Articles
- Page Path
- HOME > Endocrinol Metab > Volume 33(2); 2018 > Article
-
Original ArticlePrevalence and Annual Incidence of Thyroid Disease in Korea from 2006 to 2015: A Nationwide Population-Based Cohort Study
 Audioslide
Audioslide -
Hyemi Kwon1
 , Jin-hyung Jung2, Kyung-Do Han2, Yong-Gyu Park2, Jung-Hwan Cho1, Da Young Lee3, Ji Min Han4, Se Eun Park1, Eun-Jung Rhee1
, Jin-hyung Jung2, Kyung-Do Han2, Yong-Gyu Park2, Jung-Hwan Cho1, Da Young Lee3, Ji Min Han4, Se Eun Park1, Eun-Jung Rhee1 , Won-Young Lee1
, Won-Young Lee1
-
Endocrinology and Metabolism 2018;33(2):260-267.
DOI: https://doi.org/10.3803/EnM.2018.33.2.260
Published online: June 21, 2018
1Division of Endocrinology and Metabolism, Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea.
2Department of Medical Statistics, College of Medicine, The Catholic University of Korea, Seoul, Korea.
3Division of Endocrinology and Metabolism, Department of Internal Medicine, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea.
4Division of Endocrinology and Metabolism, Department of Internal Medicine, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea.
- Corresponding author: Won-Young Lee. Division of Endocrinology and Metabolism, Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, 29 Saemunan-ro, Jongno-gu, Seoul 03181, Korea. Tel: +82-2-2001-2075, Fax: +82-2-2001-1588, wonyoung2.lee@samsung.com
Copyright © 2018 Korean Endocrine Society
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Background
- The incidence of thyroid nodules has increased worldwide in recent years. Thyroid dysfunction is a potential risk factor for hypercholesterolemia, cardiovascular disease, osteoporosis, arrhythmia, and neuropsychiatric disease. This study investigated the prevalence and annual incidence of thyroid nodules, hypothyroidism, and hyperthyroidism in Koreans.
-
Methods
- In this nationwide population-based cohort study, 51,834,660 subjects were included using the National Health Information database from 2006 to 2015, after the exclusion of subjects with thyroid cancer.
-
Results
- The prevalence in Korea in 2015 of thyroid nodules, hypothyroidism in patients taking thyroid hormone, and hyperthyroidism in patients undergoing treatment was 15.82/1,000 population, 15.94/1,000 population, and 2.76/1,000 population, respectively. All these diseases were more prevalent among women than among men. The number of incident cases of these three thyroid diseases steadily increased from 2006 to 2012, and then decreased through 2015. The incidence of thyroid nodules, hypothyroidism treated with thyroid hormone, and treated hyperthyroidism was 6.79/1,000 population, 1.76/1,000 population, and 0.55/1,000 population, respectively, in Korea in 2015. The use of methimazole continuously increased, from 33% of total antithyroid drug prescriptions in 2006 to 74.4% in 2015, and it became the most frequently prescribed antithyroid drug in Korea. In contrast, the use of propylthiouracil continuously decreased.
-
Conclusion
- This was the first nationwide study of the prevalence and annual incidence of thyroid nodules, hypothyroidism, and hyperthyroidism to take into account recent changes and to include the current status of patients receiving treatment.
- The thyroid gland is an endocrine gland that synthesizes and secretes thyroid hormones, which play crucial roles in the control of energy homeostasis and thermogenesis [12]. Thyroid nodule is the most common thyroid disease. The incidence of thyroid nodules has been increasing worldwide in recent years, mainly caused by the widespread use of high-resolution neck ultrasonography (USG) and computed tomography [34567]. Hypothyroidism is a pathological condition of deficient thyroid hormone, whereas hyperthyroidism is a disorder in which excess thyroid hormone is present [12]. Understanding the current distribution of thyroid dysfunction in the population is important, because it is a potential risk factor for hypercholesterolemia, cardiovascular disease, osteoporosis, arrhythmia, and neuropsychiatric disease [8].
- The prevalence of thyroid nodules was found to be 14% to 29% among men and 28% to 42% among women in previous studies of subjects who underwent health checkups in Korea [491011]. However, no studies have investigated the prevalence and annual incidence of thyroid nodules in the entire Korean population. The prevalence and incidence of thyroid dysfunction vary across populations and can be influenced by several factors such as age, sex, ethnicity, and iodine status [121213]. The prevalence of hypothyroidism in the general population has been reported to be from 0.3% to 3.7% in the United States and from 0.2% to 5.3% in European countries [181415]. When subclinical hypothyroidism is also included, the overall prevalence is as high as 15% [1216]. The prevalence of overt hyperthyroidism has been reported as 0.5% to 0.8% in Europe and 0.5% in the United States [814]. Although several studies have reported the prevalence and incidence of thyroid dysfunction in Korea, some studies were not able to take recent changes into account, and other studies did not reveal the current status of patients receiving treatment [16171819].
- This study aimed to investigate the prevalence and annual incidence of thyroid nodules, hypothyroidism, and hyperthyroidism in the entire Korean population using the National Health Information (NHI) database after excluding subjects with thyroid cancer.
INTRODUCTION
- Data source and study population
- In this nationwide population-based cohort study, 51,834,660 subjects were included using the NHI database formed and maintained by the Korean National Health Insurance Service (NHIS), which is managed by the Korean Ministry of Health and Welfare, the governmental organization that supervises all medical services in Korea [20].
