Articles
- Page Path
- HOME > Endocrinol Metab > Volume 31(3); 2016 > Article
-
Review ArticleThe Revised 2016 Korean Thyroid Association Guidelines for Thyroid Nodules and Cancers: Differences from the 2015 American Thyroid Association Guidelines
-
Ka Hee Yi

-
Endocrinology and Metabolism 2016;31(3):373-378.
DOI: https://doi.org/10.3803/EnM.2016.31.3.373
Published online: September 26, 2016
Department of Internal Medicine, Seoul Metropolitan Government Seoul National University Boramae Medical Center, Seoul National University College of Medicine, Seoul, Korea.
- Corresponding author: Ka Hee Yi. Department of Internal Medicine, Seoul Metropolitan Government Seoul National University Boramae Medical Center, Seoul National University College of Medicine, 20 Boramae-ro 5-gil, Dongjak-gu, Seoul 07061, Korea. Tel: +82-2-870-3203, Fax: +82-2-870-3866, khyi@snu.ac.kr
Copyright © 2016 Korean Endocrine Society
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- Increased detection of thyroid nodules using high-resolution ultrasonography has resulted in a world-wide increase in the incidence of differentiated thyroid cancer (DTC). Despite the steep increase in its incidence, the age-standardized mortality rate of thyroid cancer has remained stable, which leads toward a trend of more conservative treatment. The latest American Thyroid Association (ATA) guidelines for thyroid nodules and thyroid cancer revised in 2015 suggested that fine needle aspiration biopsy should be performed for thyroid nodules larger than 1 cm and lobectomy might be sufficient for 1 to 4 cm intrathyroidal DTC. In addition, active surveillance instead of immediate surgical treatment was also recommended as a treatment option for papillary thyroid microcarcinoma based on the results of a few observational studies from Japan. The Korean Thyroid Association (KTA) has organized a task force team to develop revised guidelines for thyroid nodules and DTC after an extensive review of articles and intense discussion on whether we should accept the changes in the 2015 ATA guidelines. This paper introduces and discusses the updated major issues and differences in the ATA and the KTA guidelines.
- Thyroid nodules have become a very common clinical problem after the introduction of high resolution ultrasonography (US) in the 2000s that can detect nonpalpable nodules (incidentalomas). The prevalence of thyroid nodules detected by US has been reported as 19% to 68% depending on the study population [1], which resulted in an increase in the incidence of thyroid cancer since 5% to 15% of the identified nodules are malignant. Despite the steep increase in its incidence, the age-standardized mortality rate of thyroid cancer has remained stable [2], which leads to a shift toward more conservative approaches to the diagnosis and treatment of this disease. In the latest American Thyroid Association (ATA) guidelines for thyroid nodules and differentiated thyroid cancer (DTC) published in early 2016 [3], fine needle aspiration (FNA) is recommended for thyroid nodules larger than 1 cm even with highly suspicious sonographic features while lobectomy might be sufficient for 1 to 4 cm intrathyroidal DTC to avoid complications from total thyroidectomy. In addition, active surveillance instead of immediate surgical treatment is also recommended as a treatment option for papillary thyroid microcarcinoma (PTMC) based on the results of a few observational studies from Japan [45]. The Korean Thyroid Association (KTA) has organized a task force team to develop revised guidelines for thyroid nodules and thyroid cancer after an extensive review of articles including guidelines from other endocrine or thyroid associations and intense discussion on whether we should accept the changes in the 2015 ATA guidelines. The product will be published as the revised KTA guidelines for thyroid nodules and DTC later this year. Here, we focus on three major issues in the revised KTA: (1) size criteria for FNA; (2) active surveillance as one of the treatment options for PTMC; and (3) extent of surgery including surgery for grey zone tumors.
INTRODUCTION
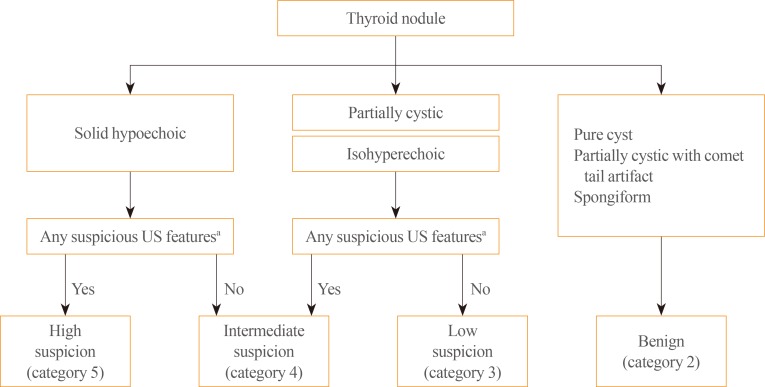
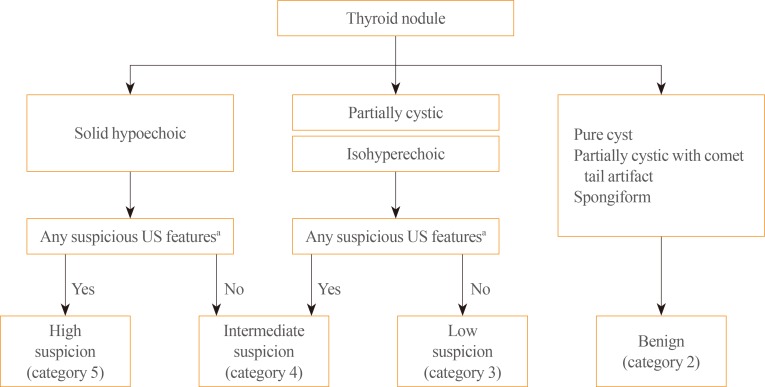
- The change in size criteria for FNA has drawn keen attention after the publication of the clinical guidelines for thyroid nodules. In the 2015 ATA guidelines, ultrasound stratification of thyroid nodules according to the estimated risk of malignancy was introduced (Table 1). FNA was recommended for nodules ≥1 cm, rather than >0.5 cm as in the 2009 ATA guidelines, that show a high suspicion US pattern, i.e., solid hypoechoic nodules with one or more of the following features: irregular margins, microcalcifications, taller than wide shape, extrathyroidal extension, and rim calcifications with small extrusive soft tissue components. The size criteria for intermediate (≥1.0 cm), low (≥1.5 cm), and very low suspicion (≥2.0 cm) did not drastically change. However, they strongly recommended against FNA for nodules with a benign pattern (purely cystic) and the nodules that do not meet the FNA criteria. The high suspicion sonographic features also changed; extrathyroidal extension and rim calcifications with small extrusive soft tissue components are now regarded as new suspicious features; however, hypoechogenicity and increased nodular vascularity have been excluded. More than half of benign nodules are hypoechoic in US especially when their size is small which makes nodule hypoechogenicity less specific [6]. In the 2010 KTA guideline, intranodular hypervascularity has already been excluded from highly suspicious patterns based on the result reported by Korean radiologists showing that intranodular vascularity was higher in benign nodules than in papillary thyroid cancer (PTC) [7]. The ATA also cited this result as evidence to exclude increased vascularity from high suspicion sonographic patterns. The Korean Society of Thyroid Radiology also developed a new clinically feasible US risk-stratification system, the Korean Thyroid Imaging Reporting and Data System (K-TIRADS), primarily based on the solidity and echogenicity of thyroid nodules by analyzing 2,000 nodules including 454 nodules that were pathologically proven as malignant [89]. Major differences in risk stratification by US between the K-TIRADS and ATA were: (1) isohyperechoic or partially cystic nodules with any suspicious features were classified as intermediate suspicion (category 4), and (2) nodules of very low suspicion and in the benign group in the ATA guidelines were combined and categorized as benign (category 2) in the K-TIRADS (Table 2, Fig. 1). Korean radiologists recommend FNA for category 5 nodules when the size is ≥1.0 cm; however, the size criteria is lowered to >0.5 cm in the presence of extrathyroidal extensions, cervical lymph node or distant metastasis, trachea or recurrent laryngeal nerve invasion, and tumor progression.
