Articles
- Page Path
- HOME > Endocrinol Metab > Volume 28(3); 2013 > Article
-
Original ArticleVariation in Serum Creatinine Level Is Correlated to Risk of Type 2 Diabetes
- Jun Sung Moon1, Ji Eun Lee2, Ji Sung Yoon1
-
Endocrinology and Metabolism 2013;28(3):207-213.
DOI: https://doi.org/10.3803/EnM.2013.28.3.207
Published online: September 13, 2013
1Department of Internal Medicine, Yeungnam University College of Medicine, Daegu, Korea.
2Department of Internal Medicine, CHA Gumi Medical Center, CHA University, Gumi, Korea.
- Corresponding author: Ji Sung Yoon. Department of Internal Medicine, Yeungnam University College of Medicine, 170 Hyeonchung-ro, Nam-gu, Daegu 705-717, Korea. Tel: +82-53-620-4049, Fax: +82-53-623-8006, jsyoon9@ynu.ac.kr
- Corresponding author: Ji Eun Lee. Department of Internal Medicine, CHA Gumi Medical Center, CHA University, 12 Sinsi-ro 10-gil, Gumi 730-728, Korea. Tel: +82-54-450-9700, Fax: +82-54-452-5089, chieun@naver.com
Copyright © 2013 Korean Endocrine Society
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 4,088 Views
- 46 Download
- 19 Crossref
ABSTRACT
-
Background
- Skeletal muscle is well established as a major target organ of insulin action, and is associated with the pathogenesis of type 2 diabetes. Therefore, we attempted to determine whether a variation in serum creatinine is related to the development of type 2 diabetes and other risk factors for diabetes.
-
Methods
- A total of 2,676 nondiabetic subjects with stable and normal renal function (estimated glomerular filtration rate >60 mL/min/1.73 m2) were followed up for approximately 4.5 years. New onset diabetes was defined as fasting plasma glucose (FPG) ≥7.0 mmol/L, glycated hemoglobin (HbA1c) ≥6.5%, or subjects taking antidiabetic agents. Variation of serum creatinine (ΔCre) was defined as a difference between follow-up and baseline creatinine. In subgroup analysis, body composition was examined by bioelectric impedance analysis method.
-
Results
- A total of 106 subjects were diagnosed with new-onset diabetes during the follow-up period. Baseline serum creatinine was not different between the new-onset diabetes and no diabetes groups. Negative ΔCre (ΔCre <0) showed an association with increased risk of type 2 diabetes after adjusting for age, sex, body mass index, systolic blood pressure, FPG, HbA1c, triglyceride, high density lipoprotein cholesterol, and γ-glutamyl transpeptidase (odds ratio, 1.885; 95% confidence interval, 1.127 to 3.153). Serum creatinine level demonstrated positive correlation with muscle mass and negative correlation with percentage of body fat in body composition analysis.
-
Conclusion
- Serum creatinine reflected body muscle mass and the decrease of serum creatinine might be regarded as a risk factor for type 2 diabetes.
- Skeletal muscle is one of the major target organs of insulin action and the primary site for insulin-mediated glucose uptake in the postprandial state [1-4]. In addition, reduced muscle mass could potentially induce hyperglycemia and insulin resistance [5]. Therefore, skeletal muscle could be an original target for the treatment of metabolic disorders, e.g., insulin resistance, glucose intolerance, and type 2 diabetes mellitus [3]. In elderly patients with diabetes, dietary amino acid supplements could antagonize muscle catabolism and glucose derangement, and have been shown to increase insulin sensitivity and decrease glycated hemoglobin (HbA1c) levels [5]. Serum creatinine is a breakdown product of creatine phosphate in muscle. Since the amount of creatinine per unit of skeletal muscle mass is consistent and the breakdown rate of creatine is also consistent, plasma creatinine concentration is very stable and is a direct reflection of skeletal muscle mass [4,6]. In the Kansai Healthcare Study, lower serum creatinine levels demonstrated an association with an increased risk of type 2 diabetes [4]. A lower volume of skeletal muscle could mean fewer target sites for insulin action and this, in part, may explain the pathogenesis of type 2 diabetes associated with lower serum creatinine [4]. Accordingly, we attempted to determine whether serum creatinine and its variation are related to development of type 2 diabetes, along with other risk factors for diabetes.
