Articles
- Page Path
- HOME > Endocrinol Metab > Volume 36(6); 2021 > Article
-
Image of InterestAdrenal Gland Mucosal Neuroma Cues for Endocrine Emergency Treatment
-
Gyu Gang Choi1
 , Hwan Jin Lee1, Hyo Jin Han1, Young Beom Jeong2, Heung Bum Lee1, Ji Hyun Park1
, Hwan Jin Lee1, Hyo Jin Han1, Young Beom Jeong2, Heung Bum Lee1, Ji Hyun Park1
-
Endocrinology and Metabolism 2021;36(6):1312-1313.
DOI: https://doi.org/10.3803/EnM.2021.1269
Published online: December 3, 2021
1Department of Internal Medicine, Jeonbuk National University Medical School, Jeonju, Korea
2Department of Urology, Jeonbuk National University Medical School, Jeonju, Korea
- Corresponding author: Ji Hyun Park. Division of Endocrinology and Metabolism, Department of Internal Medicine, Jeonbuk National University Medical School, Research Institute of Clinical Medicine of Jeonbuk National University-Biomedical Research Institute of Jeonbuk National University Hospital, 20 Geonji-ro, Deokjin-gu, Jeonju 54907, Korea, Tel: +82-63-250-1780, Fax: +82-63-254-1609, E-mail: parkjh@jbnu.ac.kr
• Received: September 17, 2021 • Revised: October 25, 2021 • Accepted: November 4, 2021
Copyright © 2021 Korean Endocrine Society
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 2,534 Views
- 91 Download
-
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
Article information
Fig. 1(A) Mucosal neuromas on the tongue are found during the initial physical examination at the time of hospital admission, although a dehydrated, cracked, and dry tongue obscures this finding. A histopathological examination was not performed for these neuromas because they were benign