- What is the evidence for changing the size criteria for high suspicion nodules from >0.5 cm in the 2009 ATA guidelines to ≥1.0 cm in the 2015 ATA guidelines? In 2009, they referred to a study showing that PTCs >0.5 cm had significantly higher lymph node metastasis and recurrence [10]. While in 2015, they described that PTMCs, the PTCs ≤1 cm size have disease-specific mortality rates reported to be <1%, locoregional recurrence rates of 2% to 6%, and distant recurrence rates of 1% to 2% based on Mazzaferri's review [11]. They also insisted that these excellent outcomes are more related to the indolent nature of the disease rather than to the effectiveness of treatment. Furthermore, they suggested that a conservative approach of active surveillance management may be appropriate as an alternative to FNA in selected patients. However, FNA for US high suspicion nodules ≤1 cm size is appropriate considering that: (1) unnecessary long-term follow-up study for benign nodules with a high suspicion US pattern (approximately 20% to 40% of nodules with a high suspicion pattern) can be avoided; (2) a small percentage of patients with PTMC present with clinically significant regional or distant metastases; and (3) active surveillance for cytologically proven PTMC is also possible. For these reasons, the KTA guidelines will adopt the K-TIRADS recommendations to determine FNA indication instead of using the ATA system.
SIZE CRITERIA FOR FINE NEEDLE ASPIRATION
- When a cytology result is diagnostic for thyroid malignancy, active surveillance as well as immediate surgery was recommended in the 2015 ATA guidelines as a treatment option for patients with (1) very low risk of tumors clinically (without local invasion or metastasis) or cytologically (no evidence of aggressive disease), (2) high surgical risk because of comorbid conditions, or (3) a relatively short life expectancy. This recommendation is based on the results from two prospective clinical studies on active surveillance of patients with low risk PTMC from Japan started in the 1990s [45]. These studies enrolled 1,465 patients with biopsy-proven PTMCs that were not surgically removed and were followed for up to 15 years (average, 5 to 6 years). Most patients showed stable tumor size after an average follow-up of 60 months whereas 5% to 7% of patients showed tumor enlargement (>3 mm) by US on 5-year follow-up, and 8% showed this enlargement on 10-year follow-up. Additionally, 1% to 1.7% and 3.8% of patients at 5- and 10-year follow-up, respectively, showed evidence for lymph node metastases (Table 3). Furthermore, recurrence after delayed surgery was very rare (1/196 and 0/16) with an average of 6 years of follow-up. Interestingly, clinical progression (tumor growth or new lymph node metastasis) was related to patient age; younger patients (<40 years old) had a significantly higher progression rate (8.9%) than patients >60 years old (1.6%) [4]. Citing these results, the 2015 ATA guidelines suggested that active surveillance could be a treatment option for PTMC patients instead of immediate surgery. Until now, there are no reliable clinical features (including molecular tests) that can differentiate PTMC in patients who develop progressive disease from indolent PTMC that does not cause significant disease [121314151617]. Further studies are needed not only on the natural history of PTMC but also on the identification of markers indicating progressiveness or indolence in PTMC. The KTA will cautiously adopt active surveillance for selective PTMC patients as a treatment option, particularly for older patients.
ACTIVE SURVEILLANCE FOR PAPILLARY THYROID MICROCARCINOMA
- Surgery is the most important component of treatment for DTC, and the extent of surgery has been debated for a long time. In previous guidelines including the 2009 ATA guidelines, total thyroidectomy had been endorsed as the primary initial surgical treatment for DTCs >1 cm regardless of locoregional or distant metastases based on study results showing that total thyroidectomy improved survival and decreased recurrence [18]. Moreover, remnant ablation using radioactive iodine (RAI) which has been routinely performed to facilitate detection of recurrent or persistent disease during follow-up is much more efficient after total thyroidectomy. However, recent data have demonstrated that clinical outcomes are very similar following lobectomy or total thyroidectomy in patients with PTCs sized 1 to 2 cm and 2 to 4 cm [192021]. Furthermore, RAI remnant ablation has not been proven to be completely efficient and improve outcomes in low to intermediate risk patients, so total thyroidectomy to facilitate RAI therapy in these groups is needed in selective cases.
- Surgical complications are another factor supporting lobectomy instead of total thyroidectomy in the 2015 ATA guidelines. Postoperative hypoparathyroidism and recurrent laryngeal nerve injury are well-known surgical complications after total thyroidectomy. Surgical complication rates naturally correlate with surgical volumes [2223], although even in high volume surgeons (>100 thyroidectomies per year), complication rates were significantly higher after total thyroidectomy [24]. Based on this rationale, the 2015 ATA guidelines recommend (1) total thyroidectomy only for high risk patients with a tumor >4 cm and gross extrathyroidal extension (T4), clinical cervical nodes metastasis (cN1), or distant metastasis (M1); (2) either a bilateral or a unilateral thyroidectomy as an initial surgical treatment for DTC patients with 1 to 4 cm tumors without extrathyroidal extension and without clinical node metastasis (cN0): lobectomy alone may be sufficient for low-risk DTC patients; and (3) lobectomy as an initial treatment for patients with <1 cm tumors without extrathyroidal extension and cN0. However, in actual clinical practice, 1 to 4 cm DTCs without extrathyroidal extension and without clinical node metastasis (cN0) are so rare that total thyroidectomy would be necessary for patients with tumors in these ranges. Moreover, in Korea, surgical volume is much higher and postoperative complication rates are reported to be lower compared to other countries. The KTA guidelines flexibly accept the surgical extent for DTCs recommended by the ATA.