INTRODUCTION
- This study was conducted retrospectively. Subjects included 2,676 nondiabetic patients aged 18 to 75 years who visited the health care center of Yeungnam University Medical Center between 2001 January 1 and 2003 December 31. These subjects were visited again from 2005 January 1 to 2008 December 31. The presence of diabetes was determined by fasting plasma glucose (FPG) ≥7.0 mmol/L (n=61), HbA1c ≥6.5% (n=15), history of diabetes, or taking antidiabetic agents, which was ascertained via questionnaire; subjects with diabetes at baseline were excluded (n=20) [7]. We attempted to evaluate the serum creatinine as a surrogate marker of muscle mass under normal and stable renal function. Estimated glomerular filtration rate (eGFR) was calculated from creatinine using the Modification of Diet in Renal Disease (MDRD) equation, as follows: eGFR=186.3×[serum creatinine (mg/dL)]-1.154×[age (years)]-0.203×(0.742 if female) [8]. We included chronic kidney disease stage 1 and 2 (eGFR ≥60 mL/min/1.73 m2), and excluded subjects with higher serum creatinine (≥132.6 µmol/L, n=5) or eGFR <60 mL/min/1.73 m2 (n=49) at baseline. Blood samples were collected after an overnight fast (at least 8 hours) at baseline and at the end of the follow-up. Serum creatinine and other routine laboratory blood tests were performed with an automatic Olymphus AU5400 Analyzer (Olympus Optical, Tokyo, Japan). Serum creatinine was calibrated using the Jaffe method installed on the Olymphus AU5400 Analyzer. A variation of serum creatinine (ΔCre) was defined as a difference between follow-up and baseline creatinine. FPG was measured using the hexokinase method. HbA1c was measured using high performance liquid chromatography (HLC-723G7, Tosoh, Tokyo, Japan). Serum total cholesterol was measured using an enzymatic colorimetric method (Kyowa Medex Co., Ltd., Tokyo, Japan). Serum high density lipoprotein cholesterol (HDL-C) and low density lipoprotein cholesterol was measured using a direct enzymatic assay (Kyowa Medex Co., Ltd.). Body mass index (BMI) was computed from measurements of height and weight, as follows: BMI=body weight (kg)/height (m2). In some subjects, we analyzed body composition using the Inbody 720 (Biospace, Seoul, Korea), a multifrequency impedance body composition analyzer. The Inbody 720 uses an 8-point tactile electrode method, measuring resistance at five specific frequencies (1, 50, 250, 500 kHz, and 1 MHz) and reactance at three specific frequencies (5, 50, and 250 kHz).
- Differences of continuous variables between subjects who were diagnosed with new-onset diabetes and the no diabetes group were analyzed using Student t test for statistical analysis. We used linear regression analysis to evaluate correlation between serum creatinine, muscle mass, and percentage of body fat tissue. We used multiple logistic regression analysis and computed odds ratios (ORs) for the incidence of type 2 diabetes in order to determine the relationship between the incidence of type 2 diabetes and variation of serum creatinine. Results were expressed as a mean±SD for continuous variables. Statistical analyses were performed using SPSS version 18.0 for Windows (IBM Co., Armonk, NY, USA). All statistical tests were two tailed and a P value of less than 0.05 was regarded as statistically significant. All patients provided informed consent, and the study protocol was approved by our local ethics committee, as well as the Institutional Review Board of Yeungnam University Medical Center.
METHODS
- A total of 2,602 nondiabetic subjects were finally included in this study and the mean follow-up duration was 4.5±0.67 years. During the follow-up period, 106 subjects were diagnosed with diabetes and were categorized into the new-onset diabetes group. A summary of the baseline characteristics of the subjects is shown in Tables 1, 2. Compared with the no diabetes group, subjects in the new-onset diabetes group were older, with higher BMI, higher systolic blood pressure (SBP)/diastolic blood pressures (DBP), higher FPG, and higher HbA1c levels (P<0.05). The baseline serum creatinine level did not differ between the two groups, however, ΔCre was lower in the new-onset diabetes group compared with the no diabetes group (P<0.05). Table 2 shows the differences in characteristics of subjects in the negative ΔCre group (ΔCre <0) and positive ΔCre group (ΔCre ≥0). Subjects in the negative ΔCre group (n=755) had higher BMI and SBP. No difference in the baseline fasting blood glucose and HbA1c was observed between the two groups. However, more patients in the negative ΔCre group developed type 2 diabetes (P<0.05).
- In multivariate regression analysis (Table 3), higher SBP, FPG, HbA1c, and lower HDL-C showed an association with development of type 2 diabetes (P<0.05). After adjusting for age, gender, BMI, SBP and DBP, FPG, HbA1c, triglyceride, HDL-C, and γ-GTP, the decrease of serum creatinine showed an independent association with development of type 2 diabetes with an OR of 1.885 (95% confidence interval [CI], 1.127 to 3.153; P=0.015). In male subjects (n=1,551), the OR of negative ΔCre was 2.249 (95% CI, 1.184 to 4.274; P=0.013).