- Retrospective cohort data were extracted from 2002 to 2015 based on data collected during the process of claiming health care services using Korean NHIS data. The database includes information on diagnoses based on the reported International Classification of Diseases, 10th revision (ICD-10) codes, utilization records (dates of visits, types of medical institutions, types of visits, length of stay, and medical costs), and prescription records (drug code, days prescribed, and daily dosage) [20]. Because the Korean NHIS has data from 2002, we used a wash-out period from 2002 to 2005, and investigated incidence starting in 2006 to exclude the possibility that patients diagnosed before 2002 were mistaken as new patients. We excluded subjects with thyroid cancer, defined as those with the ICD-10 code C73. This study was approved by the Institutional Review Board of Kangbuk Samsung Hospital (IRB 2017-06-004). It is not necessary to have informed consent in this study.
- Definitions of the diseases
- Subjects with thyroid nodules were defined as those who had the ICD-10 codes E04 and D34. The prevalence was calculated by dividing the number of subjects who had thyroid nodules by the total population in 2015. Incident cases of thyroid nodules were defined as new patients who had thyroid nodules in the study period and did not have thyroid nodules before 2005.
- Subjects with hypothyroidism were defined as those with the ICD-10 codes E02, E03, or E06.3 who took thyroid hormone (levothyroxine, liothyronine, or combination of levothyroxine and liothyronine) for more than 60 days to exclude patients with transient hypothyroidism. The prevalence was calculated by dividing the number of subjects who had hypothyroidism by the total population in 2015. Incident cases of hypothyroidism were defined as new hypothyroidism patients who took thyroid hormone in the study period and did not have any prescriptions for it before 2005.
- Subjects who were treated due to hyperthyroidism were defined as those who had the ICD-10 code E05 and underwent treatment including antithyroid drugs (propylthiouracil [PTU], methimazole [MMI], or carbimazole [CAMZ]), thyroid surgery, or radioactive iodine (RAI) ablation. The antithyroid drug was defined as the first prescribed medicine. Subjects who had an antithyroid drug prescription for fewer than 60 days were excluded. Thyroid surgery was defined as codes P4551-P4554 and RAI ablation was defined as code HD071. Subjects who underwent thyroid surgery or RAI due to hyperthyroidism were included if they had the ICD-10 code E05 or had been prescribed antithyroid drugs. The prevalence and incidence of hyperthyroidism were calculated in the same way as for hypothyroidism.
- Statistical analysis
- For statistical analysis, SAS version 9.3 (SAS Institute Inc., Cary, NC, USA) was used. We used descriptive statistics to investigate the prevalence and annual incidence of thyroid disease and to evaluate trends in treatment modalities for hyperthyroidism. The prevalence and incidence of each disease was calculated by dividing the number of prevalent and incident cases by the total population, respectively, and presented per 1,000 population. Categorical variables are presented as numbers and percentages.
METHODS
- Prevalence and annual incidence of thyroid nodules in Korea
- The prevalence of thyroid nodules according to sex and age group in 2015 is shown in Table 1. The number of patients with thyroid nodules was 0.82 million (0.15 million men and 0.66 million women). The prevalence of thyroid nodules was 15.82/1,000 population in Korea in 2015. Their prevalence among men and women was 5.94/1,000 population and 25.72/1,000 population in 2015, respectively. The prevalence of thyroid nodules was the greatest in the 60 to 69 years age group among both men (15.06/1,000 population) and women (52.41/1,000 population).
- In total, the number of newly diagnosed patients with thyroid nodules steadily increased from 208,200 in 2006 to 458,500 in 2012, and then decreased to 325,400 in 2015 (Fig. 1). This corresponded to 4.36, 9.49, and 6.79 cases/1,000 population among NHIS beneficiaries in 2006, 2012, and 2015, respectively. Among men, the number of newly diagnosed patients with thyroid nodules steadily increased from 40,200 in 2006 to 100,200 in 2012, and then decreased to 80,000 in 2015. Among women, the number of newly diagnosed patients with thyroid nodules steadily increased from 168,000 in 2006 to 358,300 in 2012, and then decreased to 245,400 in 2015.
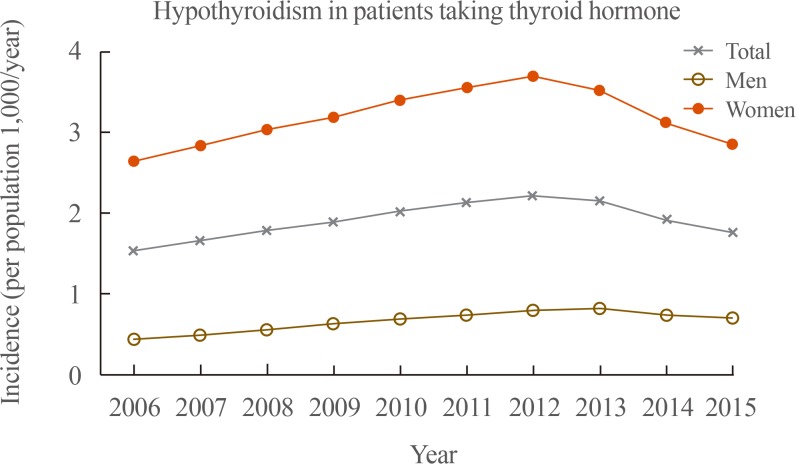
- Prevalence and annual incidence of hypothyroidism in patients taking thyroid hormone in Korea
- The prevalence of hypothyroidism in patients taking thyroid hormone according to sex and age group in 2015 is shown in Table 2. The number of patients who had hypothyroidism and were taking thyroid hormone was 0.82 million (0.13 million men and 0.69 million women). The prevalence of hypothyroidism in patients taking thyroid hormone was 15.94/1,000 population in Korea in 2015. Its prevalence among men and women was 5.15/1,000 population and 26.75/1,000 population, respectively. The prevalence of hypothyroidism in patients taking thyroid hormone was the greatest in the 70 to 79 years age group (13.9/1,000 population) among men, and in the 60 to 69 years age group (55.75/1,000 population) among women.