SURGICAL EXTENT FOR DIFFERENTIATED THYROID CANCER
- DTCs, especially PTMCs, have excellent prognosis with very low mortality, which makes it difficult to determine the most efficient treatment options based on prospective, randomized controlled studies. Many of the published guidelines for the management of thyroid nodules and DTCs were necessarily based on retrospective experiential reviews. In the 2015 ATA guidelines, more conservative approaches to the diagnosis and treatment of DTCs were recommended because it was not certain if aggressive treatments were clearly beneficial rather than harmful for patients. The KTA will 'flexibly' and 'selectively' adopt the 2015 ATA guidelines such as active surveillance for PTMC patients and surgical extents for DTCs sized 1 to 4 cm; however, for FNA criteria according to US features, the K-TIRADS system will be used. Research to identify markers that can differentiate progressive from indolent PTMC as well as on the natural history of this disease should be continued in the future.
CONCLUSIONS
-
Acknowledgements
- The revised KTA guidelines for the management of thyroid nodules and thyroid cancer will be published this year in the Journal of Korean Thyroid Association.
ACKNOWLEDGMENTS
-
CONFLICTS OF INTEREST: No potential conflict of interest relevant to this article was reported.
Article information
- 1. Guth S, Theune U, Aberle J, Galach A, Bamberger CM. Very high prevalence of thyroid nodules detected by high frequency (13 MHz) ultrasound examination. Eur J Clin Invest 2009;39:699–706. ArticlePubMed
- 2. International Agency for Research on Cancer, World Health Organization. GLOBOCAN 2012: estimated cancer incidence, mortality and prevalence worldwide in 2012; Lyon: IARC; c2016. cited 2016 Aug 18. Available from: http://globocan.iarc.fr.
- 3. Haugen BR, Alexander EK, Bible KC, Doherty GM, Man-del SJ, Nikiforov YE, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 2016;26:1–133. ArticlePubMedPMC
- 4. Ito Y, Miyauchi A, Kihara M, Higashiyama T, Kobayashi K, Miya A. Patient age is significantly related to the progression of papillary microcarcinoma of the thyroid under observation. Thyroid 2014;24:27–34. ArticlePubMedPMC
- 5. Sugitani I, Toda K, Yamada K, Yamamoto N, Ikenaga M, Fujimoto Y. Three distinctly different kinds of papillary thyroid microcarcinoma should be recognized: our treatment strategies and outcomes. World J Surg 2010;34:1222–1231. ArticlePubMedPDF
- 6. Moon WJ, Jung SL, Lee JH, Na DG, Baek JH, Lee YH, et al. Benign and malignant thyroid nodules: US differentiation: multicenter retrospective study. Radiology 2008;247:762–770. ArticlePubMed
- 7. Moon HJ, Kwak JY, Kim MJ, Son EJ, Kim EK. Can vascularity at power Doppler US help predict thyroid malignancy? Radiology 2010;255:260–269. ArticlePubMed
- 8. Na DG, Baek JH, Sung JY, Kim JH, Kim JK, Choi YJ, et al. Thyroid imaging reporting and data system risk stratification of thyroid nodules: categorization based on solidity and echogenicity. Thyroid 2016;26:562–572. ArticlePubMed
- 9. Shin JH, Baek JH, Chung J, Ha EJ, Kim JH, Lee YH, et al. Ultrasonography diagnosis and imaging-based management of thyroid nodules: revised Korean Society of Thyroid Radiology consensus statement and recommendations. Korean J Radiol 2016;17:370–395. ArticlePubMedPMC
- 10. Noguchi S, Yamashita H, Uchino S, Watanabe S. Papillary microcarcinoma. World J Surg 2008;32:747–753. ArticlePubMedPMCPDF
- 11. Mazzaferri EL. Management of low-risk differentiated thyroid cancer. Endocr Pract 2007;13:498–512. ArticlePubMedPDF
- 12. Chow SM, Law SC, Chan JK, Au SK, Yau S, Lau WH. Papillary microcarcinoma of the thyroid: prognostic significance of lymph node metastasis and multifocality. Cancer 2003;98:31–40. ArticlePubMed
- 13. Hay ID, Hutchinson ME, Gonzalez-Losada T, McIver B, Reinalda ME, Grant CS, et al. Papillary thyroid microcarcinoma: a study of 900 cases observed in a 60-year period. Surgery 2008;144:980–987. ArticlePubMed
- 14. Roti E, degli Uberti EC, Bondanelli M, Braverman LE. Thyroid papillary microcarcinoma: a descriptive and meta-analysis study. Eur J Endocrinol 2008;159:659–673. ArticlePubMed
- 15. Giordano D, Gradoni P, Oretti G, Molina E, Ferri T. Treatment and prognostic factors of papillary thyroid microcarcinoma. Clin Otolaryngol 2010;35:118–124. ArticlePubMed
- 16. Ito Y, Miyauchi A, Inoue H, Fukushima M, Kihara M, Higashiyama T, et al. An observational trial for papillary thyroid microcarcinoma in Japanese patients. World J Surg 2010;34:28–35. ArticlePubMedPDF
- 17. Niemeier LA, Kuffner Akatsu H, Song C, Carty SE, Hodak SP, Yip L, et al. A combined molecular-pathologic score improves risk stratification of thyroid papillary microcarcinoma. Cancer 2012;118:2069–2077. ArticlePubMed
- 18. Bilimoria KY, Bentrem DJ, Ko CY, Stewart AK, Winchester DP, Talamonti MS, et al. Extent of surgery affects survival for papillary thyroid cancer. Ann Surg 2007;246:375–381. ArticlePubMedPMC
- 19. Haigh PI, Urbach DR, Rotstein LE. Extent of thyroidectomy is not a major determinant of survival in low- or high-risk papillary thyroid cancer. Ann Surg Oncol 2005;12:81–89. ArticlePubMedPDF
- 20. Nixon IJ, Ganly I, Patel SG, Palmer FL, Whitcher MM, Tuttle RM, et al. Thyroid lobectomy for treatment of well differentiated intrathyroid malignancy. Surgery 2012;151:571–579. ArticlePubMed
- 21. Adam MA, Pura J, Gu L, Dinan MA, Tyler DS, Reed SD, et al. Extent of surgery for papillary thyroid cancer is not associated with survival: an analysis of 61,775 patients. Ann Surg 2014;260:601–605. ArticlePubMedPMC
- 22. Kandil E, Noureldine SI, Abbas A, Tufano RP. The impact of surgical volume on patient outcomes following thyroid surgery. Surgery 2013;154:1346–1352. ArticlePubMed
- 23. Duclos A, Peix JL, Colin C, Kraimps JL, Menegaux F, Pattou F, et al. Influence of experience on performance of individual surgeons in thyroid surgery: prospective cross sectional multicentre study. BMJ 2012;344:d8041ArticlePubMedPMC
- 24. Hauch A, Al-Qurayshi Z, Randolph G, Kandil E. Total thyroidectomy is associated with increased risk of complications for low- and high-volume surgeons. Ann Surg Oncol 2014;21:3844–3852. ArticlePubMedPDF
References
Algorithm used in the Korean Thyroid Imaging Reporting and Data System for malignancy risk stratification based on solidity and echogenicity of thyroid nodules. Adapted from Shin et al. [9]. US, ultrasonography. aMicrocalcification, taller than wide shape, spiculated/microlobulated margin.
