 65 years, but screening strategies for osteoporosis are controversial. Currently, there is no study focusing on the BMD testing interval in Asian populations. The current study aimed to evaluate the estimated time interval for screening osteoporosis.
Methods
We conducted a study of 6,385 subjects aged 50 years and older who underwent dual-energy X-ray absorptiometry screening more than twice at Samsung Medical Center as participants in a routine health checkup. Subjects were divided based on baseline T-score into mild osteopenia (T-score, <–1.0 to >–1.5), moderate osteopenia (T-score, ≤–1.5 to >–2.0), and severe osteopenia (T-score, ≤–2.0 to >–2.5). Information about personal medical and social history was collected by a structured questionnaire.
Results
The adjusted estimated BMD testing interval for 10% of the subjects to develop osteoporosis was 13.2 years in mild osteopenia, 5.0 years in moderate osteopenia, and 1.5 years in severe osteopenia.
Conclusion
Our study provides extended information about BMD screening intervals in Asian female population. Baseline T-score was important for predicting BMD screening interval, and repeat BMD testing within 5 years might not be necessary in mild osteopenia subjects. -
Citations
Citations to this article as recorded by- Effects of Bazedoxifene/Vitamin D Combination Therapy on Serum Vitamin D Levels and Bone Turnover Markers in Postmenopausal Women with Osteopenia: A Randomized Controlled Trial
Chaiho Jeong, Jeonghoon Ha, Jun-Il Yoo, Young-Kyun Lee, Jung Hee Kim, Yong-Chan Ha, Yong-Ki Min, Dong-Won Byun, Ki-Hyun Baek, Ho Yeon Chung
Journal of Bone Metabolism.2023; 30(2): 189. CrossRef - Bone-modifying agents for non–small-cell lung cancer patients with bone metastases during the era of immune checkpoint inhibitors: A narrative review
Jinyoung Kim, Chaiho Jeong, Jeongmin Lee, Jeonghoon Ha, Ki-Hyun Baek, Seohyun Kim, Tai Joon An, Chan Kwon Park, Hyoung Kyu Yoon, Jeong Uk Lim
Seminars in Oncology.2023; 50(3-5): 105. CrossRef
- Effects of Bazedoxifene/Vitamin D Combination Therapy on Serum Vitamin D Levels and Bone Turnover Markers in Postmenopausal Women with Osteopenia: A Randomized Controlled Trial

- Diabetes, Obesity and Metabolism
- The Presence of Clonal Hematopoiesis Is Negatively Associated with Diabetic Peripheral Neuropathy in Type 2 Diabetes
- Tae Jung Oh, Han Song, Youngil Koh, Sung Hee Choi
- Endocrinol Metab. 2022;37(2):243-248. Published online April 25, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1337
- 3,295 View
- 122 Download
- 1 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
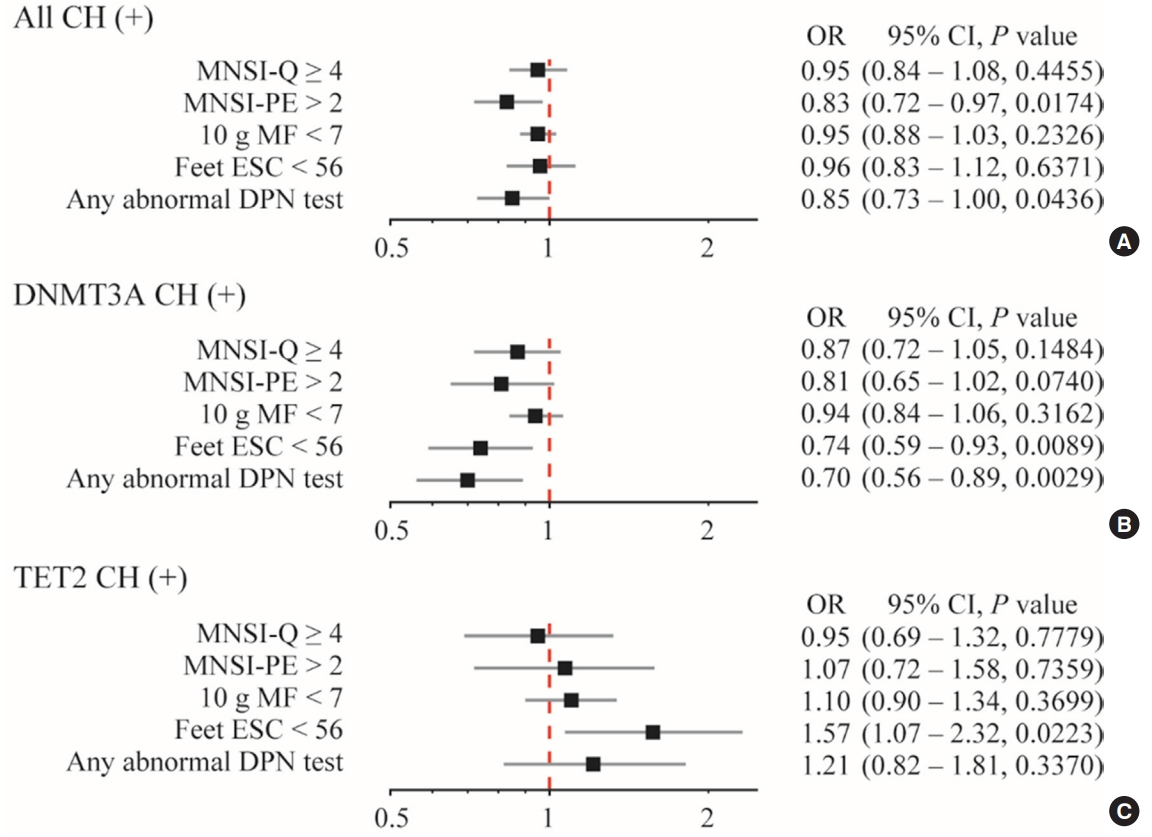
Clonal hematopoiesis of indeterminate potential (CHIP) has been reported to be associated with increased cardiovascular disease, aging and insulin resistance. Despite the debate of causal contribution of CHIP on metabolic diseases, we want to explore whether CHIP is related to diabetic peripheral neuropathy (DPN).
Methods
This study analyzed the prevalence of CHIP in patients with type 2 diabetes classified according to DPN status. Logistic regression analysis was used to evaluate the association between CHIP and DPN.
Results
CHIP was more prevalent in subjects without DPN than those with DPN (19.9% vs. 8.8%, respectively; P=0.013). Individuals having any CHIP, or DNA methyltransferase 3A (DNMT3A) CHIP were less likely to have any abnormality shown in DPN test; the adjusted odds ratio were 0.85 (95% confidence interval [CI], 0.73 to 1.00) and 0.70 (95% CI, 0.56 to 0.89), respectively. Interestingly, DNMT3A CHIP showed the negative association, but Tet methylcytosine dioxygenase 2 (TET2) CHIP showed the positive association with abnormal feet electrochemical skin conductance level.