- In total, the number of newly diagnosed hypothyroidism patients treated with thyroid hormone steadily increased from 73,300 in 2006 to 110,500 in 2012, and then decreased to 88,600 in 2015 (Fig. 2). This corresponded to 1.53, 2.21, and 1.76 cases/1,000 population among NHIS beneficiaries in 2006, 2012, and 2015, respectively. Among men, the number of newly diagnosed hypothyroidism patients treated with thyroid hormone steadily increased from 10,600 in 2006 to 20,000 in 2013, and then decreased to 17,800 in 2015. Among women, the number of those patients steadily increased from 62,600 in 2006 to 90,500 in 2012, and then decreased to 70,700 in 2015.
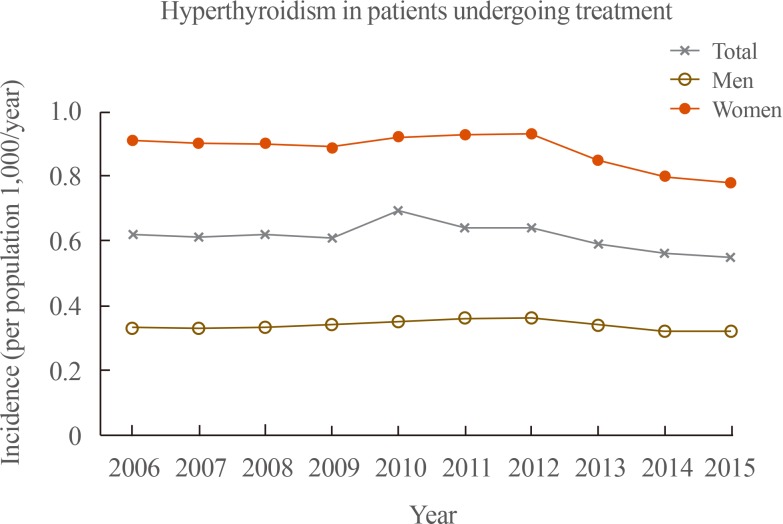
- Prevalence and annual incidence of hyperthyroidism in patients undergoing treatment in Korea
- The prevalence of hyperthyroidism in patients undergoing treatment according to sex and age groups in 2015 is shown in Table 3. The number of patients who had hyperthyroidism and were undergoing treatment was 0.14 million (46,500 men and 96,900 women). The prevalence of hyperthyroidism in patients undergoing treatment was 2.76/1,000 population in Korea in 2015. Its prevalence among men and women was 1.79/1,000 population and 3.74/1,000 population, respectively. The prevalence of hyperthyroidism in patients undergoing treatment was greatest in the 50 to 59 years age group (2.89/1,000 population) among men, and the 60 to 69 years age group (5.71/1,000 population) among women.
- In total, the number of patients newly diagnosed with hyperthyroidism who were undergoing treatment slightly increased from 29,900 in 2006 to 32,400 in 2012, and then decreased to 28,200 in 2015 (Fig. 3). This corresponded to 0.62, 0.64, and 0.55 cases/1,000 population among NHIS beneficiaries in 2006, 2012, and 2015, respectively. Among men, the number of newly diagnosed hyperthyroidism patients who were undergoing treatment slightly increased from 7,900 in 2006 to 9,000 in 2012, and then decreased to 8,200 in 2015. Among women, the number of those patients slightly increased from 21,900 in 2006 to 23,300 in 2012, and then decreased to 19,800 in 2015.
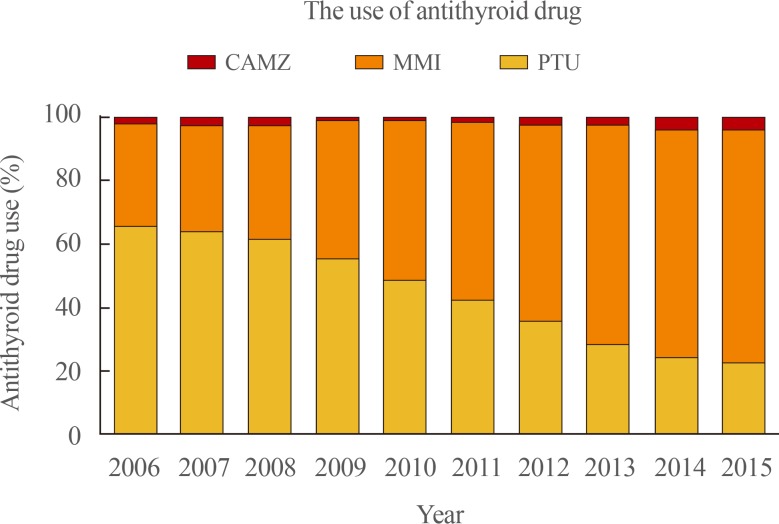
- Changes in the prescription patterns of antithyroid drugs in patients with hyperthyroidism
- The use of different types of antithyroid drugs in patients with hyperthyroidism is illustrated in Fig. 4. PTU was the most commonly used drug for patients with hyperthyroidism before 2009, but MMI overtook PTU in 2010. Among 30,000 patients with hyperthyroidism in 2006, 65.8% of all prescriptions for antithyroid drugs were PTU, while MMI was used only in 30% of patients. The use of MMI continuously increased to 74.4% of total antithyroid drug prescriptions in 2015, and it became the most frequently prescribed antithyroid drug in Korea. In contrast, the use of PTU steadily decreased to 22.3% in 2015.