Sonographic Patterns, Risk of Malignancy, and FNA Guidance for Thyroid Nodules in the 2015 American Thyroid Association Guidelines
Adapted from Haugen et al., with permission from Mary Ann Liebert, Inc. [3].
FNA, fine needle aspiration; US, ultrasonography; ETE, extrathyroidal extension.
aThe estimate is derived from high volume centers, the overall risk of malignancy may be lower given the interobserver variability in sonography; bAspiration of the cyst may be considered for symptomatic or cosmetic drainage.
Malignancy Risk Stratification according to K-TIRADS and FNA Indications
Adapted from Shin et al. [9]. LV and HV indicate low and high cancer volume data, respectively. Solid hypoechoic nodules include solid nodules with marked or mild hypoechogenicity.
K-TIRADS, Korean Thyroid Imaging Reporting and Data System; FNA, fine needle aspiration; US, ultrasonography; LV, low volume; HV, high volume; NA, not applicable for FNA.
aFNA is indicated regardless of size and US feature of nodule in presence of poor prognostic factors including suspected lymph node metastasis by US or clinical evaluation, suspected extrathyroidal tumor extension, patients with diagnosed distant metastasis from thyroid cancer; bMicrocalcification, nonparallel orientation (taller-than-wide), spiculated/microlobulated margin; cMalignancy risk calculated from nodules excluding spongiform or partially cystic nodules with comet tail artifacts; dK-TIRADS 2 (benign category) includes partially cystic nodules with spongiform appearance or comet tail artifacts which do not have any suspicious US feature.
Results of Two Studies on Active Surveillance in Japan
| Variable | Ito et al. (2014) [4] | Sugitani et al. (2010) [5] |
|---|---|---|
| No. of patients | 1,235 | 230 |
| Mean follow-up duration, mo | 60 | 60 |
| Progression, % | ||
| Size enlargement >3 mm | ||
| 5 yr | 5 | 7 |
| 10 yr | 8 | |
| LN metastasis | ||
| 5 yr | 1.7 | 1 |
| 10 yr | 3.8 | |
| Recurrence after delayed Op | 1/191 | 0/16 |
Figure & Data
References
Citations

- Intraoperative pathologic evaluation of central compartment lymph nodes in patients undergoing lobectomy for unilateral papillary thyroid carcinoma
Hye Lim Bae, Jong-hyuk Ahn, JungHak Kwak, Hyun Soo Kim, Sang Gab Yoon, Jin Wook Yi, Su-jin Kim, Kyu Eun Lee
Asian Journal of Surgery.2024; 47(1): 360. CrossRef - Global scientific trends on thyroid disease in early 21st century: a bibliometric and visualized analysis
Mingyuan Song, Wei Sun, Qi Liu, Zhongqing Wang, Hao Zhang
Frontiers in Endocrinology.2024;[Epub] CrossRef - A Narrative Review of the 2023 Korean Thyroid Association Management Guideline for Patients with Thyroid Nodules
Eun Kyung Lee, Young Joo Park, Chan Kwon Jung, Dong Gyu Na
Endocrinology and Metabolism.2024; 39(1): 61. CrossRef - Lowering Barriers to Health Risk Assessments in Promoting Personalized Health Management
Hayoung Park, Se Young Jung, Min Kyu Han, Yeonhoon Jang, Yeo Rae Moon, Taewook Kim, Soo-Yong Shin, Hee Hwang
Journal of Personalized Medicine.2024; 14(3): 316. CrossRef - Prognostic Utility of Tumor Stage versus American Thyroid Association Risk Class in Thyroid Cancer
Arash Abiri, Jonathan Pang, Karthik R. Prasad, Khodayar Goshtasbi, Edward C. Kuan, William B. Armstrong, Yarah M. Haidar, Tjoson Tjoa
The Laryngoscope.2023; 133(1): 205. CrossRef - Active surveillance for PTMC warranted for the UK population?
Pavithran Maniam, Noah Harding, Lucy Li, Richard Adamson, Ashley Hay, Ian Nixon
Clinical Otolaryngology.2023; 48(1): 88. CrossRef - Cost-effectiveness of active surveillance versus early surgery for thyroid micropapillary carcinoma based on diagnostic and treatment norms in China
Min Lai, Miao Miao Zhang, Qing Qing Qin, Yu An, Yan Ting Li, Wen Zhen Yuan
Frontiers in Endocrinology.2023;[Epub] CrossRef - Biopsy strategies for intermediate and high suspicion thyroid nodules with macrocalcifications
Sungmok Kim, Jae Ho Shin, Yon Kwon Ihn
Current Medical Research and Opinion.2023; 39(2): 179. CrossRef - Active surveillance versus immediate surgery: A comparison of clinical and quality of life outcomes among patients with highly suspicious thyroid nodules 1 cm or smaller in China
Chunhao Liu, Hao Zhao, Yu Xia, Yue Cao, Liyang Zhang, Ya Zhao, Luying Gao, Ruifeng Liu, Yuewu Liu, Hongfeng Liu, Zhilan Meng, Shuzhou Liu, Ying Lu, Xiaoyi Li
European Journal of Surgical Oncology.2023; 49(9): 106917. CrossRef - SThy-Net: a feature fusion-enhanced dense-branched modules network for small thyroid nodule classification from ultrasound images
Abdulrhman H. Al-Jebrni, Saba Ghazanfar Ali, Huating Li, Xiao Lin, Ping Li, Younhyun Jung, Jinman Kim, David Dagan Feng, Bin Sheng, Lixin Jiang, Jing Du
The Visual Computer.2023; 39(8): 3675. CrossRef - Response to Letter to the Editor on Surgical Outcomes in Patients With Low-Risk Papillary Thyroid Microcarcinoma From MAeSTro Study: Immediate Operation Versus Delayed Operation Following Active Surveillance: A Multicenter Prospective Cohort Study
Hyeonuk Hwang, June Young Choi, Jae Hoon Moon, Eun Kyung Lee, Young Joo Park, Su-jin Kim, Yuh-Seog Jung
Annals of Surgery Open.2023; 4(3): e311. CrossRef - The Association of Pregnancy with Disease Progression in Patients Previously Treated for Differentiated Thyroid Cancer: A Propensity Score-Matched Retrospective Cohort Study
Xin Li, Wu-Cai Xiao, Fang Mei, Rui Shan, Shi-Bing Song, Bang-Kai Sun, He-Ling Bao, Jing Chen, Chun-Hui Yuan, Zheng Liu
Journal of Women's Health.2023; 32(11): 1174. CrossRef - Mortality rate and causes of death in papillary thyroid microcarcinoma
Jung Heo, Hyun Jin Ryu, Hyunju Park, Tae Hyuk Kim, Sun Wook Kim, Young Lyun Oh, Jae Hoon Chung