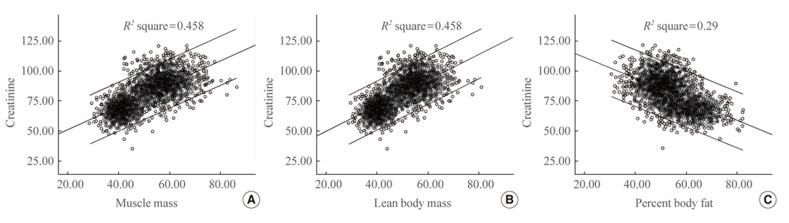
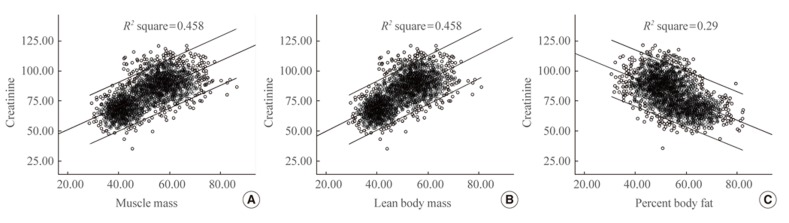
- In subgroup analysis using bioelectric impedance analysis (BIA) method, we obtained the lean body mass of 1,067 subjects at baseline and 27 cases were identified as newly diagnosed diabetes. Serum creatinine showed positive correlation with body muscle mass and lean body mass, and negative correlation with body fat percentage in linear regression analysis (Fig. 1). Although basal lean body mass was not associated with the risk for incident diabetes, the change of lean body mass was negatively correlated with incident diabetes (P<0.05). The change of lean body mass was also positively correlated with the change of serum creatinine (P<0.05). Serum creatinine was negatively correlated with body fat mass and percent body fat (P<0.05). ΔCre and the change of body fat mass showed marginal correlation, but had no statistical significance (P=0.05).
RESULTS
- In this retrospective follow-up study, we found that the variation of serum creatinine is closely associated with age-related sarcopenic changes. Additionally negative ΔCre, that is decreased creatinine, is independent risk factor of diabetes in healthy subjects with normal renal function.
- Reduced muscle mass, or sarcopenia, has been reported as a well-known risk factor for insulin resistance and type 2 diabetes [9-12]. Since skeletal muscle is the primary tissue contributing to whole body insulin-mediated glucose disposal, sarcopenia may be an important causal factor in age-induced insulin resistance and type 2 diabetes susceptibility [9]. In the study reported by Srikanthan and Karlamangla [13], muscle mass relative to body size might also predict the level of insulin resistance and risk of prediabetes. They also revealed that sarcopenia might be an early predictor of diabetes susceptibility independent of obesity in a large population study [9]. Kim et al. [14] reported that sarcopenic obesity was associated with the risk of metabolic syndrome in a cohort study of Korean subjects. Similarly, Lim et al. [15] showed that sarcopenic obesity was more closely correlated with metabolic syndrome than either sarcopenia or obesity alone. Therefore, serial examinations about sarcopenic and obese changes, through analyzing proportions of skeletal muscles and body fat, are presumed to predict diabetes. However, there are some limitations for carrying those predictions into clinical practice. What the gold standard is still debatable among various instruments to measure muscle mass, strength, and function. Although dual energy X-ray absorptiometry (DEXA) or computed tomography were currently accepted to be gold standard tests for evaluating body composition [16], these methods are not easily accessible and not commonly available to large epidemiologic studies due to time and cost. Additionally, there is not a consensus about concepts of sarcopenia and sarcopenic obesity, and it is unclear which definition is most powerful to predict prognosis [17]. Recently the European Working Group on Sarcopenia in Older People suggested a practical definition using the concepts of muscle mass and function [18], but that also has limitations. This criteria is not accepted widely, and inappropriate to apply other ethnicities, including Asians.
- We hypothesized that variation of serum creatinine might be related to change of insulin sensitivity, and predict the risk of type 2 diabetes. Serum creatinine concentration is simple, cheap, and widely used for evaluation of renal function, and is known to be a very stable surrogate marker of skeletal muscle mass [4,6,19]. Previous studies have reported correlations of total plasma creatinine with lean body mass, estimated anthropometrically using BIA or DEXA [20-22]. According to Harita et al. [4], lower serum creatinine increased the risk of type 2 diabetes in their large cohort study. In a large cohort study of chronic kidney disease patients receiving hemodialysis, an increase in lean body mass accompanied by a parallel increase in muscle mass was associated with survival benefit [23]. Consistent with these results, we found that serum creatinine was positively associated with muscle mass and had inverse relationship with percentage of body fat in subgroup analysis using BIA. The variation of serum creatinine also may imply the change of lean body mass, as we expected. The incidence of type 2 diabetes was higher in the negative ΔCre group, even though the baseline creatinine level did not differ between the groups. Taken together, subjects with similar creatinine level at baseline may have different risk of diabetes and negative ΔCre is also considered to independent risk factor of diabetes. Serial follow-up of serum creatinine could be alternative for repetitive body composition analysis.