RESULTS
- This nation-wide cross-sectional study investigated the prevalence and annual incidence of thyroid nodules, hypothyroidism, and hyperthyroidism in Korea using the NHI database after excluding of subjects with thyroid cancer. The prevalence of thyroid nodules, hypothyroidism in patients taking thyroid hormone, and hyperthyroidism in patients undergoing treatment was 15.82/1,000 population, 15.94/1,000 population, and 2.76/1,000 population in Korea in 2015, respectively. All these diseases were more prevalent among women than among men. In total, the number of incident cases of these three thyroid diseases steadily increased from 2006 to 2012, and then decreased through 2015. The incidence of thyroid nodules, hypothyroidism in patients taking thyroid hormone, and hyperthyroidism in patients undergoing treatment was 6.79/1,000 population, 1.76/1,000 population, and 0.55/1,000 population in Korea in 2015. The use of MMI continuously increased from 33% of total antithyroid drug prescriptions in 2006 to 74.4% in 2015, and it became the most frequently prescribed antithyroid drug in Korea, while the use of PTU continuously decreased.
- Several studies of Korean subjects with thyroid nodules who underwent health checkups have been reported [491011]. The prevalence of thyroid nodules was 14% to 29% among men and 28% to 42% among women [491011]. However, those studies could not reflect the current state of the population and clinical practice, because the examinees of health checkup might be unusually interested in their health and have a relatively high prevalence of thyroid nodules. In the current study, the prevalence of thyroid nodules among men and women was 5.94/1,000 population and 25.72/1,000 population in 2015, respectively. The prevalence of thyroid nodules was the greatest in the 60 to 69 years age group among both men (15.06/1,000 population) and women (52.41/1,000 population).
- In the current study, 5.15/1,000 population among men and 26.75/1,000 population among women took thyroid hormone due to hypothyroidism. Several studies have investigated the prevalence and incidence of hypothyroidism in Korea [161719]. A previous study using claims data provided by the Health Insurance Review and Assessment Service (HIRA) reported that the prevalence of hypothyroidism was 14.28/1,000 population in Korea in 2015 [17]. Another cohort study reported that the prevalence of subclinical hypothyroidism in the Ansung cohort and Korean Longitudinal Study on Health and Aging Study was 11.7% and 17.3%, respectively [19]. Recently, a study investigated the prevalence of hypothyroidism and hyperthyroidism using the Korea National Health and Nutrition Examination Survey VI (KNHANES VI, 2013 to 2015) by applying the reference interval of serum thyroid stimulating hormone in the Korean reference population [16]. The study reported that the prevalence of overt and subclinical hypothyroidism was 0.73% and 3.10%, respectively [16]. However, the study could not reflect the actual clinical prevalence of the disease, because the authors evaluated the prevalence of the disease after excluding patients with a prior history of thyroid disease or taking medicine that could influence thyroid function [16].
- The prevalence of hyperthyroidism in patients undergoing treatment was 1.79/1,000 population among men and 3.74/1,000 population among women in this study. The prevalence of hyperthyroidism reported by previous studies from Korea was similar to that of other countries [814]. In a previous study published in 2013 using the HIRA database, the prevalence of hyperthyroidism was 3.40/1,000 population (2.09 among men and 4.70 among women), and the incidence of hyperthyroidism was 0.72/1,000 population (0.40 among men and 1.03 among women) [18]. The study using the KNHANES VI reported that the prevalence of overt and subclinical hyperthyroidism in the disease-free population was 0.54% and 2.98%, respectively [16].
- The number of incident cases of thyroid nodules, hypothyroidism, and hyperthyroidism steadily increased from 2006 to 2012, and then decreased to 2015. In 2010, the Korean Thyroid Association (KTA) presented revised guidelines for the diagnosis and management of thyroid nodules and cancer and size criteria of thyroid nodules for applying fine-needle aspiration cytology (FNAC) based on the risk factors for thyroid cancer [21]. They recommended that FNAC should be performed in nodules larger than 5 mm, even if in patients at a high risk for thyroid cancer or with malignant features on neck USG [21]. For these reasons, physicians might have started to perform examinations less frequently, not only for thyroid nodules and cancer, but also for thyroid dysfunction. Ahn and Welch [22] reported that the number of operations for thyroid cancer decreased after screening for thyroid cancer with USG was discouraged in March 2014. However, the current study showed that the incidence of thyroid nodules, hypothyroidism, and hyperthyroidism decreased starting in 2013.
- Recently, MMI became the most frequently prescribed antithyroid drug among the three types of antithyroid drugs (PTU, MMI, and CAMZ). PTU was the most commonly used drug for patients with hyperthyroidism before 2009, but MMI overtook PTU in 2010. The U.S. Food and Drug Administration added a new boxed warning to the label for PTU about severe liver injury in 2010, because PTU can lead to potentially fatal fulminant hepatic necrosis [232425]. The American Thyroid Association and American Association of Clinical Endocrinologists guidelines, as well as the KTA guidelines, recommended using MMI to treat hyperthyroidism, except within the first trimester of pregnancy and in patients experiencing thyrotoxic crisis [2526]. For these reasons, the trends in physician's prescriptions changed and MMI became the most frequently prescribed antithyroid drug in 2015.