Conclusion
On the contrary to expectations, CHIP was negatively associated with DPN. Functional linking between the mutation in hematopoietic cells and DPN, and the opposite role of DNMT3A and TET2 should be investigated. -
Citations
Citations to this article as recorded by- TET2 mutation as prototypic clonal hematopoiesis lesion
Luca Guarnera, Babal K. Jha
Seminars in Hematology.2024; 61(1): 51. CrossRef - Clonal hematopoiesis with DNMT3A mutation is associated with lower white matter hyperintensity volume
Woo‐Jin Lee, Keun‐Hwa Jung, Han Song, Heesun Lee, Hyo Eun Park, Youngil Koh, Su‐Yeon Choi, Kyung‐Il Park
CNS Neuroscience & Therapeutics.2023; 29(5): 1243. CrossRef
- TET2 mutation as prototypic clonal hematopoiesis lesion

- Thyroid
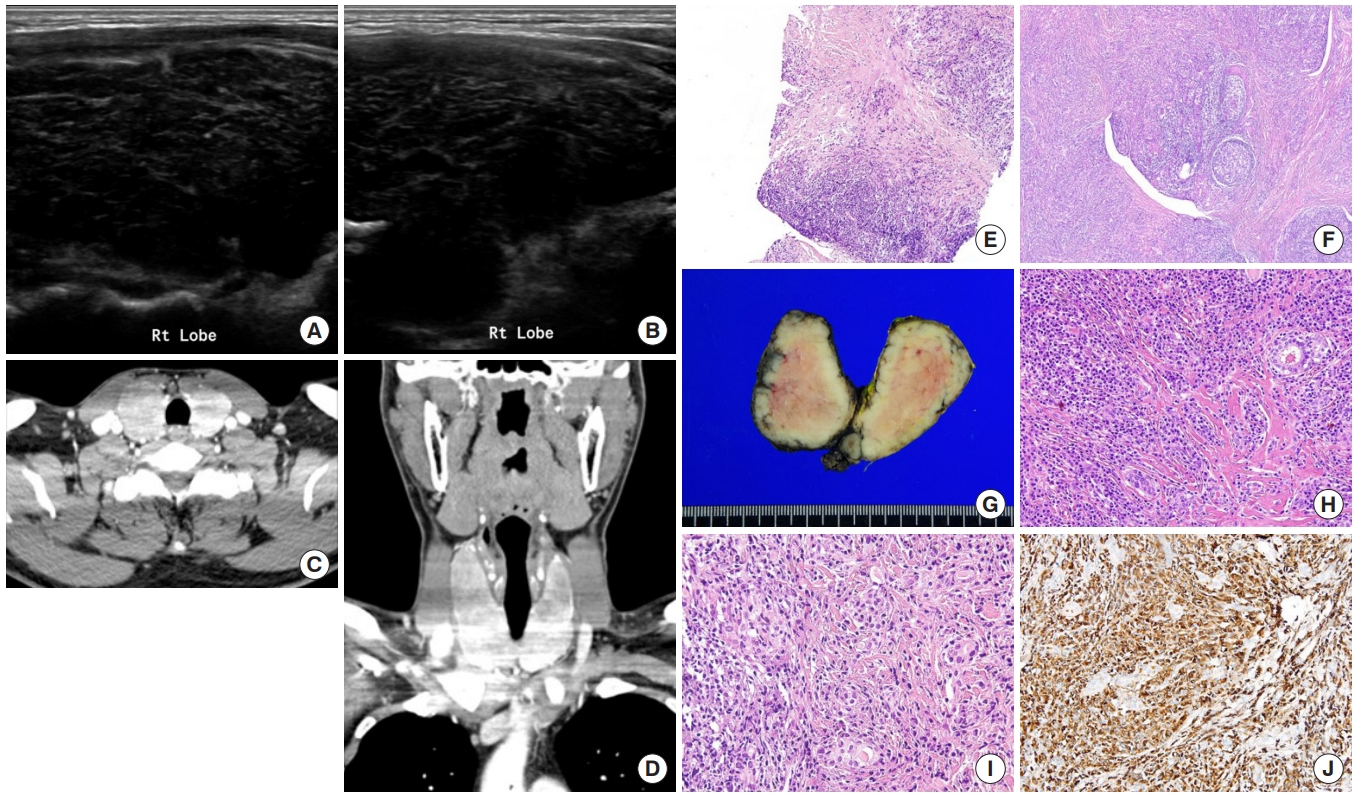
- Immunoglobulin G4-Related Thyroid Disease: A Single-Center Experience and Literature Review
- Meihua Jin, Bictdeun Kim, Ahreum Jang, Min Ji Jeon, Young Jun Choi, Yu-Mi Lee, Dong Eun Song, Won Gu Kim
- Endocrinol Metab. 2022;37(2):312-322. Published online April 25, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1318
- 3,953 View
- 176 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Immunoglobulin G4 (IgG4)-related disease is an entity that can involve the thyroid gland. The spectrum of IgG4-related thyroid disease (IgG4-RTD) includes Hashimoto thyroiditis (HT) and its fibrotic variant, Riedel thyroiditis, as well as Graves’ disease. The early diagnosis of IgG4-RTD is important because it is a medically treatable disease, and a delay in the diagnosis might result in unnecessary surgery. We present a case series of IgG4-RTD with a review of the literature.
Methods
We retrospectively reviewed the clinical presentation and the radiological and pathological findings of patients diagnosed with IgG4-RTD between 2017 and 2021 at a tertiary medical center in Korea. We also conducted a literature review of IgG4-RTD.
Results
Five patients were diagnosed with IgG4-RTD during the study period. The patients’ age ranged from 31 to 76 years, and three patients were men. Most patients visited the clinic for a neck mass, and hypoechogenic nodular lesions were observed on neck ultrasonography. Three patients had IgG4 HT, and two patients had IgG4 Riedel thyroiditis. All patients developed hypothyroidism that necessitated L-thyroxine replacement. The diagnosis of IgG4-RTD was confirmed after a pathological examination of the surgical specimen in the first two cases. However, the early diagnosis was possible after a core needle biopsy in three clinically suspected patients.