tumors and had no specific symptoms. (B) A photograph, taken 6 days after the ectopic adrenocorticotropic hormone syndrome was resolved by bilateral adrenalectomy, shows clearly visible lingual mucosal neuromas with thickened lips, which are typical features of multiple endocrine neoplasia type 2B (MEN2B).


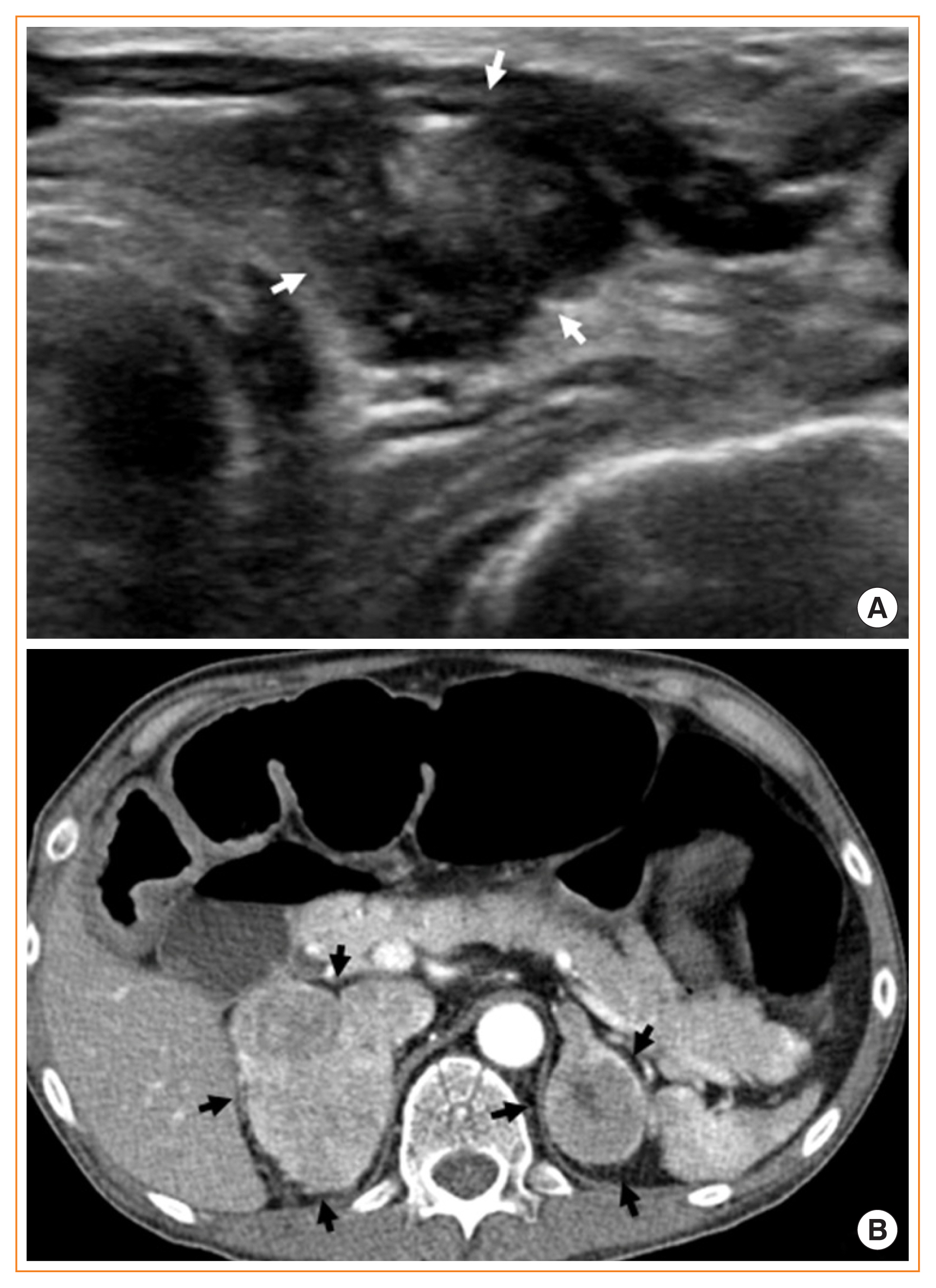
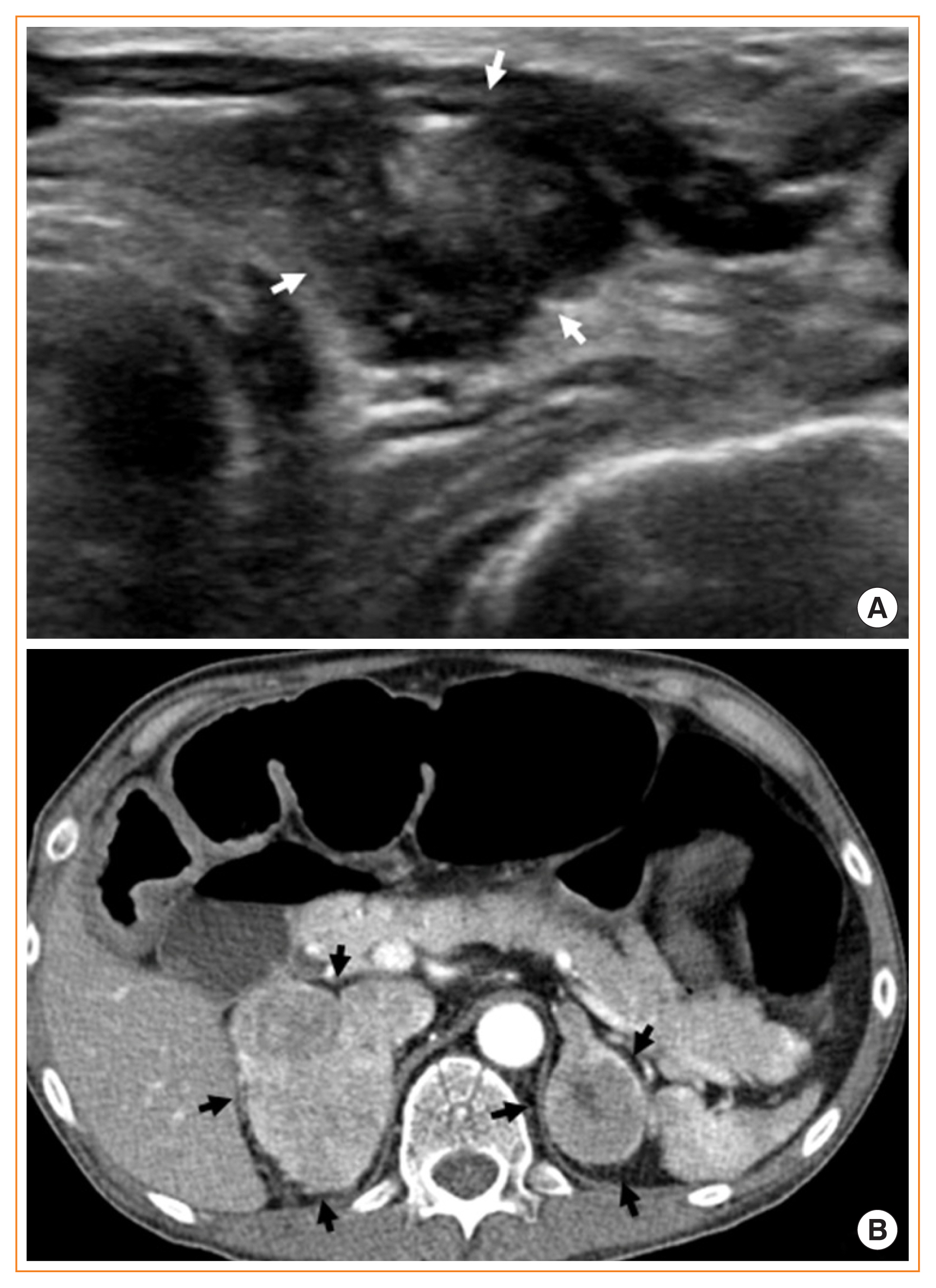
Fig. 2(A) Transverse neck sonographic image showing a 1.8 cm, irregular-shaped, hypoechoic nodule (white arrows) with speculated margins, heterogeneous echotexture of the solid portion, and microcalcifications located in the left lobe of the thyroid. (B) Axial contrast-enhanced computed tomography image showing heterogeneous enhancing masses in both adrenal glands (black arrows), including focal cystic components in the left adrenal mass, with diffuse dilatation of the transverse colon.
- 1. Elliott PF, Berhane T, Ragnarsson O, Falhammar H. Ectopic ACTH- and/or CRH-producing pheochromocytomas. J Clin Endocrinol Metab 2021;106:598–608.ArticlePubMed
- 2. Choi HS, Kim MJ, Moon CH, Yoon JH, Ku HR, Kang GW, et al. Medullary thyroid carcinoma with ectopic adrenocorticotropic hormone syndrome. Endocrinol Metab (Seoul) 2014;29:96–100.ArticlePubMedPMC
- 3. Young J, Haissaguerre M, Viera-Pinto O, Chabre O, Baudin E, Tabarin A. Management of endocrine disease: Cushing’s syndrome due to ectopic ACTH secretion: an expert operational opinion. Eur J Endocrinol 2020;182:R29–58.ArticlePubMed
References
Figure & Data
References
Citations
Citations to this article as recorded by 


 KES
KES
 PubReader
PubReader ePub Link
ePub Link Cite
Cite