- This retrospective cohort study has several limitations. Because of its population-based design, this study could be subject to several biases, including coding bias, selection bias, and the effects of confounding factors. A possible discrepancy existed between the actual diagnosis and claim data because the NHIS database depends on the diagnostic code and prescription submitted on the physician's claim. In addition, the NHIS database does not contain information about prescriptions not covered through insurance. Data from thyroid function tests were not available in this study. We were not able to include subjects who had hypothyroidism and did not receive medication or those with hyperthyroidism who did not receive treatment. We could not evaluate the causative disease of hypothyroidism and hyperthyroidism. We excluded subjects diagnosed with thyroid cancer, even if they had been treated for thyroid dysfunction or had thyroid nodules. This could have led us to underestimate the prevalence and incidence of these thyroid diseases. Nevertheless, this was the first study of the prevalence and annual incidence of thyroid nodules in the entire Korean population. We investigated the prevalence and annual incidence of hypothyroidism and hyperthyroidism, taking into account recent changes and including the current status of patients receiving treatment.
- In conclusion, the prevalence of thyroid nodules, hypothyroidism in patients taking thyroid hormone, and hyperthyroidism in patients undergoing treatment was 15.82/1,000 population, 15.94/1,000 population, and 2.76/1,000 population, respectively, in Korea in 2015 using the NHI database after excluding subjects with thyroid cancer. All these diseases were more prevalent among women than among men. The number of incident cases of these thyroid diseases steadily increased from 2006 to 2012, and then decreased through 2015. The incidence of thyroid nodules, hypothyroidism in patients taking thyroid hormone, and hyperthyroidism in patients undergoing treatment was 6.79/1,000 population, 1.76/1,000 population, and 0.55/1,000 population in Korea in 2015. MMI is now the most frequently prescribed antithyroid drug in Korea.
DISCUSSION
-
Acknowledgements
- This work was supported by the Korean Endocrine Society of EnM Research Award 2017.
ACKNOWLEDGMENTS
-
AUTHOR CONTRIBUTIONS: Conception and design: W.Y.L., H.K. Development of methodology: H.K., J.J., K.D.H., Y.G.P. Acquisition of data (provided animals, acquired and managed patients, provided facilities, etc.): J.J., K.D.H., Y.G.P. Analysis and interpretation of data (e.g., statistical analysis, biostatistics, computational analysis): J.J., K.D.H., Y.G.P. Writing, review, and/or revision of the manuscript: H.K., J.H.C., D.Y.L., J.M.H. Administrative, technical, or material support (i.e., reporting or organizing data, constructing databases): K.D.H., H.K. Study supervision: S.E.P., E.J.R., W.Y.L.
-
CONFLICTS OF INTEREST: No potential conflict of interest relevant to this article was reported.
Article information
- 1. Chaker L, Bianco AC, Jonklaas J, Peeters RP. Hypothyroidism. Lancet 2017;390:1550–1562. ArticlePubMedPMC
- 2. De Leo S, Lee SY, Braverman LE. Hyperthyroidism. Lancet 2016;388:906–918. ArticlePubMedPMC
- 3. Mitchell J, Parangi S. The thyroid incidentaloma: an increasingly frequent consequence of radiologic imaging. Semin Ultrasound CT MR 2005;26:37–46. ArticlePubMed
- 4. Moon JH, Hyun MK, Lee JY, Shim JI, Kim TH, Choi HS, et al. Prevalence of thyroid nodules and their associated clinical parameters: a large-scale, multicenter-based health checkup study. Korean J Intern Med 2017 7 07 [Epub]. ArticlePDF
- 5. Shin J, Kim MH, Yoon KH, Kang MI, Cha BY, Lim DJ. Relationship between metabolic syndrome and thyroid nodules in healthy Koreans. Korean J Intern Med 2016;31:98–105. ArticlePubMedPDF
- 6. Liu Y, Lin Z, Sheng C, Zhu Y, Huang Y, Zhong N, et al. The prevalence of thyroid nodules in northwest China and its correlation with metabolic parameters and uric acid. Oncotarget 2017;8:41555–41562. ArticlePubMedPMC
- 7. Guo H, Sun M, He W, Chen H, Li W, Tang J, et al. The prevalence of thyroid nodules and its relationship with metabolic parameters in a Chinese community-based population aged over 40 years. Endocrine 2014;45:230–235. ArticlePubMedPDF
- 8. Hollowell JG, Staehling NW, Flanders WD, Hannon WH, Gunter EW, Spencer CA, et al. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab 2002;87:489–499. ArticlePubMed
- 9. Suk JH, Kim TY, Kim MK, Kim WB, Kim HK, Jeon SH, et al. Prevalence of ultrasonographically-detected thyroid nodules in adults without previous history of thyroid disease. J Korean Endocr Soc 2006;21:389–393.Article