Conclusion
The diagnosis of IgG4-RTD requires clinical suspicion combined with serology and histological analyses using IgG4 immunostaining. The early diagnosis of IgG4-RTD is difficult; thus, biopsy with IgG4 immunostaining and serum IgG4 measurements will help diagnose patients suspected of having IgG4-RTD. -
Citations
Citations to this article as recorded by- Are sonographic characteristics of Hashimoto’s thyroiditis related with immunologic parameters? A cross-sectional study
K. Kenarlı, A. B. Bahçecioğlu, Ö. B. Aksu, S. Güllü
Journal of Endocrinological Investigation.2024;[Epub] CrossRef - Reshaping the Concept of Riedel’s Thyroiditis into the Larger Frame of IgG4-Related Disease (Spectrum of IgG4-Related Thyroid Disease)
Mara Carsote, Claudiu Nistor
Biomedicines.2023; 11(6): 1691. CrossRef
- Are sonographic characteristics of Hashimoto’s thyroiditis related with immunologic parameters? A cross-sectional study

Review Article
- Calcium & Bone Metabolism
- Discontinuing Denosumab: Can It Be Done Safely? A Review of the Literature
- Wei Lin Tay, Donovan Tay
- Endocrinol Metab. 2022;37(2):183-194. Published online April 14, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1369

- 16,038 View
- 892 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Denosumab, which has been approved for the treatment of osteoporosis since 2010, is a fully humanised monoclonal antibody against a cytokine, receptor activator of nuclear factor kappa B ligand (RANKL), involved in bone resorption. Continued use of denosumab results in a potent and sustained decrease in bone turnover, an increase in bone mineral density (BMD), and a reduction in vertebral and hip fractures. The anti-resorptive effects of denosumab are reversible upon cessation, and this reversal is accompanied by a transient marked increase in bone turnover that is associated with bone loss, and of concern, an increased risk of multiple vertebral fractures. In this review, we outline the effects of denosumab withdrawal on bone turnover markers, BMD, histomorphometry, and fracture risk. We provide an update on recent clinical trials that sought to answer how clinicians can transition away from denosumab safely with follow-on therapy to mitigate bone loss and summarise the recommendations of various international guidelines.
-
Citations
Citations to this article as recorded by- Loss of lower extremity bone mineral density 1 year after denosumab is discontinued in persons with subacute spinal cord injury
Christopher M. Cirnigliaro, Michael F. La Fountaine, J. Scott Parrott, Steven C. Kirshblum, Susan J. Sauer, Sue A. Shapses, Isa A. McClure, William A. Bauman
Osteoporosis International.2023; 34(4): 741. CrossRef - Persistence with Denosumab in Male Osteoporosis Patients: A Real-World, Non-Interventional Multicenter Study
Chaiho Jeong, Jeongmin Lee, Jinyoung Kim, Jeonghoon Ha, Kwanhoon Jo, Yejee Lim, Mee Kyoung Kim, Hyuk-Sang Kwon, Tae-Seo Sohn, Ki-Ho Song, Moo Il Kang, Ki-Hyun Baek
Endocrinology and Metabolism.2023; 38(2): 260. CrossRef
- Loss of lower extremity bone mineral density 1 year after denosumab is discontinued in persons with subacute spinal cord injury

Original Article
- Diabetes, Obesity and Metabolism
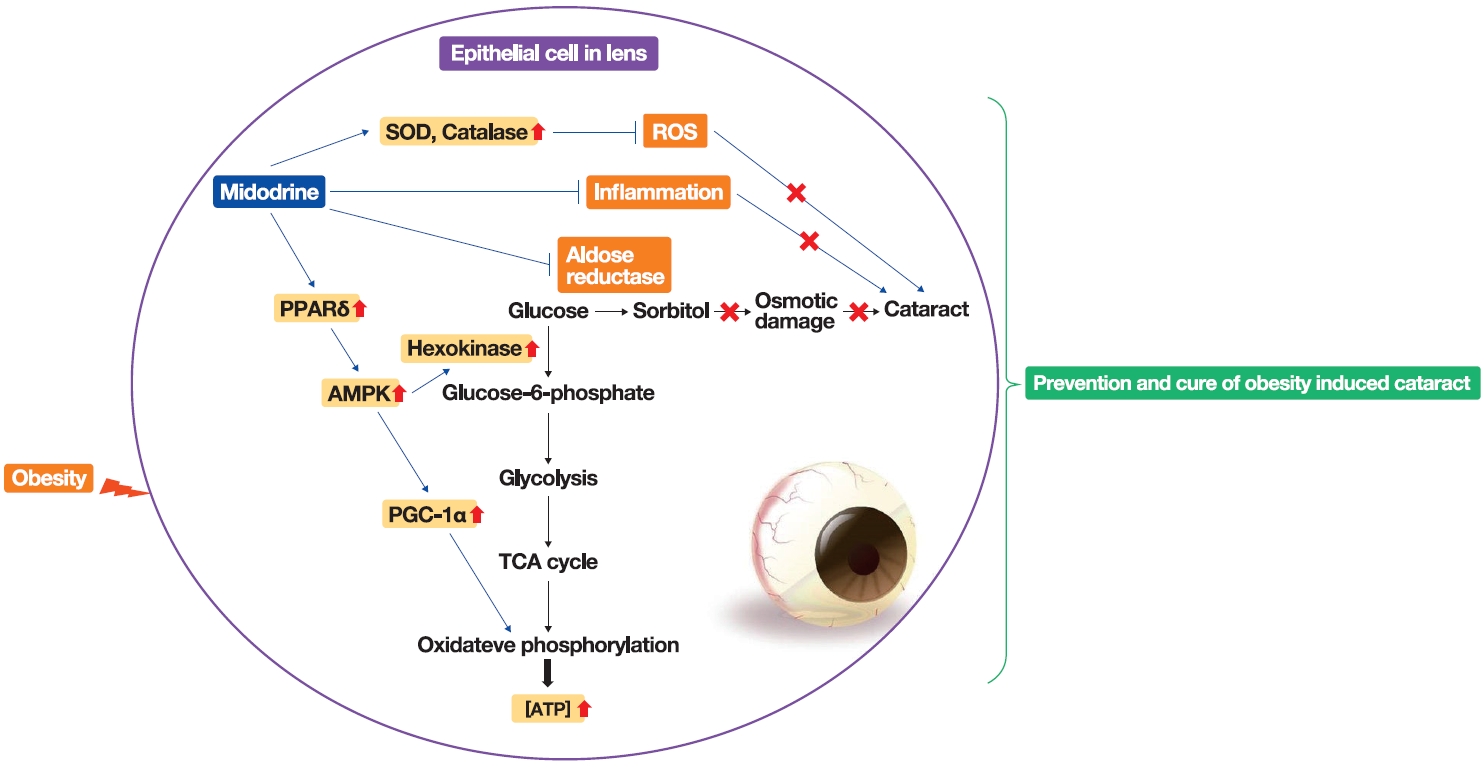
- Stimulation of Alpha-1-Adrenergic Receptor Ameliorates Obesity-Induced Cataracts by Activating Glycolysis and Inhibiting Cataract-Inducing Factors
- Yong-Jik Lee, Yoo-Na Jang, Hyun-Min Kim, Yoon-Mi Han, Hong Seog Seo, Youngsub Eom, Jong-suk Song, Ji Hoon Jeong, Tae Woo Jung
- Endocrinol Metab. 2022;37(2):221-232. Published online March 23, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1237
- 3,573 View
- 134 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Obesity, the prevalence of which is increasing due to the lack of exercise and increased consumption of Westernized diets, induces various complications, including ophthalmic diseases. For example, obesity is involved in the onset of cataracts.