- Oterdoom and his colleagues [24] demonstrated that low muscle mass, as reflected by low creatinine excretion, was associated with major adverse cardiovascular events and all cause mortality in general populations. They reported that their results were independent of insulin sensitivity, components of the metabolic syndrome, and inflammation. However, muscle mass measured by urinary creatinine excretion was positively associated with fasting insulin and components of metabolic syndrome. Also, diabetes was not associated with lower creatinine excretion in both male and female subjects. The authors explained that insulin is an anabolic hormone, so subjects with higher muscle masses may have higher insulin concentrations. When comparing our results, the discrepancies might be come from differing methods to assess muscle mass (urinary creatinine excretion vs. serum creatinine level), but further studies are needed to clarify the differences in results.
- Female gender tended to have lower skeletal muscle mass than male. Intuitionally, gender differences might be considered when using serum creatinine as a surrogate marker of muscle mass. A large cohort study of Japanese men [4] reported that low serum creatinine increased the risk of type 2 diabetes, but the investigators did not include females. They suggested the results may differ in women because of their lower levels of skeletal muscle mass. Serum creatinine, as a risk factor of diabetes, was more closely associated in male than females in our study. These findings suggest that variation of creatinine can differ depending on gender, and gender differences should be considered and weighed practically.
- Our study had several limitations. Firstly, given that serum creatinine closely related with skeletal muscle mass, it could be influenced by numerous factors such as drugs and other dietary factors. We tried to eliminate confounding factors through questionnaires at baseline, but could not exclude exogenous factors during follow-up periods. Secondly, this was a retrospective observational study and the numbers of participants were relatively small for single center recruitment. Thirdly, some cases of undetermined diabetes might have existed since postprandial plasma glucose levels and 75 g oral glucose tolerance tests were not checked. Additionally, the variation of creatinine could be surrogate of insulin resistance but not reflect insulin secretory function, so β-cell failure-another main cause of diabetes-was overlooked. We did not check C-peptide or islet cell autoantibodies, so it is difficult to predict occurrence of diabetes by progressive β-cell failure, such as late adult onset of diabetes. Finally, direct comparisons between insulin resistance indexes (i.e., homeostasis model assessment-estimated insulin resistance, quantitative insulin sensitivity check index, etc.) and creatinine level were not conducted in our subjects.
- In summary, the results of this study showed that serum creatinine could be used as a surrogate marker of skeletal muscle mass, and the decrease of serum creatinine over time might be regarded as a risk factor for type 2 diabetes. Therefore, monitoring of serum creatinine can be helpful in prediction and assessment of type 2 diabetes risk. In order to determine and confirm these results, large-scale prospective randomized controlled trials will be needed in the future.
DISCUSSION
- 1. DeFronzo RA, Jacot E, Jequier E, Maeder E, Wahren J, Felber JP. The effect of insulin on the disposal of intravenous glucose: results from indirect calorimetry and hepatic and femoral venous catheterization. Diabetes 1981;30:1000–1007. ArticlePubMed
- 2. DeFronzo RA, Gunnarsson R, Bjorkman O, Olsson M, Wahren J. Effects of insulin on peripheral and splanchnic glucose metabolism in noninsulin-dependent (type II) diabetes mellitus. J Clin Invest 1985;76:149–155. ArticlePubMedPMC
- 3. DeFronzo RA. Lilly lecture 1987. The triumvirate: beta-cell, muscle, liver: a collusion responsible for NIDDM. Diabetes 1988;37:667–687. ArticlePubMed
- 4. Harita N, Hayashi T, Sato KK, Nakamura Y, Yoneda T, Endo G, Kambe H. Lower serum creatinine is a new risk factor of type 2 diabetes: the Kansai healthcare study. Diabetes Care 2009;32:424–426. ArticlePubMedPMC
- 5. Solerte SB, Fioravanti M, Locatelli E, Bonacasa R, Zamboni M, Basso C, Mazzoleni A, Mansi V, Geroutis N, Gazzaruso C. Improvement of blood glucose control and insulin sensitivity during a long-term (60 weeks) randomized study with amino acid dietary supplements in elderly subjects with type 2 diabetes mellitus. Am J Cardiol 2008;101(11A):82E–88E.ArticlePubMed
- 6. Kaplan LA, Pesce AJ, Kazmierczak SC. Clinical chemistry: theory, analysis, correlation; 4th ed. St. Louis: Mosby; 2003.