Endocrine.2023; 83(3): 671. CrossRef - Surgical Outcomes in Patients With Low-risk Papillary Thyroid Microcarcinoma From MAeSTro Study
Hyeonuk Hwang, June Young Choi, Hyeong Won Yu, Jae Hoon Moon, Ji-hoon Kim, Eun Kyung Lee, Yeo Koon Kim, Chang Yoon Lee, Sun Wook Cho, Eun-Jae Chung, Chang Hwan Ryu, Junsun Ryu, Ka Hee Yi, Do Joon Park, Kyu Eun Lee, Young Joo Park, Su-jin Kim, Yuh-Seog Jun
Annals of Surgery.2023; 278(5): e1087. CrossRef - US Predictors of Papillary Thyroid Microcarcinoma Progression at Active Surveillance
Ji Ye Lee, Ji-hoon Kim, Yeo Koon Kim, Chang Yoon Lee, Eun Kyung Lee, Jae Hoon Moon, Hoon Sung Choi, Hwangbo Yul, Sun Wook Cho, Su-jin Kim, Kyu Eun Lee, Do Joon Park, Young Joo Park
Radiology.2023;[Epub] CrossRef - Bilaterality as a Risk Factor for Recurrence in Papillary Thyroid Carcinoma
Hyeji Kim, Hyungju Kwon
Cancers.2023; 15(22): 5414. CrossRef - Clinical and molecular genetic analysis of cytologically uncertain thyroid nodules in patients with thyroid disease
Jindrich Lukas, Barbora Hintnausova, Vlasta Sykorova, Martin Syrucek, Marek Maly, David Lukas, Jaroslava Duskova
Biomedical Papers.2023;[Epub] CrossRef - Thyroid Papillary Microcarcinoma - Carcinoma with Clinically Benign Behaviour
Hitesh R Singhavi, Manish Mair, Burhanuddin Qayyumi, Arjun Singh, Pankaj Chaturvedi
Journal of Head & Neck Physicians and Surgeons.2023; 11(2): 95. CrossRef - Trends in Diagnosis of Noninvasive Follicular Thyroid Neoplasm With Papillarylike Nuclear Features and Total Thyroidectomies for Patients With Papillary Thyroid Neoplasms
Lisa Caulley, Antoine Eskander, Weining Yang, Edel Auh, Lydia Cairncross, Nancy L. Cho, Bahar Golbon, Subramania Iyer, Jeffrey C. Liu, Paul J. Lee, Brenessa Lindeman, Charles Meltzer, Nicole Molin, Alessandra Moore, Julia Noel, Halie Nozolino, Jesse Paste
JAMA Otolaryngology–Head & Neck Surgery.2022; 148(2): 99. CrossRef - What's in a Name? A Cost-Effectiveness Analysis of the Noninvasive Follicular Thyroid Neoplasm with Papillary-Like Nuclear Features' Nomenclature Revision
Vikas Mehta, Ankita Naraparaju, David Liao, Louise Davies, Bryan R. Haugen, Peter A. Kopp, Susan J. Mandel, Yuri E. Nikiforov, Douglas S. Ross, Jennifer J. Shin, R. Michael Tuttle, Gregory W. Randolph
Thyroid.2022; 32(4): 421. CrossRef - Clinical management of low-risk papillary thyroid microcarcinoma
Chie MASAKI, Kiminori SUGINO, Koichi ITO
Minerva Endocrinology.2022;[Epub] CrossRef - Can Active Surveillance Management be Developed for Patients With Low-Risk Papillary Thyroid Microcarcinoma? A Preliminary Investigation in a Chinese Population
Wen Liu, Weihan Cao, Zhizhong Dong, Ruochuan Cheng
Endocrine Practice.2022; 28(4): 391. CrossRef - Assessment of Radiofrequency Ablation for Papillary Microcarcinoma of the Thyroid
Sam P. J. van Dijk, Hannelore I. Coerts, Sabrina T. G. Gunput, Evert F. S. van Velsen, Marco Medici, Adriaan Moelker, Robin P. Peeters, Cornelis Verhoef, Tessa M. van Ginhoven
JAMA Otolaryngology–Head & Neck Surgery.2022; 148(4): 317. CrossRef - The Future of Thyroid Nodule Risk Stratification
Nydia Burgos, Naykky Singh Ospina, Jennifer A. Sipos
Endocrinology and Metabolism Clinics of North America.2022; 51(2): 305. CrossRef - Complication Rates of Total Thyroidectomy vs Hemithyroidectomy for Treatment of Papillary Thyroid Microcarcinoma
Vivian Hsiao, Tyler J. Light, Abdullah A. Adil, Michael Tao, Alexander S. Chiu, Mary Hitchcock, Natalia Arroyo, Sara Fernandes-Taylor, David O. Francis
JAMA Otolaryngology–Head & Neck Surgery.2022; 148(6): 531. CrossRef - Malignancy risk stratification of thyroid nodules smaller than 10 mm with ACR-TIRADS, K-TIRADS, and ATA-2015 guidelines: a prospective study
Mehrdad Nabahati, Zoleika Moazezi
Egyptian Journal of Radiology and Nuclear Medicine.2022;[Epub] CrossRef - Thyroglobulin-Based Risk Factor Repositioning for Determining Radioactive Iodine Activity in Patients with Papillary Thyroid Carcinoma: a Multicenter Retrospective Cohort Study
Subin Jeon, Seong Young Kwon, Sang-Woo Lee, Sang Kyun Bae
Nuclear Medicine and Molecular Imaging.2022; 56(4): 173. CrossRef - Quality of Life of Survivors of Thyroid Cancer Is Not Inferior to That in Subjects without Cancer: Long-Term after Over 5 Years
Jeongmin Lee, Youn-Ju Lee, Dong-Jun Lim, Jung-Min Lee, Sang-Ah Chang, Min-Hee Kim
Endocrinology and Metabolism.2022; 37(4): 664. CrossRef - Residual, regrowth, and new growth of radiofrequency ablation for benign thyroid nodules of different volumes: two-year follow-up results
Meng-Hsiang Chen, Wei-Che Lin, Sheng-Dean Luo, Pi-Ling Chiang, Yueh-Sheng Chen, Wei-Chih Chen, An-Ni Lin, Cheng-Kang Wang, Jung-Hwan Baek, Hsiu-Ling Chen
International Journal of Hyperthermia.2022; 39(1): 1172. CrossRef - Progression of Low-Risk Papillary Thyroid Microcarcinoma During Active Surveillance: Interim Analysis of a Multicenter Prospective Cohort Study of Active Surveillance on Papillary Thyroid Microcarcinoma in Korea
Eun Kyung Lee, Jae Hoon Moon, Yul Hwangbo, Chang Hwan Ryu, Sun Wook Cho, June Young Choi, Eun-Jae Chung, Woo-Jin Jeong, Yuh-Seog Jung, Junsun Ryu, Su-jin Kim, Min Joo Kim, Yeo Koon Kim, Chang Yoon Lee, Ji Ye Lee, Hyeong Won Yu, Jeong Hun Hah, Kyu Eun Lee,
Thyroid.2022; 32(11): 1328. CrossRef - Recent Changes in the Incidence of Thyroid Cancer in Korea between 2005 and 2018: Analysis of Korean National Data
Yun Mi Choi, Jiwoo Lee, Mi Kyung Kwak, Min Ji Jeon, Tae Yong Kim, Eun-Gyoung Hong, Won Bae Kim, Won Gu Kim
Endocrinology and Metabolism.2022; 37(5): 791. CrossRef - Strain Versus 2D Shear-Wave Elastography Parameters—Which Score Better in Predicting Thyroid Cancer?