Methods
To clarify the effects and mechanisms of midodrine, an α1-adrenergic receptor agonist, in cataracts induced by obesity, we conducted various analytic experiments in Otsuka Long-Evans Tokushima Fatty (OLETF) rats, a rat model of obesity.
Results
Midodrine prevented cataract occurrence and improved lens clearance in OLETF rats. In the lenses of OLETF rats treated with midodrine, we observed lower levels of aldose reductase, tumor necrosis factor-α, and sorbitol, but higher levels of hexokinase, 5’-adenosine monophosphate-activated protein kinase-alpha, adenosine 5´-triphosphate, peroxisome proliferator-activated receptordelta, peroxisome proliferator-activated receptor gamma coactivator 1-alpha, superoxide dismutase, and catalase.
Conclusion
The ameliorating effects of midodrine on cataracts in the OLETF obesity rat model are exerted via the following three mechanisms: direct inhibition of the biosynthesis of sorbitol, which causes cataracts; reduction of reactive oxygen species and inflammation; and (3) stimulation of normal aerobic glycolysis. -
Citations
Citations to this article as recorded by- α1-Adrenergic Receptors: Insights into Potential Therapeutic Opportunities for COVID-19, Heart Failure, and Alzheimer’s Disease
Dianne M. Perez
International Journal of Molecular Sciences.2023; 24(4): 4188. CrossRef - A new use for old drugs: identifying compounds with an anti-obesity effect using a high through-put semi-automated Caenorhabditis elegans screening platform
Freek Haerkens, Charlotte Kikken, Laurens Kirkels, Monique van Amstel, Willemijn Wouters, Els van Doornmalen, Christof Francke, Samantha Hughes
Heliyon.2022; 8(8): e10108. CrossRef
- α1-Adrenergic Receptors: Insights into Potential Therapeutic Opportunities for COVID-19, Heart Failure, and Alzheimer’s Disease

Editorial
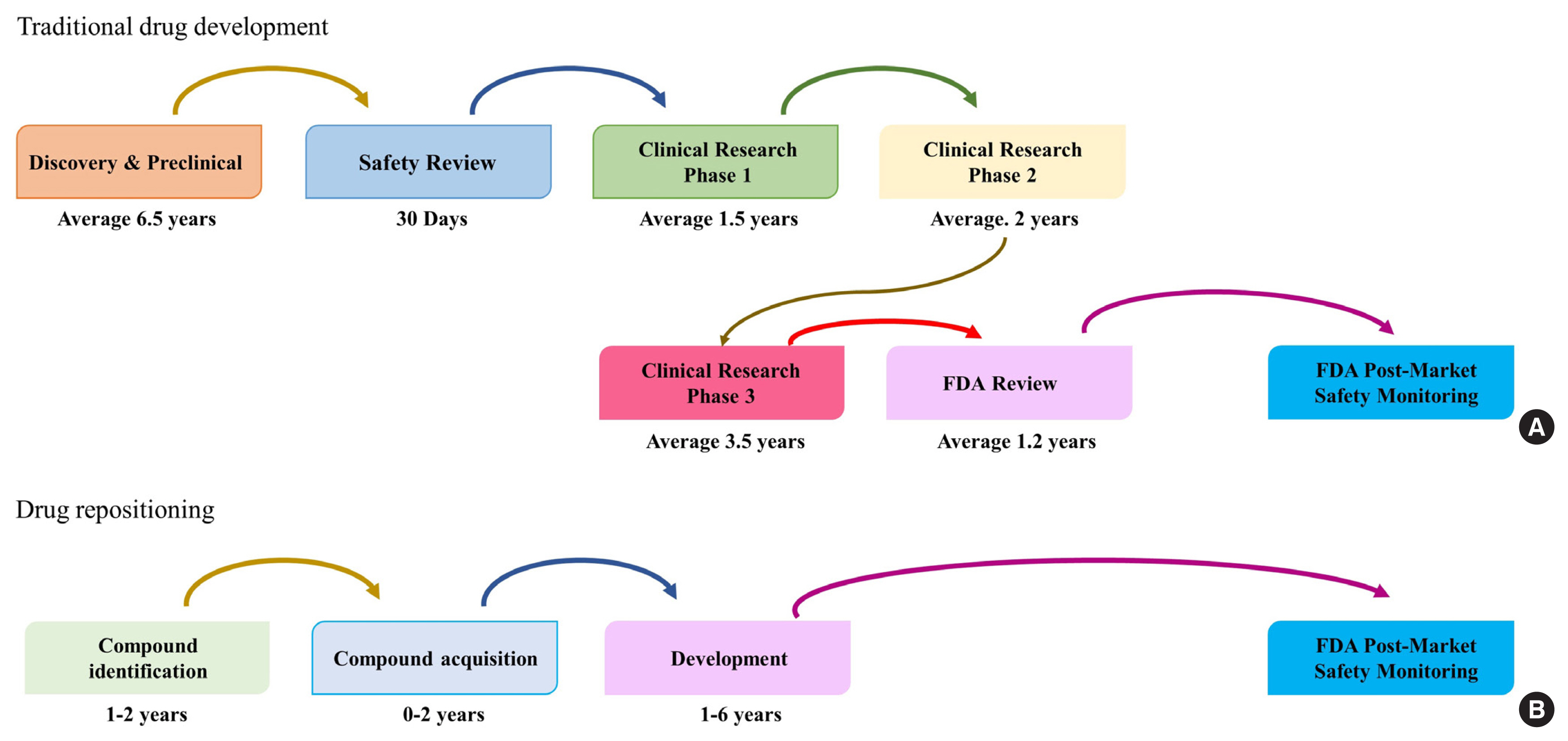
- Diabetes, Obesity and Metabolism
- Drug Repositioning: Exploring New Indications for Existing Drug-Disease Relationships
- Hun-Sung Kim
- Endocrinol Metab. 2022;37(1):62-64. Published online February 28, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1403
- 2,607 View
- 170 Download
- 1 Web of Science
- 2 Crossref
-
 PDF
PDF PubReader
PubReader  ePub
ePub -
Citations
Citations to this article as recorded by- Drug Repositioning Using Computer-aided Drug Design (CADD)