- 7. American Diabetes Association. Standards of medical care in diabetes: 2010. Diabetes Care 2010;33 Suppl 1:S11–S61. ArticlePubMedPDF
- 8. Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation: modification of diet in Renal Disease Study Group. Ann Intern Med 1999;130:461–470. ArticlePubMed
- 9. Srikanthan P, Hevener AL, Karlamangla AS. Sarcopenia exacerbates obesity-associated insulin resistance and dysglycemia: findings from the National Health and Nutrition Examination Survey III. PLoS One 2010;5:e10805ArticlePubMedPMC
- 10. Dominguez LJ, Barbagallo M. The cardiometabolic syndrome and sarcopenic obesity in older persons. J Cardiometab Syndr 2007;2:183–189. ArticlePubMed
- 11. Atlantis E, Martin SA, Haren MT, Taylor AW, Wittert GA. Members of the Florey Adelaide Male Ageing Study. Inverse associations between muscle mass, strength, and the metabolic syndrome. Metabolism 2009;58:1013–1022. ArticlePubMed
- 12. Kim TN, Park MS, Lim KI, Yang SJ, Yoo HJ, Kang HJ, Song W, Seo JA, Kim SG, Kim NH, Baik SH, Choi DS, Choi KM. Skeletal muscle mass to visceral fat area ratio is associated with metabolic syndrome and arterial stiffness: the Korean Sarcopenic Obesity Study (KSOS). Diabetes Res Clin Pract 2011;93:285–291. ArticlePubMed
- 13. Srikanthan P, Karlamangla AS. Relative muscle mass is inversely associated with insulin resistance and prediabetes: findings from the third National Health and Nutrition Examination Survey. J Clin Endocrinol Metab 2011;96:2898–2903. ArticlePubMed
- 14. Kim TN, Yang SJ, Yoo HJ, Lim KI, Kang HJ, Song W, Seo JA, Kim SG, Kim NH, Baik SH, Choi DS, Choi KM. Prevalence of sarcopenia and sarcopenic obesity in Korean adults: the Korean sarcopenic obesity study. Int J Obes (Lond) 2009;33:885–892. ArticlePubMedPDF
- 15. Lim S, Kim JH, Yoon JW, Kang SM, Choi SH, Park YJ, Kim KW, Lim JY, Park KS, Jang HC. Sarcopenic obesity: prevalence and association with metabolic syndrome in the Korean Longitudinal Study on Health and Aging (KLoSHA). Diabetes Care 2010;33:1652–1654. ArticlePubMedPMC
- 16. Haderslev KV, Haderslev PH, Staun M. Accuracy of body composition measurements by dual energy x-ray absorptiometry in underweight patients with chronic intestinal disease and in lean subjects. Dyn Med 2005;4:1ArticlePubMedPMC
- 17. Choi KM. Sarcopenia and sarcopenic obesity. Endocrinol Metab 2013;28:86–89.Article