Andreea Borlea, Ioan Sporea, Alexandru Popa, Mihnea Derban, Laura Taban, Dana Stoian
Applied Sciences.2022; 12(21): 11147. CrossRef - Estimating the risk of completion total thyroidectomy using real-world data to guide initial surgical decision-making for patients with clinical low-risk papillary thyroid carcinoma
Wen Liu, Xiangxiang Zhan, Zhizhong Dong, Yanjun Su, Jianming Zhang, Jun Qian, Yunhai Ma, Chang Diao, Ruochuan Cheng
Holistic Integrative Oncology.2022;[Epub] CrossRef - Rigorous radiofrequency ablation can completely treat low-risk small papillary thyroid carcinoma without affecting subsequent surgical management
Xinyang Li, Jie Li, Zhi Qiao, Lin Yan, Jing Xiao, Yingying Li, Mingbo Zhang, Yukun Luo
European Radiology.2022; 33(6): 4189. CrossRef - Whirling technique for thyroid fine needle aspiration biopsy: a preliminary study of effectiveness and safety
Jae Ho Shin, Seung Wan Han, Hyang Lim Lee, Yon Kwon Ihn
Ultrasonography.2021; 40(1): 147. CrossRef - Value of dual-phase, contrast-enhanced CT combined with ultrasound for the diagnosis of metastasis to central lymph nodes in patients with papillary thyroid cancer
Ying Liu, Sheng Li, Cuiju Yan, Caiyun He, Miao Yun, Min Liu, Jianhua Zhou, Longzhong Liu
Clinical Imaging.2021; 75: 5. CrossRef - Clinical outcomes of T4a papillary thyroid cancer with recurrent laryngeal nerve involvement: a retrospective analysis
Han-Seul Na, Hyun-Keun Kwon, Sung-Chan Shin, Yong-Il Cheon, Myeonggu Seo, Jin-Choon Lee, Eui-Suk Sung, Minhyung Lee, In-Joo Kim, Bo Hyun Kim, Byung-Joo Lee
Scientific Reports.2021;[Epub] CrossRef - Protocol for a Korean Multicenter Prospective Cohort Study of Active Surveillance or Surgery (KoMPASS) in Papillary Thyroid Microcarcinoma
Min Ji Jeon, Yea Eun Kang, Jae Hoon Moon, Dong Jun Lim, Chang Yoon Lee, Yong Sang Lee, Sun Wook Kim, Min-Hee Kim, Bo Hyun Kim, Ho-Cheol Kang, Minho Shong, Sun Wook Cho, Won Bae Kim
Endocrinology and Metabolism.2021; 36(2): 359. CrossRef - Thyroid nodules in childhood‐onset Hashimoto's thyroiditis: Frequency, risk factors, follow‐up course and genetic alterations of thyroid cancer
Yun Jeong Lee, Yeon Jin Cho, You Joung Heo, Eun‐Jae Chung, Young Hun Choi, Jong‐Il Kim, Young Joo Park, Choong Ho Shin, Young Ah Lee
Clinical Endocrinology.2021; 95(4): 638. CrossRef - Clinical implications of age and excellent response to therapy in patients with high‐risk differentiated thyroid carcinoma
Meihua Jin, Jonghwa Ahn, Yu‐Mi Lee, Tae‐Yon Sung, Dong Eun Song, Tae Yong Kim, Ki‐Wook Chung, Jin‐Sook Ryu, Won Bae Kim, Young Kee Shong, Min Ji Jeon, Won Gu Kim
Clinical Endocrinology.2021; 95(6): 882. CrossRef - Ecografía clínica de la glándula tiroides y del cuello
Pepa Bertrán Culla, David Teixidó Gimeno, Pere Guirado Vila
FMC - Formación Médica Continuada en Atención Primaria.2021; 28(7): 390. CrossRef - Active Surveillance as an Effective Management Option for Low-Risk Papillary Thyroid Microcarcinoma
Min Ji Jeon, Won Gu Kim, Tae Yong Kim, Young Kee Shong, Won Bae Kim
Endocrinology and Metabolism.2021; 36(4): 717. CrossRef - Clinical Effects of Microwave Ablation in the Treatment of Low-Risk Papillary Thyroid Microcarcinomas and Related Histopathological Changes
Chenya Lu, Xingjia Li, Xiaoqiu Chu, Ruiping Li, Jie Li, Jianhua Wang, Yalin Wang, Yang Xu, Guofang Chen, Shuhang Xu, Chao Liu
Frontiers in Endocrinology.2021;[Epub] CrossRef - Optimization of follow-up in patients with papillary thyroid cancer who show no evidence of disease 9–12 months after treatment
Fabian Nordell, Ghadir Hallal, Pernilla Asp, Martin Almquist
BJS Open.2021;[Epub] CrossRef - The most reliable time point for intact parathyroid hormone measurement to predict hypoparathyroidism after total thyroidectomy with central neck dissection to treat papillary thyroid carcinoma: a prospective cohort study
Jae Won Chang, Ki Wan Park, Seung-Nam Jung, Lihua Liu, Sung Min Kim, Bon Seok Koo
European Archives of Oto-Rhino-Laryngology.2020; 277(2): 549. CrossRef - Time Trends for Prostate Cancer Incidence from 2003 to 2013 in South Korea: An Age-Period-Cohort Analysis
Hyun Young Lee, Do Kyoung Kim, Seung Whan Doo, Won Jae Yang, Yun Seob Song, Bora Lee, Jae Heon Kim
Cancer Research and Treatment.2020; 52(1): 301. CrossRef - Clinical behavior and outcome of papillary T1 thyroid cancers: South Korea vs. Turkey vs. Colombia in a cohort study analyzing oncological outcomes
Murat Ozdemir, Yong-Sang Lee, Ozer Makay, Juan Pablo Dueñas, Bulent Yazici, Aysegul Akgun, Gokhan Icoz, Mahir Akyildiz, Soo Young Kim, Seok-Mo Kim, Hojin Chang, Hang-Seok Chang, Cheong Soo Park
Asian Journal of Surgery.2020; 43(8): 795. CrossRef - Radioiodine ablation in thyroid cancer patients: renal function and external radiation dose rate at discharge according to patient preparation
Yeon-Hee Han, Hwan-Jeong Jeong, Myung-Hee Sohn, Sun Y. Lee, Seok T. Lim
The Quarterly Journal of Nuclear Medicine and Molecular Imaging.2020;[Epub] CrossRef - Effect of the location and size of thyroid nodules on the diagnostic performance of ultrasound elastography: A retrospective analysis