Sona Rawat, Kanmani Subramaniam, Selva Kumar Subramanian, Saravanan Subbarayan, Subramanian Dhanabalan, Sashik Kumar Madurai Chidambaram, Balasubramaniam Stalin, Arpita Roy, Nagaraj Nagaprasad, Mahalingam Aruna, Jule Leta Tesfaye, Bayissa Badassa, Ramaswa
Current Pharmaceutical Biotechnology.2024; 25(3): 301. CrossRef - Magic bullets, magic shields, and antimicrobials in between
Praveen Prathapan
Pharmaceutical Science Advances.2023; 1(1): 100002. CrossRef
- Drug Repositioning Using Computer-aided Drug Design (CADD)

Review Article
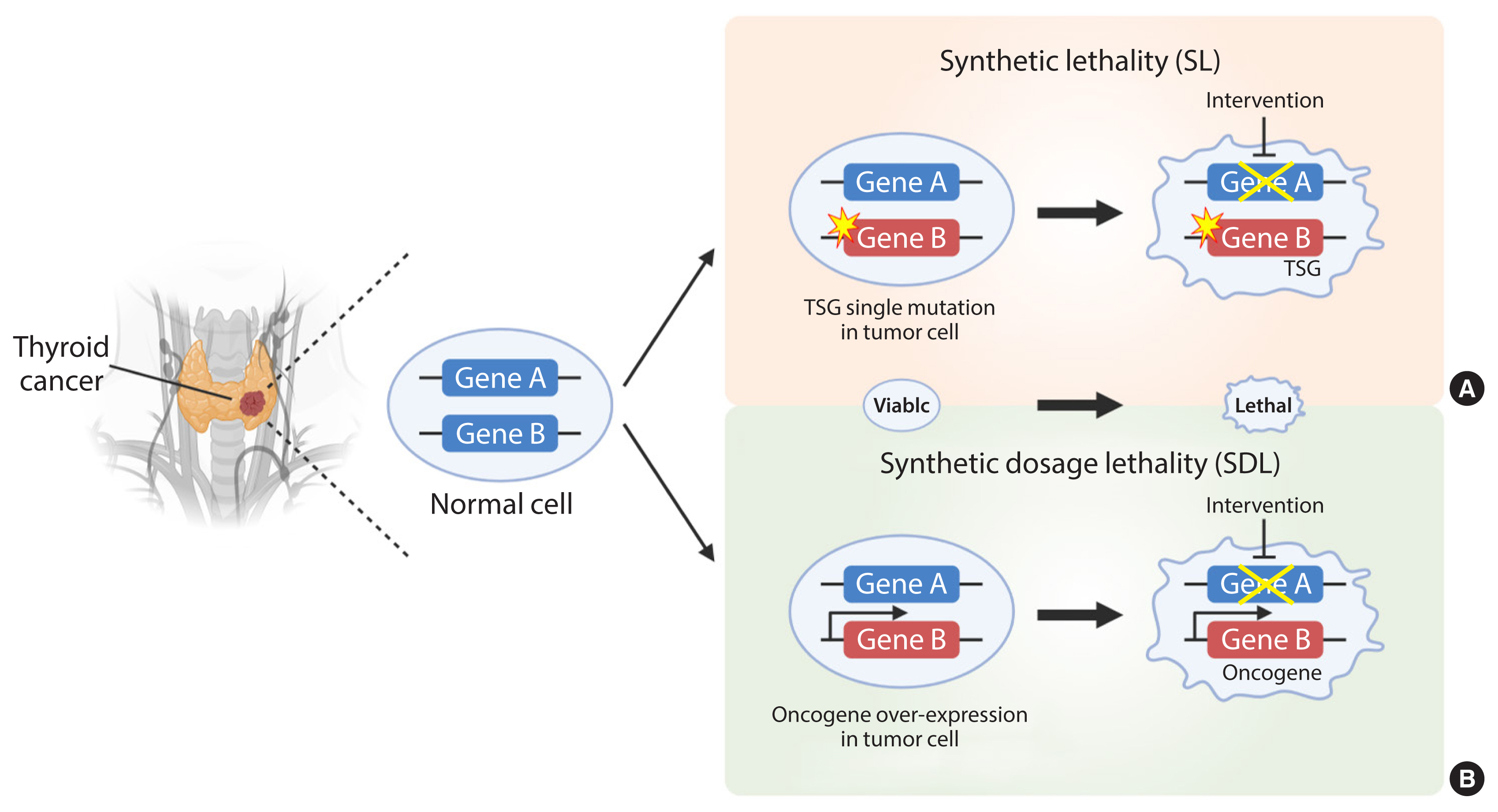
- Thyroid
- Development of Metabolic Synthetic Lethality and Its Implications for Thyroid Cancer
- Sang-Hyeon Ju, Seong Eun Lee, Yea Eun Kang, Minho Shong
- Endocrinol Metab. 2022;37(1):53-61. Published online February 28, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1402
- 3,344 View
- 185 Download
- 1 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Cancer therapies targeting genetic alterations are a topic of great interest in the field of thyroid cancer, which frequently harbors mutations in the RAS, RAF, and RET genes. Unfortunately, U.S. Food and Drug Administration-approved BRAF inhibitors have relatively low therapeutic efficacy against BRAF-mutant thyroid cancer; in addition, the cancer often acquires drug resistance, which prevents effective treatment. Recent advances in genomics and transcriptomics are leading to a more complete picture of the range of mutations, both driver and messenger, present in thyroid cancer. Furthermore, our understanding of cancer suggests that oncogenic mutations drive tumorigenesis and induce rewiring of cancer cell metabolism, which promotes survival of mutated cells. Synthetic lethality (SL) is a method of neutralizing mutated genes that were previously considered untargetable by traditional genotype-targeted treatments. Because these metabolic events are specific to cancer cells, we have the opportunity to develop new therapies that target tumor cells specifically without affecting healthy tissue. Here, we describe developments in metabolism-based cancer therapy, focusing on the concept of metabolic SL in thyroid cancer. Finally, we discuss the essential implications of metabolic reprogramming and its role in the future direction of SL for thyroid cancer.