- 10. Kim WJ, Kim JH, Park DW, Lee CB, Park YS, Kim DS, et al. Prevalence of thyroid nodules detected by ultrasonography in adults for health check-ups and analysis of fine needle aspiration cytology. J Korean Endocr Soc 2008;23:413–419.Article
- 11. Kim JH, Park SJ, Kim SE, Lee KH, Cho IK, Jang SI, et al. Prevalence of thyroid nodules detected by ultrasonography in adult men attending health check-ups. J Korean Endocr Soc 2007;22:112–117.Article
- 12. Peeters RP. Subclinical hypothyroidism. N Engl J Med 2017;376:2556–2565. ArticlePubMed
- 13. Smith TJ, Hegedus L. Graves' disease. N Engl J Med 2016;375:1552–1565. ArticlePubMed
- 14. Garmendia Madariaga A, Santos Palacios S, Guillen-Grima F, Galofre JC. The incidence and prevalence of thyroid dysfunction in Europe: a meta-analysis. J Clin Endocrinol Metab 2014;99:923–931. ArticlePubMedPDF
- 15. Asvold BO, Vatten LJ, Bjoro T. Changes in the prevalence of hypothyroidism: the HUNT Study in Norway. Eur J Endocrinol 2013;169:613–620. ArticlePubMed
- 16. Kim WG, Kim WB, Woo G, Kim H, Cho Y, Kim TY, et al. Thyroid stimulating hormone reference range and prevalence of thyroid dysfunction in the Korean population: Korea National Health and Nutrition Examination Survey 2013 to 2015. Endocrinol Metab (Seoul) 2017;32:106–114. ArticlePubMedPMC
- 17. Seo GH, Chung JH. Incidence and prevalence of overt hypothyroidism and causative diseases in Korea as determined using claims data provided by the Health Insurance Review and Assessment Service. Endocrinol Metab (Seoul) 2015;30:288–296. ArticlePubMedPMC
- 18. Seo GH, Kim SW, Chung JH. Incidence & prevalence of hyperthyroidism and preference for therapeutic modalities in Korea. J Korean Thyroid Assoc 2013;6:56–63.ArticlePDF
- 19. Chang MY, Han DH, Moon IJ, Kim ST, Kim DY, Lee CH, et al. Assessment of allergic rhinitis websites in Korea. Clin Exp Otorhinolaryngol 2010;3:32–36. ArticlePubMedPMCPDF
- 20. Seong SC, Kim YY, Khang YH, Park JH, Kang HJ, Lee H, et al. Data resource profile: the National Health Information database of the National Health Insurance Service in South Korea. Int J Epidemiol 2017;46:799–800. PubMed
- 21. Yi KH, Park YJ, Koong SS, Kim JH, Na DG, Ryu JS, et al. Revised Korean Thyroid Association management guidelines for patients with thyroid nodules and thyroid cancer. Endocrinol Metab 2010;25:270–297.Article
- 22. Ahn HS, Welch HG. South Korea's thyroid-cancer “epidemic”: turning the tide. N Engl J Med 2015;373:2389–2390. ArticlePubMed
- 23. Rivkees SA, Mattison DR. Ending propylthiouracil-induced liver failure in children. N Engl J Med 2009;360:1574–1575.Article
- 24. Bahn RS, Burch HS, Cooper DS, Garber JR, Greenlee CM, Klein IL, et al. The role of propylthiouracil in the management of Graves' disease in adults: report of a meeting jointly sponsored by the American Thyroid Association and the Food and Drug Administration. Thyroid 2009;19:673–674. ArticlePubMed
- 25. Bahn Chair RS, Burch HB, Cooper DS, Garber JR, Greenlee MC, Klein I, et al. Hyperthyroidism and other causes of thyrotoxicosis: management guidelines of the American Thyroid Association and American Association of Clinical Endocrinologists. Thyroid 2011;21:593–646. ArticlePubMed
- 26. Moon JH, Yi KH. The diagnosis and management of hyperthyroidism in Korea: consensus report of the Korean Thyroid Association. Endocrinol Metab (Seoul) 2013;28:275–279. ArticlePubMedPMC
References
Changes in the prescription patterns of antithyroid drug in patients with hyperthyroidism. CAMZ, carbimazole; MMI, methimazole; PTU, propylthiouracil.
Prevalence of Thyroid Nodules in 2015
Prevalence of Hypothyroidism in Patients Taking Thyroid Hormone in 2015
Prevalence of Hyperthyroidism in Patients Undergoing Treatment in 2015
Figure & Data
References
Citations

- New-onset atrial fibrillation in seropositive rheumatoid arthritis: association with disease-modifying anti-rheumatic drugs treatment
Hyung Woo Kim, Minkyung Han, Inkyung Jung, Sung Soo Ahn
Rheumatology.2024; 63(3): 630. CrossRef - Nonalcoholic Fatty Liver Disease and the Risk of Thyroid Cancer Among Young Adults in South Korea
Hyemi Kwon, Kyung-Do Han, Sun Joon Moon, Se Eun Park, Eun-Jung Rhee, Won-Young Lee
The Journal of Clinical Endocrinology & Metabolism.2024; 109(3): e1095. CrossRef - Endocrine and metabolic comorbidities in primary cicatricial alopecia: A nationwide population‐based study
Da‐Ae Yu, Seong Rae Kim, Soo Ick Cho, Ohsang Kwon
The Journal of Dermatology.2024; 51(3): 429. CrossRef - Risk of non-thyroidal autoimmune diseases in patients with Graves’ disease: a nationwide retrospective cohort study