Xinxin Xie, Yongqiang Yu
Clinics.2020; 75: e1720. CrossRef Fine-Needle Aspiration of Subcentimeter Thyroid Nodules in the Real-World Management
Chaiho Jeong, Hyunsam Kim, Jeongmin Lee, Jeonghoon Ha, Min-Hee Kim, Moo Il Kang, Dong-Jun Lim
Cancer Management and Research.2020; Volume 12: 7611. CrossRef- Continuing controversy regarding individualized surgical decision-making for patients with 1–4 cm low-risk differentiated thyroid carcinoma: A systematic review
Wen Liu, Xuejing Yan, Ruochuan Cheng
European Journal of Surgical Oncology.2020; 46(12): 2174. CrossRef - Clinical Implication of World Health Organization Classification in Patients with Follicular Thyroid Carcinoma in South Korea: A Multicenter Cohort Study
Meihua Jin, Eun Sook Kim, Bo Hyun Kim, Hee Kyung Kim, Hyon-Seung Yi, Min Ji Jeon, Tae Yong Kim, Ho-Cheol Kang, Won Bae Kim, Young Kee Shong, Mijin Kim, Won Gu Kim
Endocrinology and Metabolism.2020; 35(3): 618. CrossRef - Clinical Outcomes of N1b Papillary Thyroid Cancer Patients Treated with Two Different Doses of Radioiodine Ablation Therapy
Meihua Jin, Jonghwa Ahn, Yu-Mi Lee, Tae-Yon Sung, Won Gu Kim, Tae Yong Kim, Jin-Sook Ryu, Won Bae Kim, Young Kee Shong, Min Ji Jeon
Endocrinology and Metabolism.2020; 35(3): 602. CrossRef - A Propensity Score‐matched Comparison Study of Surgical Outcomes in Patients with Differentiated Thyroid Cancer After Robotic Versus Open Total Thyroidectomy
Dong Sik Bae, Do Hoon Koo
World Journal of Surgery.2019; 43(2): 540. CrossRef - Diagnostic value of cytology, thyroglobulin, and combination of them in fine-needle aspiration of metastatic lymph nodes in patients with differentiated thyroid cancer
Yixin Xu, Dapeng Wu, Wenting Wu, Jian Jiang, Cheng Xi, Nianyuan Ye, Yibo Wang, Xuezhong Xu
Medicine.2019; 98(45): e17859. CrossRef - Investigation of blood groups in benign thyroid diseases in Turkey
Murat Dağdeviren, İhsan Ateş, Burak Furkan Demir, Emine Ergün, Canan Yıldız, Mustafa Altay
Endocrine Journal.2019; 66(11): 1001. CrossRef - Tumor Volume Doubling Time in Active Surveillance of Papillary Thyroid Carcinoma
Hye-Seon Oh, Hyemi Kwon, Eyun Song, Min Ji Jeon, Tae Yong Kim, Jeong Hyun Lee, Won Bae Kim, Young Kee Shong, Ki-Wook Chung, Jung Hwan Baek, Won Gu Kim
Thyroid.2019; 29(5): 642. CrossRef - Tumor doubling time predicts response to sorafenib in radioactive iodine-refractory differentiated thyroid cancer
Min Joo Kim, Seok-Mo Kim, Eun Kyung Lee, Yul Hwangbo, You Jin Lee, Sun Wook Cho, Do Joon Park, Yumi Lee, Young Joo Park
Endocrine Journal.2019; 66(7): 597. CrossRef - Total thyroidectomy's association with survival in papillary thyroid cancers and the high proportion of total thyroidectomy in low-risk patients: Analysis of Korean nationwide data
Hyun-Soo Zhang, Eun-Kyung Lee, Yuh-Seog Jung, Byung-Ho Nam, Kyu-Won Jung, Hyun-Joo Kong, Young-Joo Won, Boyoung Park
Surgery.2019; 165(3): 629. CrossRef - Individualized Follow-Up Strategy for Patients with an Indeterminate Response to Initial Therapy for Papillary Thyroid Carcinoma
Hye-Seon Oh, Jong Hwa Ahn, Eyun Song, Ji Min Han, Won Gu Kim, Tae Yong Kim, Won Bae Kim, Young Kee Shong, Min Ji Jeon
Thyroid.2019; 29(2): 209. CrossRef - Differentiated Thyroid Cancer and Radioactive Iodine: Past, Present and Future
Jaetae Lee, Il Jo
International Journal of Thyroidology.2019; 12(2): 71. CrossRef - Diagnostic performance of HMGA2 gene expression for differentiation of malignant thyroid nodules: A systematic review and meta‐analysis
Bo Hyun Kim, Seong Jang Kim, Mijin Kim, Sang‐Woo Lee, Shin Young Jeong, Kyoungjune Pak, Keunyoung Kim, In Joo Kim
Clinical Endocrinology.2018; 89(6): 856. CrossRef - Ultrasound risk evaluation of thyroid nodules that are “unspecified” in the 2015 American Thyroid Association management guidelines
Luying Gao, Xuehua Xi, Juanjuan Wang, Xiao Yang, Ying Wang, Shenling Zhu, Xingjian Lai, Xiaoyan Zhang, Ruina Zhao, Bo Zhang
Medicine.2018; 97(52): e13914. CrossRef - Refining the eighth edition AJCC TNM classification and prognostic groups for papillary thyroid cancer with lateral nodal metastasis
Hye In Kim, Kyunga Kim, So Young Park, Jun-Ho Choe, Jung-Han Kim, Jee Soo Kim, Young Lyun Oh, Soo Yeon Hahn, Jung Hee Shin, Hyeon Seon Ahn, Sun Wook Kim, Tae Hyuk Kim, Jae Hoon Chung
Oral Oncology.2018; 78: 80. CrossRef - Thyroid cancer surgery guidelines in an era of de-escalation
K.J. Kovatch, C.W. Hoban, A.G. Shuman
European Journal of Surgical Oncology.2018; 44(3): 297. CrossRef - Changes in Serum Thyroglobulin Levels After Lobectomy in Patients with Low-Risk Papillary Thyroid Cancer
Suyeon Park, Min Ji Jeon, Hye-Seon Oh, Yu-Mi Lee, Tae-Yon Sung, Minkyu Han, Ji Min Han, Tae Yong Kim, Ki-Wook Chung, Won Bae Kim, Young Kee Shong, Won Gu Kim
Thyroid.2018; 28(8): 997. CrossRef - Study Protocol of Multicenter Prospective Cohort Study of Active Surveillance on Papillary Thyroid Microcarcinoma (MAeSTro)