- 18. Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, Martin FC, Michel JP, Rolland Y, Schneider SM, Topinkova E, Vandewoude M, Zamboni M. European Working Group on Sarcopenia in Older People. Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing 2010;39:412–423. ArticlePubMedPMCPDF
- 19. Patel SS, Molnar MZ, Tayek JA, Ix JH, Noori N, Benner D, Heymsfield S, Kopple JD, Kovesdy CP, Kalantar-Zadeh K. Serum creatinine as a marker of muscle mass in chronic kidney disease: results of a cross-sectional study and review of literature. J Cachexia Sarcopenia Muscle 2013;4:19–29. ArticlePubMed
- 20. Schutte JE, Longhurst JC, Gaffney FA, Bastian BC, Blomqvist CG. Total plasma creatinine: an accurate measure of total striated muscle mass. J Appl Physiol 1981;51:762–766. ArticlePubMed
- 21. Donadio C, Halim AB, Caprio F, Grassi G, Khedr B, Mazzantini M. Single- and multi-frequency bioelectrical impedance analyses to analyse body composition in maintenance haemodialysis patients: comparison with dual-energy X-ray absorptiometry. Physiol Meas 2008;29:S517–S524. ArticlePubMed
- 22. Keshaviah PR, Nolph KD, Moore HL, Prowant B, Emerson PF, Meyer M, Twardowski ZJ, Khanna R, Ponferrada L, Collins A. Lean body mass estimation by creatinine kinetics. J Am Soc Nephrol 1994;4:1475–1485. ArticlePubMed
- 23. Kalantar-Zadeh K, Streja E, Kovesdy CP, Oreopoulos A, Noori N, Jing J, Nissenson AR, Krishnan M, Kopple JD, Mehrotra R, Anker SD. The obesity paradox and mortality associated with surrogates of body size and muscle mass in patients receiving hemodialysis. Mayo Clin Proc 2010;85:991–1001. ArticlePubMedPMC
- 24. Oterdoom LH, Gansevoort RT, Schouten JP, de Jong PE, Gans RO, Bakker SJ. Urinary creatinine excretion, an indirect measure of muscle mass, is an independent predictor of cardiovascular disease and mortality in the general population. Atherosclerosis 2009;207:534–540. ArticlePubMed
References
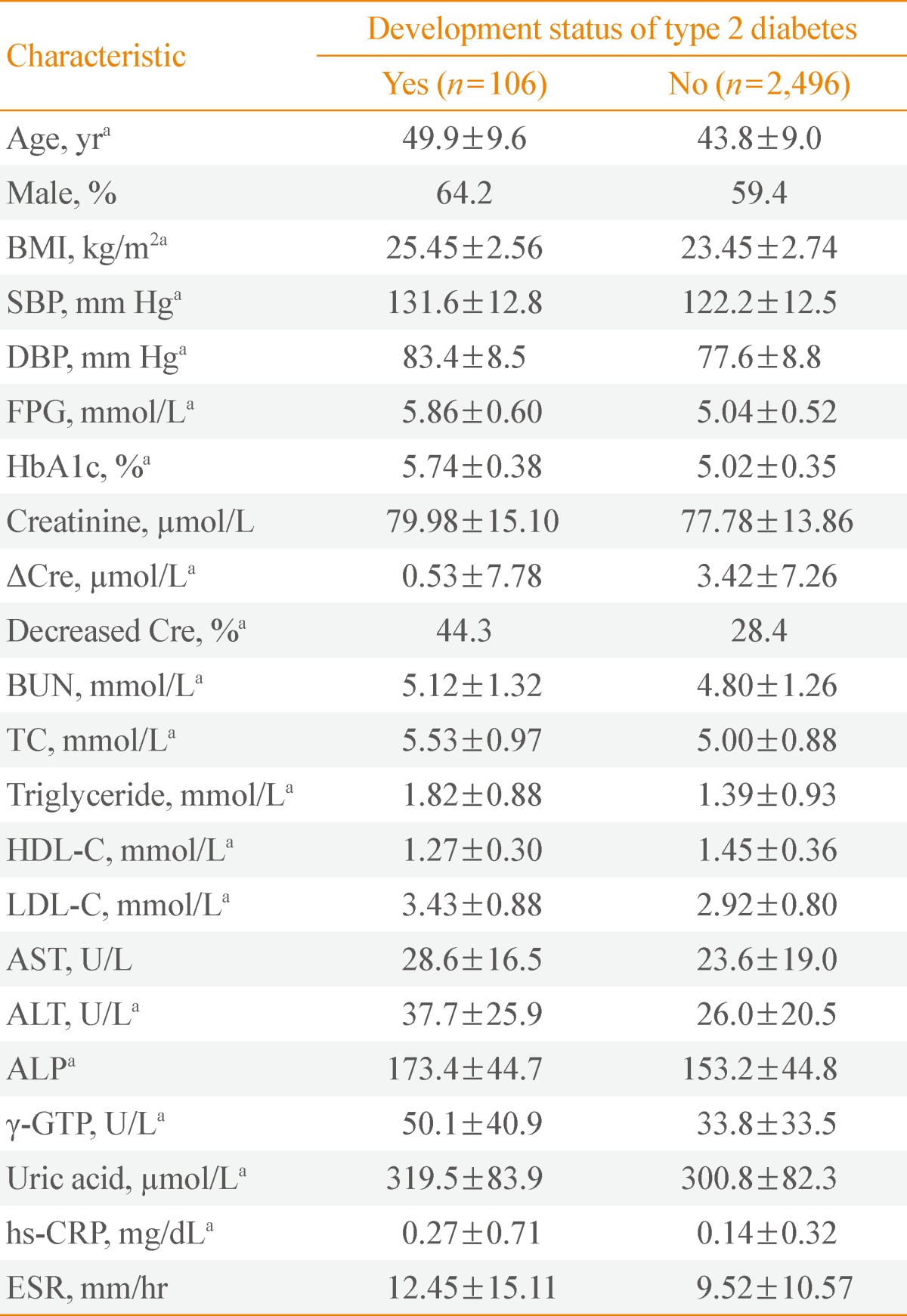
Values are expressed as mean±SD or number (%).
BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; FPG, fasting plasma glucose level; HbA1c, glycated hemoglobin; ΔCre, follow-up serum creatinine level to baseline serum creatinine level; Decreased Cre, follow-up serum creatinine level to baseline serum creatinine level <0; BUN, blood urea nitrogen; TC, total cholesterol; HDL-C, high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol; AST, aspartate aminotransferase; ALT, alanine aminotransferase; ALP, alkaline phosphatase; γ-GTP, γ-glutamyl transpeptidase; hs-CRP, high-sensitivity C-reactive protein; ESR, erythrocyte sedimentation rate.
aP<0.05.