-
Citations
Citations to this article as recorded by- Toward Systems-Level Metabolic Analysis in Endocrine Disorders and Cancer
Aliya Lakhani, Da Hyun Kang, Yea Eun Kang, Junyoung O. Park
Endocrinology and Metabolism.2023; 38(6): 619. CrossRef - The Role of De novo Serine Biosynthesis from Glucose in Papillary Thyroid Cancer
Seong Eun Lee, Na Rae Choi, Jin-Man Kim, Mi Ae Lim, Bon Seok Koo, Yea Eun Kang
International Journal of Thyroidology.2023; 16(2): 175. CrossRef
- Toward Systems-Level Metabolic Analysis in Endocrine Disorders and Cancer

Brief Report
- Diabetes, Obesity and Metabolism
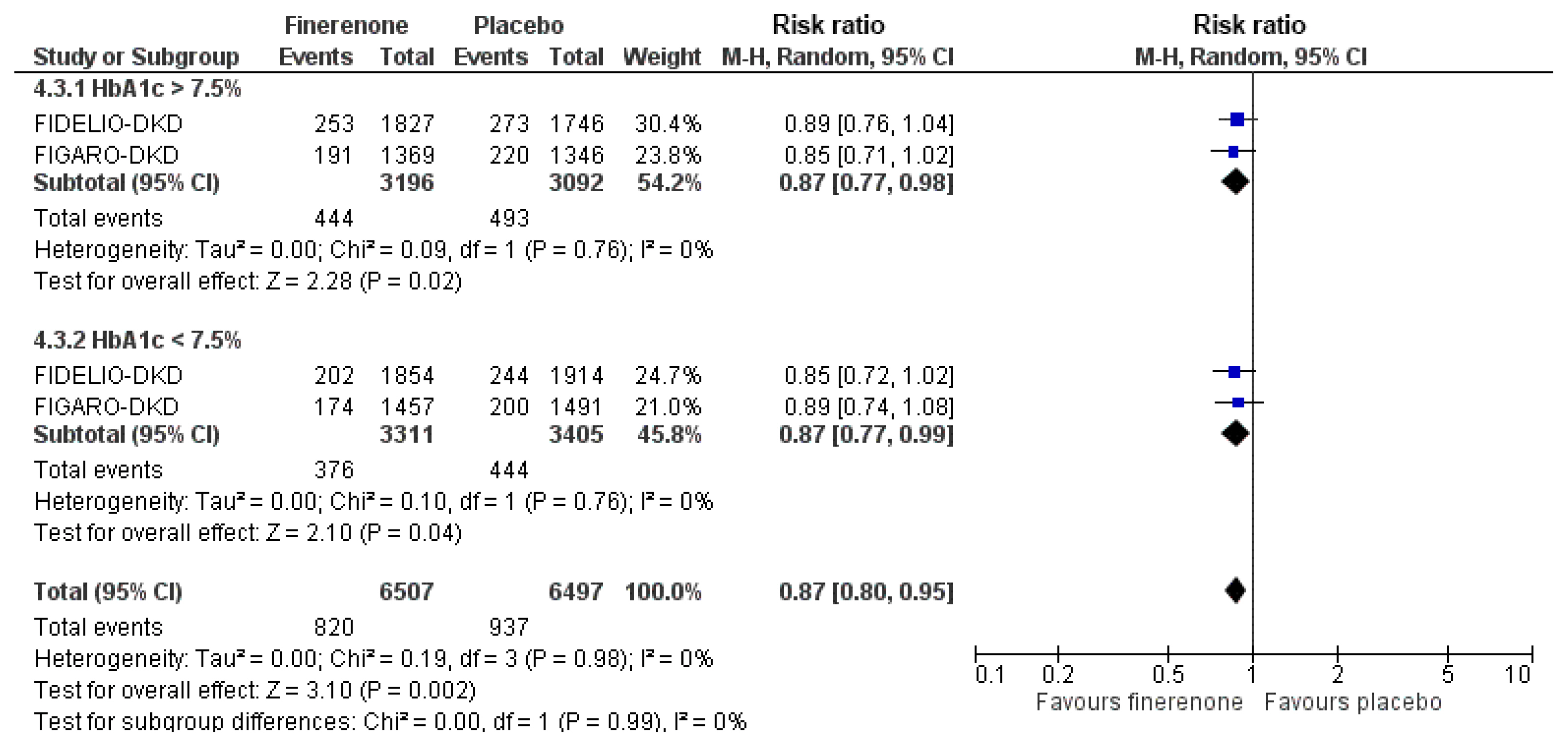
- Cardiovascular Outcomes with Finerenone According to Glycemic Status at Baseline and Prior Treatment with Newer Antidiabetics among Patients with Type 2 Diabetes Mellitus
- Dimitrios Patoulias, Christodoulos Papadopoulos, Asterios Karagiannis, Vassilios Vassilikos, Michael Doumas
- Endocrinol Metab. 2022;37(1):170-174. Published online February 9, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1296
- 3,889 View
- 202 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Type 2 diabetes mellitus (T2DM) and cardiovascular disease are closely interconnected. We sought to determine the cardioprotective action of finerenone according to prior treatment with newer antidiabetics and glycemic status. We searched PubMed and Cochrane Library from inception to October 1, 2021 for randomized controlled trials (RCTs) assessing the effect of finerenone on major adverse cardiovascular outcomes in patients with T2DM. We set the primary endpoint as major adverse cardiovascular events (MACE), defined as the composite of death from cardiovascular causes, nonfatal myocardial infarction, nonfatal stroke, or hospitalization for heart failure. We finally included two RCTs in our quantitative synthesis. Compared to placebo, finerenone induced a 23% risk reduction for the composite cardiovascular endpoint, regardless of prior glycemia. We also showed that finerenone provided significant cardiovascular benefit for obese patients with T2DM compared to placebo, although this benefit was diminished for subjects with a body mass index lower than 30 kg/m2. Finally, the combination of finerenone with sodium-glucose co-transporter-2 inhibitors or glucagon-like peptide-1 receptor agonists did not produce a significant risk reduction for MACE. We conclude that finerenone provides significant cardiovascular benefits for patients with T2DM, especially for those who are obese, while glycemic status or treatment with newer antidiabetics at baseline does not affect the observed cardioprotective action.