Seo Young Sohn, Jiyeon Ahn, Min Kyung Lee, Jae Hyuk Lee, Ji-Won Kwon, Ji-Min Kweon, Ju-Yeun Lee
Rheumatology.2024;[Epub] CrossRef - Cancer Risk in Graves Disease with Radioactive131I Treatment: A Nationwide Cohort Study
Kyeong Jin Kim, Jimi Choi, Kyoung Jin Kim, Eyun Song, Ji Hee Yu, Nam Hoon Kim, Hye Jin Yoo, Ji A Seo, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Sin Gon Kim
Journal of Nuclear Medicine.2024; : jnumed.123.266531. CrossRef - Long-term effect of thyrotropin-binding inhibitor immunoglobulin on atrial fibrillation in euthyroid patients
Jung-Chi Hsu, Kang-Chih Fan, Ting-Chuan Wang, Shu-Lin Chuang, Ying-Ting Chao, Ting-Tse Lin, Kuan-Chih Huang, Lian-Yu Lin, Lung-Chun Lin
Endocrine Practice.2024;[Epub] CrossRef - Myotonic dystrophy type 1 in South Korea: a comprehensive analysis of cancer and comorbidity risks
Incheol Seo, Jin-Mo Park
Neurological Sciences.2024;[Epub] CrossRef - Association of ITM2A rs1751094 polymorphism on X chromosome in Korean pediatric patients with autoimmune thyroid disease
Won K. Cho, In‐Cheol Baek, Sung E. Kim, Mirae Kim, Tai‐Gyu Kim, Byung‐Kyu Suh
Immunity, Inflammation and Disease.2023;[Epub] CrossRef - Preoperative Risk Stratification of Follicular-patterned Thyroid Lesions on Core Needle Biopsy by Histologic Subtyping and RAS Variant-specific Immunohistochemistry
Meejeong Kim, Sora Jeon, Chan Kwon Jung
Endocrine Pathology.2023; 34(2): 247. CrossRef - Cancer and Mortality Risks of Graves’ Disease in South Korea Based on National Data from 2010 to 2019
Young Ju Choi, Kyungdo Han, Won Kyoung Cho, Min Ho Jung, Byung-Kyu Suh
Clinical Epidemiology.2023; Volume 15: 535. CrossRef - Acromegaly and the long-term fracture risk of the vertebra and hip: a national cohort study
Hyemi Kwon, Kyung-Do Han, Bong-Sung Kim, Sun Joon Moon, Se Eun Park, Eun-Jung Rhee, Won-Young Lee
Osteoporosis International.2023; 34(9): 1591. CrossRef - Association of Thyroid Hormone Medication Adherence With Risk of Dementia
Saemi Han, Seogsong Jeong, Seulggie Choi, Sun Jae Park, Kyae Hyung Kim, Gyeongsil Lee, Yoosun Cho, Joung Sik Son, Sang Min Park
The Journal of Clinical Endocrinology & Metabolism.2023; 109(1): e225. CrossRef - Increased risk of incident gout in patients with hyperthyroidism: a nationwide retrospective cohort study
Ju-Yeun Lee, So-Yeon Park, Seo Young Sohn
Rheumatology International.2023; 44(3): 451. CrossRef - The Current Status of Hyperthyroidism in Korea
Hyemi Kwon
Endocrinology and Metabolism.2023; 38(4): 392. CrossRef - Prevalence, Treatment Status, and Comorbidities of Hyperthyroidism in Korea from 2003 to 2018: A Nationwide Population Study
Hwa Young Ahn, Sun Wook Cho, Mi Young Lee, Young Joo Park, Bon Seok Koo, Hang-Seok Chang, Ka Hee Yi
Endocrinology and Metabolism.2023; 38(4): 436. CrossRef - Comprehensive analysis of chemokine gene polymorphisms in Korean children with autoimmune thyroid disease
Chungwoo Shin, In-Cheol Baek, Won Kyoung Cho, Tai-Gyu Kim, Byung-Kyu Suh
Scientific Reports.2023;[Epub] CrossRef - Analysis of the status of treatment of benign thyroid diseases — a public health problem aggravated in the COVID-19 pandemic era
Giulianno Molina Melo, Antonio José Gonçalves, Fernando Walder, Carolina Ferraz, Murilo Catafesta Neves, Marcio Abrahão, Onivaldo Cervantes
Brazilian Journal of Otorhinolaryngology.2022; 88(6): 982. CrossRef - Graves’ disease and the risk of Parkinson’s disease: a Korean population-based study
Yoon Young Cho, Bongseong Kim, Dong Wook Shin, Jinyoung Youn, Ji Oh Mok, Chul-Hee Kim, Sun Wook Kim, Jae Hoon Chung, Kyungdo Han, Tae Hyuk Kim
Brain Communications.2022;[Epub] CrossRef - Graves’ Disease and the Risk of End-Stage Renal Disease: A Korean Population-Based Study
Yoon Young Cho, Bongseong Kim, Dong Wook Shin, Hye Ryoun Jang, Bo-Yeon Kim, Chan-Hee Jung, Jae Hyeon Kim, Sun Wook Kim, Jae Hoon Chung, Kyungdo Han, Tae Hyuk Kim
Endocrinology and Metabolism.2022; 37(2): 281. CrossRef - Incidence of hypothyroidism after treatment for breast cancer: A Korean population-based study
Jongmoo Park, Choongrak Kim, Yongkan Ki, Wontaek Kim, Jiho Nam, Donghyun Kim, Dahl Park, Hosang Jeon, Dong Woon Kim, Ji Hyeon Joo, Claudio Andaloro
PLOS ONE.2022; 17(6): e0269893. CrossRef - Genome-wide association study of hyperthyroidism based on electronic medical record from Taiwan
Ting-Yuan Liu, Wen-Ling Liao, Tzu-Yuan Wang, Chia-Jung Chan, Jan-Gowth Chang, Yu-Chia Chen, Hsing-Fang Lu, Hsien-Hui Yang, Shih-Yin Chen, Fuu-Jen Tsai
Frontiers in Medicine.2022;[Epub] CrossRef - Graves’ disease, its treatments, and the risk of atrial fibrillation: A Korean population-based study
Yoon Young Cho, Bongseong Kim, Dughyun Choi, Chul-Hee Kim, Dong Wook Shin, Jee Soo Kim, Seung-Jung Park, Sun Wook Kim, Jae Hoon Chung, Kyungdo Han, Tae Hyuk Kim