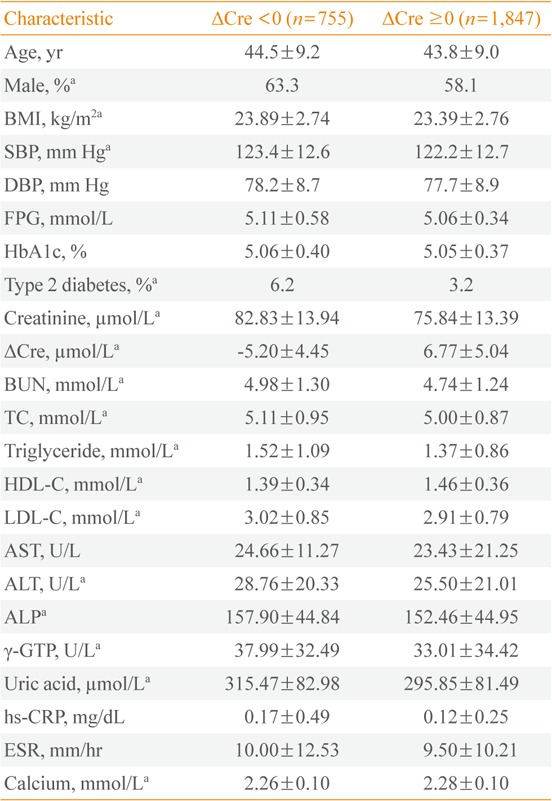
Values are expressed as mean±SD or number (%).
ΔCre, follow-up serum creatinine level to baseline serum creatinine level; BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; FPG, fasting plasma glucose level; HbA1c, glycated hemoglobin; BUN, blood urea nitrogen; TC, total cholesterol; HDL-C, high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol; AST, aspartate aminotransferase; ALT, alanine aminotransferase; ALP, alkaline phosphatase; γ-GTP, γ-glutamyl transpeptidase; hs-CRP, high-sensitivity C-reactive protein; ESR, erythrocyte sedimentation rate.
aP<0.05.
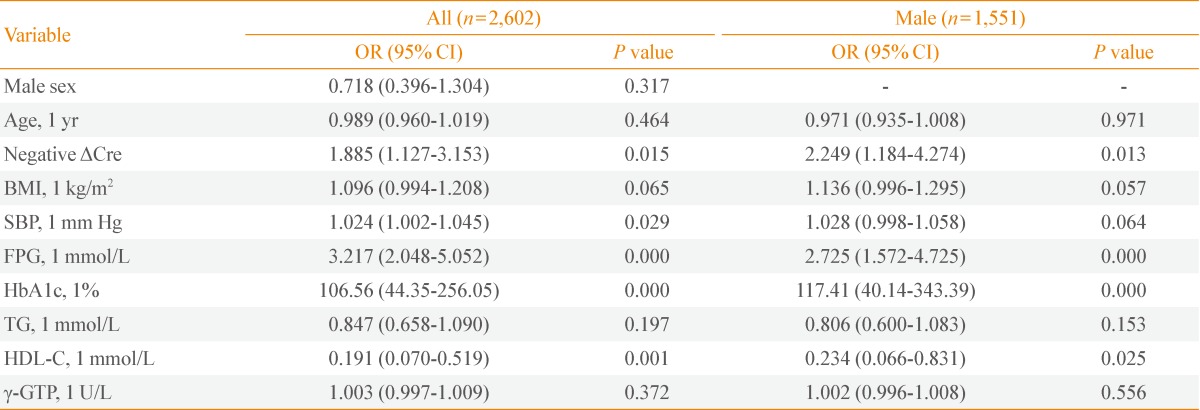
OR and P value analyzed by multivariate regression analysis adjusted for age, sex, BMI, SBP, FPG, HbA1c, TG, HDL-C, and γ-GTP.
OR, odds ratio; CI, confidence interval; ΔCre, follow-up serum creatinine level to baseline serum creatinine level; BMI, body mass index; SBP, systolic blood pressure; FPG, fasting plasma glucose level; HbA1c, glycated hemoglobin; TG, triglyceride; HDL-C, high density lipoprotein cholesterol; γ-GTP, γ-glutamyl transpeptidase.