Jae Hoon Moon, Ji-hoon Kim, Eun Kyung Lee, Kyu Eun Lee, Sung Hye Kong, Yeo Koon Kim, Woo-jin Jung, Chang Yoon Lee, Roh-Eul Yoo, Yul Hwangbo, Young Shin Song, Min Joo Kim, Sun Wook Cho, Su-jin Kim, Eun Jae Jung, June Young Choi, Chang Hwan Ryu, You Jin Lee
Endocrinology and Metabolism.2018; 33(2): 278. CrossRef - Low-Dose Radioactive Iodine Ablation Is Sufficient in Patients With Small Papillary Thyroid Cancer Having Minor Extrathyroidal Extension and Central Lymph Node Metastasis (T3 N1a): Reply
Minjung Seo, Yon Seon Kim, Jong Cheol Lee, Myung Woul Han, Eun Sook Kim, Kyung Bin Kim, Seol Hoon Park
Clinical Nuclear Medicine.2018; 43(8): 635. CrossRef - Diagnosis and treatment of low-risk papillary thyroid microcarcinoma
Jae Hoon Moon, Young Joo Park
Journal of the Korean Medical Association.2018; 61(4): 232. CrossRef - Efficacy of a Home-Based Exercise Program After Thyroidectomy for Thyroid Cancer Patients
Kyunghee Kim, Mee Ock Gu, Jung Hwa Jung, Jong Ryeal Hahm, Soo Kyoung Kim, Jin Hyun Kim, Seung Hoon Woo
Thyroid.2018; 28(2): 236. CrossRef - Genome-Wide Association Study Reveals Distinct Genetic Susceptibility of Thyroid Nodules From Thyroid Cancer
Yul Hwangbo, Eun Kyung Lee, Ho-Young Son, Sun-Wha Im, Soo-Jung Kwak, Ji Won Yoon, Min Joo Kim, Jeongseon Kim, Hoon Sung Choi, Chang Hwan Ryu, You Jin Lee, Jong-Il Kim, Nam H Cho, Young Joo Park
The Journal of Clinical Endocrinology & Metabolism.2018; 103(12): 4384. CrossRef - Active Surveillance of Low-Risk Papillary Thyroid Microcarcinoma: A Multi-Center Cohort Study in Korea
Hye-Seon Oh, Jeonghoon Ha, Hye In Kim, Tae Hyuk Kim, Won Gu Kim, Dong-Jun Lim, Tae Yong Kim, Sun Wook Kim, Won Bae Kim, Young Kee Shong, Jae Hoon Chung, Jung Hwan Baek
Thyroid.2018; 28(12): 1587. CrossRef - Ultrasound criteria for risk stratification of thyroid nodules in the previously iodine deficient area of Austria - a single centre, retrospective analysis
Christina Tugendsam, Veronika Petz, Wolfgang Buchinger, Brigitta Schmoll-Hauer, Iris Pia Schenk, Karin Rudolph, Michael Krebs, Georg Zettinig
Thyroid Research.2018;[Epub] CrossRef - Practical Initial Risk Stratification Based on Lymph Node Metastases in Pediatric and Adolescent Differentiated Thyroid Cancer
Min Ji Jeon, Young Nam Kim, Tae-Yong Sung, Suck Joon Hong, Yoon Young Cho, Tae Yong Kim, Young Kee Shong, Won Bae Kim, Sun Wook Kim, Jae Hoon Chung, Tae Hyuk Kim, Won Gu Kim
Thyroid.2018; 28(2): 193. CrossRef - Current Radiological Approach in Thyroid Nodules
Duzgun Yildirim, Deniz Alis, Sabri Sirolu, Cesur Samanci, Fethi Emre Ustabasioglu, Bulent Colakoglu
Journal of Cancer Therapy.2017; 08(05): 423. CrossRef - A new paradigm in low-risk papillary microcarcinoma: active surveillance
Alex González Bóssolo, Michelle Mangual Garcia, Paula Jeffs González, Miosotis Garcia, Guillermo Villarmarzo, Jose Hernán Martinez
Endocrinology, Diabetes & Metabolism Case Reports.2017;[Epub] CrossRef - Serial Neck Ultrasonographic Evaluation of Changes in Papillary Thyroid Carcinoma During Pregnancy
Hye-Seon Oh, Won Gu Kim, Suyeon Park, Mijin Kim, Hyemi Kwon, Min Ji Jeon, Jeong Hyun Lee, Jung Hwan Baek, Dong Eun Song, Tae Yong Kim, Young Kee Shong, Won Bae Kim
Thyroid.2017; 27(6): 773. CrossRef - Restratification of survival prognosis of N1b papillary thyroid cancer by lateral lymph node ratio and largest lymph node size
Hye In Kim, Tae Hyuk Kim, Jun‐Ho Choe, Jung‐Han Kim, Jee Soo Kim, Young Lyun Oh, Soo Yeon Hahn, Jung Hee Shin, Hye Won Jang, Young Nam Kim, Hosu Kim, Hyeon Seon Ahn, Kyunga Kim, Sun Wook Kim, Jae Hoon Chung
Cancer Medicine.2017; 6(10): 2244. CrossRef - Comparison on Fine Needle Aspiration Cytology (FNAC) and Thyroid Ultrasonography in Management of Thyroid Nodules
Sandini A Gunaratne
International Clinical Pathology Journal.2017;[Epub] CrossRef - Current Practices of Thyroid Fine-Needle Aspiration in Asia: A Missing Voice
Andrey Bychkov, Kennichi Kakudo, SoonWon Hong
Journal of Pathology and Translational Medicine.2017; 51(6): 517. CrossRef - Clinical outcomes after delayed thyroid surgery in patients with papillary thyroid microcarcinoma
Min Ji Jeon, Won Gu Kim, Hyemi Kwon, Mijin Kim, Suyeon Park, Hye-Seon Oh, Minkyu Han, Tae-Yon Sung, Ki-Wook Chung, Suck Joon Hong, Tae Yong Kim, Young Kee Shong, Won Bae Kim
European Journal of Endocrinology.2017; 177(1): 25. CrossRef - Articles inEndocrinology and Metabolismin 2016
Won-Young Lee
Endocrinology and Metabolism.2017; 32(1): 62. CrossRef - The Impact of Thyroid Nodule Size and Fine-Needle Aspiration Biopsy Result on the Risk of Malignancy in the Patients Who Underwent Thyroidectomy
Hwibin Im, Yu-Young Park, Jae-Gu Cho, Seung-Kuk Baek, Soon-Young Kwon, Kwang-Yoon Jung, Jeong-Soo Woo
Korean Journal of Otorhinolaryngology-Head and Neck Surgery.2017; 60(6): 308. CrossRef - Active Surveillance of Papillary Thyroid Microcarcinoma: A Mini-Review from Korea
Tae Yong Kim, Young Kee Shong
Endocrinology and Metabolism.2017; 32(4): 399. CrossRef

 KES
KES
 PubReader
PubReader Cite
Cite