Frontiers in Endocrinology.2022;[Epub] CrossRef - Risk of autoimmune diseases in recurrent aphthous ulcer patients: A nationwide population study
Young Chan Lee, Su Jin Jeong, Young‐Gyu Eun, Ran Song, In‐Hwan Oh
Oral Diseases.2021; 27(6): 1443. CrossRef - Hyperthyroidism Prevalence in China After Universal Salt Iodization
Chuyuan Wang, Yongze Li, Di Teng, Xiaoguang Shi, Jianming Ba, Bing Chen, Jianling Du, Lanjie He, Xiaoyang Lai, Yanbo Li, Haiyi Chi, Eryuan Liao, Chao Liu, Libin Liu, Guijun Qin, Yingfen Qin, Huibiao Quan, Bingyin Shi, Hui Sun, Xulei Tang, Nanwei Tong, Gui
Frontiers in Endocrinology.2021;[Epub] CrossRef - Comorbidity network analysis related to obesity in middle-aged and older adults: findings from Korean population-based survey data
Hye Ah Lee, Hyesook Park
Epidemiology and Health.2021; 43: e2021018. CrossRef - Prevalence of Hyperthyroidism and Hypothyroidism and its Correlation with Serum Antithyroglobulin among patients in Kirkuk-Iraq
Sabah Mohammed Salih, Wijdan Abdullameer Kamel, Mohammed Talat Abbas, Kasim Sakran Abass
Journal Of Advanced Pharmacy Education And Research.2021; 11(2): 57. CrossRef - A nationwide study of patients with monoclonal gammopathy of undetermined significance with a 10-year follow-up in South Korea
Ka-Won Kang, Ji Eun Song, Byung-Hyun Lee, Min Ji Jeon, Eun Sang Yu, Dae Sik Kim, Se Ryeon Lee, Hwa Jung Sung, Chul Won Choi, Yong Park, Byung Soo Kim
Scientific Reports.2021;[Epub] CrossRef - Incidence and Mortality of Myocardial Infarction and Stroke in Patients with Hyperthyroidism: A Nationwide Cohort Study in Korea
Hyun Jung Kim, Taeuk Kang, Min Ji Kang, Hyeong Sik Ahn, Seo Young Sohn
Thyroid.2020; 30(7): 955. CrossRef - Vitamin D supplementation does not prevent the recurrence of Graves’ disease
Yoon Young Cho, Yun Jae Chung
Scientific Reports.2020;[Epub] CrossRef - Binding and Activity of Tetrabromobisphenol A Mono-Ether Structural Analogs to Thyroid Hormone Transport Proteins and Receptors
Xiao-Min Ren, Linlin Yao, Qiao Xue, Jianbo Shi, Qinghua Zhang, Pu Wang, Jianjie Fu, Aiqian Zhang, Guangbo Qu, Guibin Jiang
Environmental Health Perspectives.2020;[Epub] CrossRef - Epidemiology of metabolic syndrome and its components in Chinese patients with a range of thyroid-stimulating hormone concentrations
Kun Tang, Qiao Zhang, Nian-chun Peng, Miao Zhang, Shu-jing Xu, Hong Li, Ying Hu, Chun-ju Xue, Li-xin Shi
Journal of International Medical Research.2020; 48(11): 030006052096687. CrossRef - The Association of Overt and Subclinical Hyperthyroidism with the Risk of Cardiovascular Events and Cardiovascular Mortality: Meta-Analysis and Systematic Review of Cohort Studies
Seo Young Sohn, Eunyoung Lee, Min Kyung Lee, Jae Hyuk Lee
Endocrinology and Metabolism.2020; 35(4): 786. CrossRef - Prevalence of Thyroid Disease in Patients Surgically Treated for Pituitary Disease
Kim, Cho, Ku, Jung, Moon, Kim, Shin, Kim, Lee
Journal of Clinical Medicine.2019; 8(8): 1142. CrossRef - Association of Thyroid-Stimulating Hormone and Thyroid Hormones with Cardiometabolic Risk Factors in Euthyroid Children and Adolescents Aged 10–18 Years: A Population-Based Study
Cheol Gyu Ma, Young Suk Shim
Scientific Reports.2019;[Epub] CrossRef - Weight change is significantly associated with risk of thyroid cancer: A nationwide population-based cohort study
Hyemi Kwon, Kyung-Do Han, Cheol-Young Park
Scientific Reports.2019;[Epub] CrossRef - Evaluation of the relationship of subclinical hypothyroidism with metabolic syndrome and its components in adolescents: a population-based study
Min-Kyung Lee, Yoo Mee Kim, Seo-Young Sohn, Jae-Hyuk Lee, Young Jun Won, Se Hwa Kim
Endocrine.2019; 65(3): 608. CrossRef - Autoimmune thyroiditis and central serous chorioretinopathy may have a relation
Brijesh Takkar, Harsha Saxena, Anubha Rathi, Rekha Singh
Medical Hypotheses.2018; 121: 180. CrossRef
- Figure
- Related articles
-
- Association between Smoking Status and the Risk of Hip Fracture in Patients with Type 2 Diabetes: A Nationwide Population-Based Study
- Long-Term Cumulative Exposure to High γ-Glutamyl Transferase Levels and the Risk of Cardiovascular Disease: A Nationwide Population-Based Cohort Study
- Risk of Cause-Specific Mortality across Glucose Spectrum in Elderly People: A Nationwide Population-Based Cohort Study
- Prevalence, Treatment Status, and Comorbidities of Hyperthyroidism in Korea from 2003 to 2018: A Nationwide Population Study
- Predicting the Risk of Insulin-Requiring Gestational Diabetes before Pregnancy: A Model Generated from a Nationwide Population-Based Cohort Study in Korea

 KES
KES


 PubReader
PubReader ePub Link
ePub Link Cite
Cite