-
Citations
Citations to this article as recorded by- Finerenone protects against progression of kidney and cardiovascular damage in a model of type 1 diabetes through modulation of proinflammatory and osteogenic factors
M. Sanz-Gómez, F.J. Manzano-Lista, E. Vega-Martín, D. González-Moreno, M. Alcalá, M. Gil-Ortega, B. Somoza, C. Pizzamiglio, L.M. Ruilope, I. Aránguez, P. Kolkhof, R. Kreutz, M.S. Fernández-Alfonso
Biomedicine & Pharmacotherapy.2023; 168: 115661. CrossRef - Research Progress in Finerenone in Cardiovascular Diseases
Sun Xue, Dong Yanghong, Gu Jiaxin, Liu Wenxiu, Liu Yue
Cardiovascular Innovations and Applications.2023;[Epub] CrossRef
- Finerenone protects against progression of kidney and cardiovascular damage in a model of type 1 diabetes through modulation of proinflammatory and osteogenic factors

Review Article
- Diabetes, obesity and metabolism
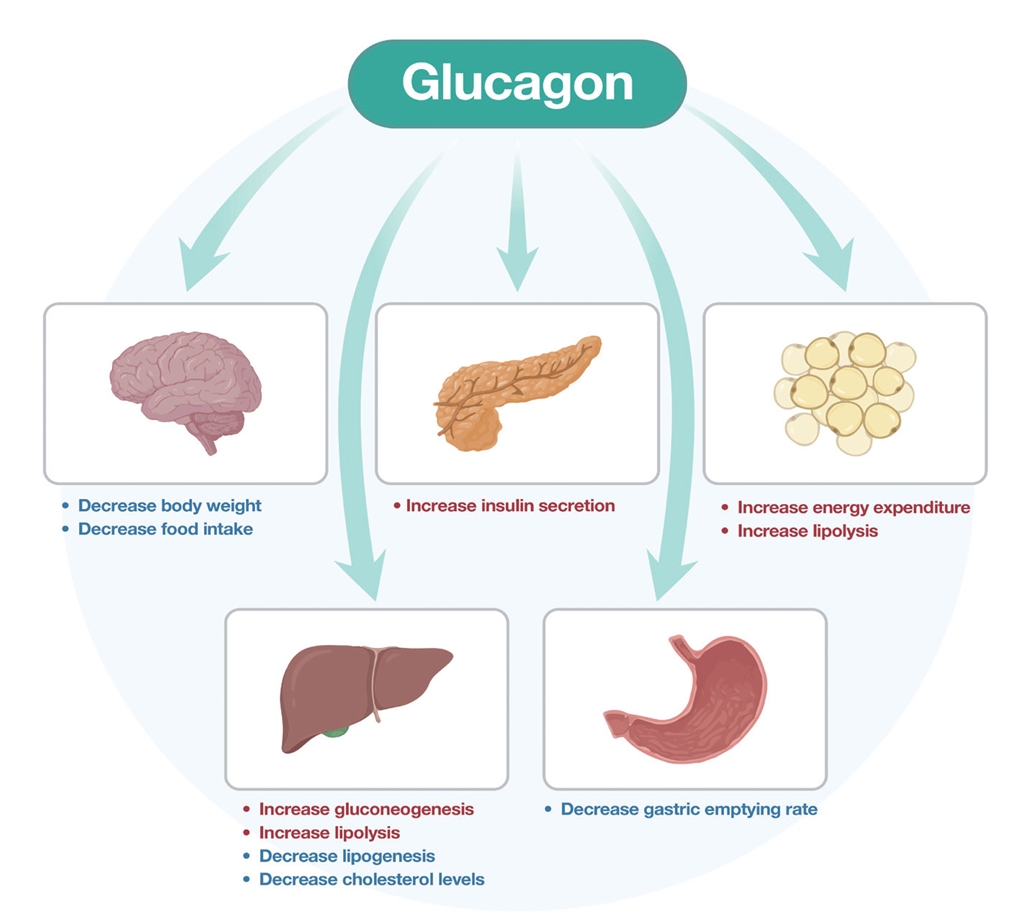
- The Road towards Triple Agonists: Glucagon-Like Peptide 1, Glucose-Dependent Insulinotropic Polypeptide and Glucagon Receptor - An Update
- Agnieszka Jakubowska, Carel W. le Roux, Adie Viljoen
- Endocrinol Metab. 2024;39(1):12-22. Published online February 14, 2024
- DOI: https://doi.org/10.3803/EnM.2024.1942
- 2,351 View
- 189 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Obesity is the fifth leading risk factor for global deaths with numbers continuing to increase worldwide. In the last 20 years, the emergence of pharmacological treatments for obesity based on gastrointestinal hormones has transformed the therapeutic landscape. The successful development of glucagon-like peptide-1 (GLP-1) receptor agonists, followed by the synergistic combined effect of glucose-dependent insulinotropic polypeptide (GIP)/GLP-1 receptor agonists achieved remarkable weight loss and glycemic control in those with the diseases of obesity and type 2 diabetes. The multiple cardiometabolic benefits include improving glycemic control, lipid profiles, blood pressure, inflammation, and hepatic steatosis. The 2023 phase 2 double-blind, randomized controlled trial evaluating a GLP-1/GIP/glucagon receptor triagonist (retatrutide) in patients with the disease of obesity reported 24.2% weight loss at 48 weeks with 12 mg retatrutide. This review evaluates the current available evidence for GLP-1 receptor agonists, dual GLP-1/GIP receptor co-agonists with a focus on GLP-1/GIP/glucagon receptor triagonists and discusses the potential future benefits and research directions.
-
Citations
Citations to this article as recorded by- New Mechanisms to Prevent Heart Failure with Preserved Ejection Fraction Using Glucagon-like Peptide-1 Receptor Agonism (GLP-1 RA) in Metabolic Syndrome and in Type 2 Diabetes: A Review
Jorge E. Jalil, Luigi Gabrielli, María Paz Ocaranza, Paul MacNab, Rodrigo Fernández, Bruno Grassi, Paulina Jofré, Hugo Verdejo, Monica Acevedo, Samuel Cordova, Luis Sanhueza, Douglas Greig
International Journal of Molecular Sciences.2024; 25(8): 4407. CrossRef
- New Mechanisms to Prevent Heart Failure with Preserved Ejection Fraction Using Glucagon-like Peptide-1 Receptor Agonism (GLP-1 RA) in Metabolic Syndrome and in Type 2 Diabetes: A Review

Original Article
- Thyroid
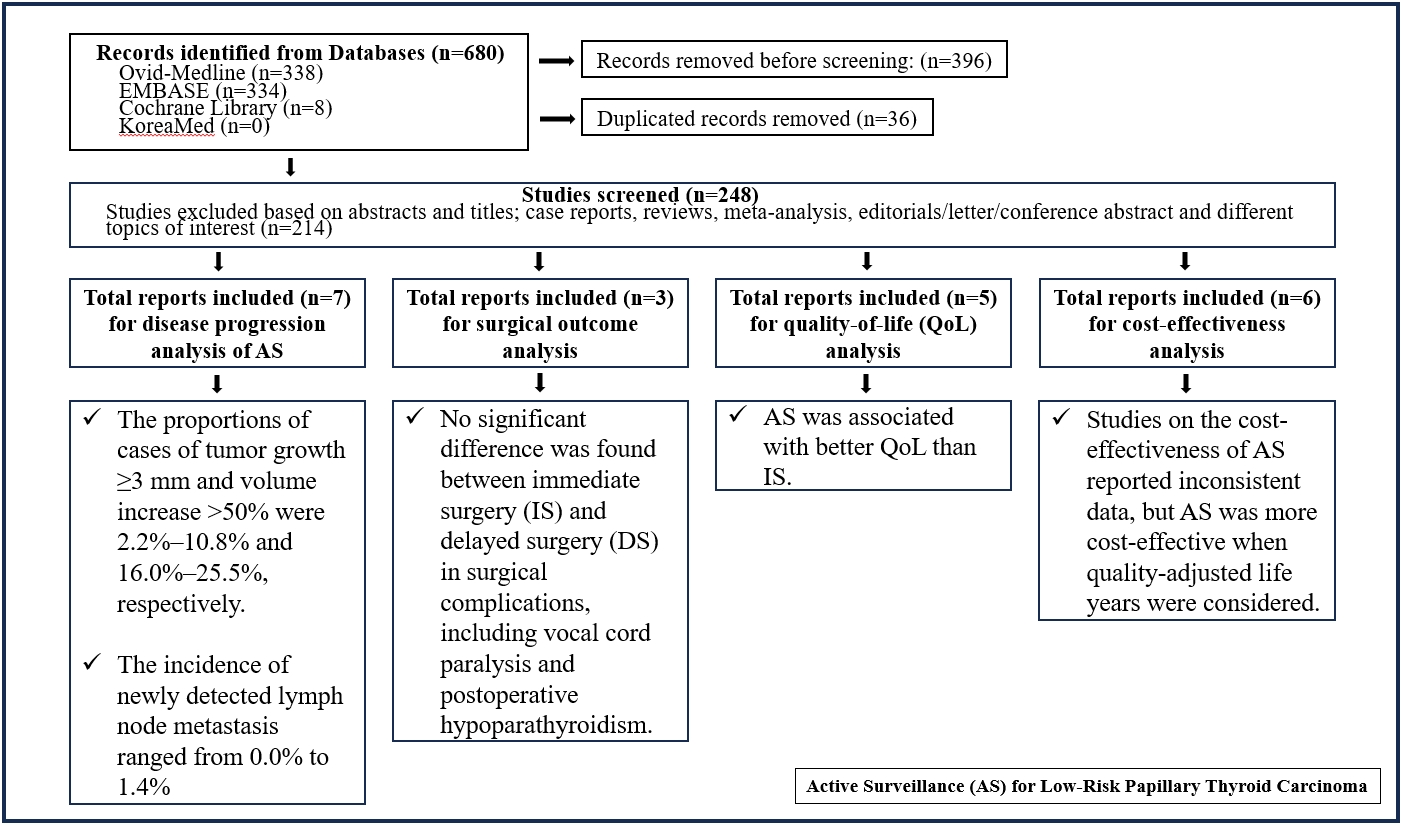
- Active Surveillance for Low-Risk Papillary Thyroid Carcinoma as an Acceptable Management Option with Additional Benefits: A Comprehensive Systematic Review
- Jee Hee Yoon, Wonsuk Choi, Ji Yong Park, A Ram Hong, Hee Kyung Kim, Ho-Cheol Kang
- Endocrinol Metab. 2024;39(1):152-163. Published online January 22, 2024
- DOI: https://doi.org/10.3803/EnM.2023.1794
- 1,081 View
- 39 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Active surveillance (AS) has been introduced as a management strategy for low-risk papillary thyroid carcinoma (PTC) due to its typically indolent nature. Despite this, the widespread adoption of AS has encountered several challenges. The aim of this systematic review was to evaluate the safety of AS related to disease progression and its benefits compared with immediate surgery (IS).
Methods
Studies related to AS in patients with low-risk PTC were searched through the Ovid MEDLINE, Embase, Cochrane Library, and KoreaMed databases. Studies on disease progression, surgical complication, quality of life (QoL), and cost-effectiveness were separately analyzed and narratively synthesized.
Results
In the evaluation of disease progression, the proportions of cases with tumor growth ≥3 mm and a volume increase >50% were 2.2%–10.8% and 16.0%–25.5%, respectively. Newly detected lymph node metastasis was identified in 0.0%–1.4% of patients. No significant difference was found between IS and delayed surgery in surgical complications, including vocal cord paralysis and postoperative hypoparathyroidism. AS was associated with better QoL than IS. Studies on the cost-effectiveness of AS reported inconsistent data, but AS was more cost-effective when quality-adjusted life years were considered.
Conclusion
AS is an acceptable management option for patients with low-risk PTC based on the low rate of disease progression and the absence of an increased mortality risk. AS has additional benefits, including improved QoL and greater QoL-based cost-effectiveness. -
Citations
Citations to this article as recorded by- It Is Time to Understand the Additional Benefits of Active Surveillance for Low-Risk Papillary Thyroid Carcinoma
Kyeong Jin Kim
Endocrinology and Metabolism.2024; 39(1): 95. CrossRef
- It Is Time to Understand the Additional Benefits of Active Surveillance for Low-Risk Papillary Thyroid Carcinoma

Review Article
- Adrenal gland
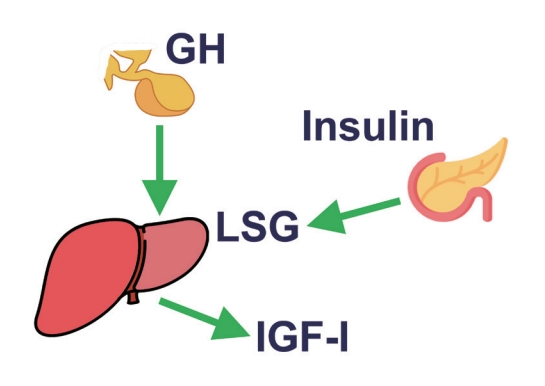
- The Fascinating Interplay between Growth Hormone, Insulin-Like Growth Factor-1, and Insulin
- Eline C. Nijenhuis-Noort, Kirsten A. Berk, Sebastian J. C. M. M. Neggers, Aart J. van der Lely
- Endocrinol Metab. 2024;39(1):83-89. Published online January 9, 2024
- DOI: https://doi.org/10.3803/EnM.2024.101
- 1,487 View
- 111 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - This review intends to provide the reader with a practical overview of several (patho)physiological conditions in which knowledge of the interplay between growth hormone (GH), insulin-like growth factor-1 (IGF-1), and insulin is important. This might help treating physicians in making the right decisions on how to intervene and improve metabolism for the benefit of patients, and to understand why and how metabolism responds in their specific cases. We will specifically address the interplay between GH, IGF-1, and insulin in type 1 and 2 diabetes mellitus, liver cirrhosis, and acromegaly as examples in which this knowledge is truly necessary.
-
Citations
Citations to this article as recorded by- IGF-1 and IGF-2 as Molecules Linked to Causes and Consequences of Obesity from Fetal Life to Adulthood: A Systematic Review
Justyna Szydlowska-Gladysz, Adrianna Edyta Gorecka, Julia Stepien, Izabela Rysz, Iwona Ben-Skowronek
International Journal of Molecular Sciences.2024; 25(7): 3966. CrossRef
- IGF-1 and IGF-2 as Molecules Linked to Causes and Consequences of Obesity from Fetal Life to Adulthood: A Systematic Review


 KES
KES

 First
First Prev
Prev