Figure & Data
References
Citations

- Low serum creatinine, a surrogate marker of muscle mass, correlates with insulin sensitivity in nonhuman primates
Uddhav K. Chaudhari, Barbara C. Hansen
Journal of Medical Primatology.2023; 52(2): 100. CrossRef - Identification of Novel Biomarkers of Spinal Muscular Atrophy and Therapeutic Response by Proteomic and Metabolomic Profiling of Human Biological Fluid Samples
Megi Meneri, Elena Abati, Delia Gagliardi, Irene Faravelli, Valeria Parente, Antonia Ratti, Federico Verde, Nicola Ticozzi, Giacomo P. Comi, Linda Ottoboni, Stefania Corti
Biomedicines.2023; 11(5): 1254. CrossRef - Association of serum creatinine levels and risk of type 2 diabetes mellitus in Korea: a case control study
Do Kyeong Song, Young Sun Hong, Yeon-Ah Sung, Hyejin Lee
BMC Endocrine Disorders.2022;[Epub] CrossRef - Impact of Female Sex on the Susceptibility to Hypernatremia Among Older Community-Dwelling Individuals in Japan
Sho Tanaka, Midori Fujishiro, Kazuhiro Imatake, Yasuyuki Suzuki, Hisamitsu Ishihara, Shigemasa Tani
International Journal of General Medicine.2022; Volume 15: 777. CrossRef - Ameliorative Effect of Oxytocin on FBN1 and PEPCK Gene Expression, and Behavioral Patterns in Rats' Obesity-Induced Diabetes
Asmaa Elnagar, Khalifa El-Dawy, Hussein I. El-Belbasi, Ibrahim F. Rehan, Hamdy Embark, Zeinab Al-Amgad, Obeid Shanab, Elsayed Mickdam, Gaber E. Batiha, Salman Alamery, Samer S. Fouad, Simona Cavalu, Mohammed Youssef
Frontiers in Public Health.2022;[Epub] CrossRef - Time to doubling of serum creatinine in patients with diabetes in Ethiopian University Hospital: Retrospective follow-up study
Adeladlew Kassie Netere, Ashenafi Kibret Sendekie, Donovan Anthony McGrowder
PLOS ONE.2022; 17(9): e0274495. CrossRef - Deep Learning for Integrated Analysis of Insulin Resistance with Multi-Omics Data
Eunchong Huang, Sarah Kim, TaeJin Ahn
Journal of Personalized Medicine.2021; 11(2): 128. CrossRef - Arsenic Secondary Methylation Capacity Is Inversely Associated with Arsenic Exposure-Related Muscle Mass Reduction
Md. Khalequzzaman Sarker, Selim Reza Tony, Abu Eabrahim Siddique, Md. Rezaul Karim, Nazmul Haque, Zohurul Islam, Md. Shofikul Islam, Moriom Khatun, Jahidul Islam, Shakhawoat Hossain, Zahangir Alam Saud, Hideki Miyataka, Daigo Sumi, Aaron Barchowsky, Seiic
International Journal of Environmental Research and Public Health.2021; 18(18): 9730. CrossRef - Creatinine to Body Weight Ratio Is Associated with Incident Diabetes: Population-Based Cohort Study
Yoshitaka Hashimoto, Takuro Okamura, Masahide Hamaguchi, Akihiro Obora, Takao Kojima, Michiaki Fukui
Journal of Clinical Medicine.2020; 9(1): 227. CrossRef - ¿Debemos prestar más atención a la creatinina baja?
Carlos A. Amado Diago, José A. Amado Señaris
Endocrinología, Diabetes y Nutrición.2020; 67(7): 486. CrossRef - Arsenic exposure-related hyperglycemia is linked to insulin resistance with concomitant reduction of skeletal muscle mass
Victor Mondal, Zubaer Hosen, Faruk Hossen, Abu Eabrahim Siddique, Selim Reza Tony, Zohurul Islam, Md. Shofikul Islam, Shakhawoat Hossain, Khairul Islam, Md. Khalequzzaman Sarker, M.M. Hasibuzzaman, Ling-Zhi Liu, Bing-Hua Jiang, Md Mominul Hoque, Zahangir
Environment International.2020; 143: 105890. CrossRef - Noninvasive assessment of abdominal adipose tissues and quantification of hepatic and pancreatic fat fractions in type 2 diabetes mellitus
Manoj Kumar Sarma, Andres Saucedo, Christine Hema Darwin, Ely Richard Felker, Kavya Umachandran, Daniel Kohanghadosh, Edward Xu, Steve Raman, Michael Albert Thomas
Magnetic Resonance Imaging.2020; 72: 95. CrossRef - Should we pay more attention to low creatinine levels?
Carlos A. Amado Diago, José A. Amado Señaris
Endocrinología, Diabetes y Nutrición (English ed.).2020; 67(7): 486. CrossRef - Acute Effect of the Timing of Resistance Exercise and Nutrient Intake on Muscle Protein Breakdown
Wataru Kume, Jun Yasuda, Takeshi Hashimoto
Nutrients.2020; 12(4): 1177. CrossRef - Serum creatinine levels and risk of incident type 2 diabetes mellitus or dysglycemia in middle-aged Japanese men: a retrospective cohort study
Mamoru Takeuchi, Hironori Imano, Isao Muraki, Yuji Shimizu, Mina Hayama-Terada, Akihiko Kitamura, Takeo Okada, Masahiko Kiyama, Hiroyasu Iso
BMJ Open Diabetes Research & Care.2018; 6(1): e000492. CrossRef - Assessment of kidney dysfunction with cystatin C- and creatinine-based estimated glomerular filtration rate and predicting type 2 diabetes: Toranomon Hospital Health Management Center Study 21
Yoriko Heianza, Shigeko Hara, Kazumi Saito, Hiroshi Tsuji, Shiro Tanaka, Satoru Kodama, Tetsuro Kobayashi, Yasuji Arase, Hirohito Sone
Diabetes Research and Clinical Practice.2016; 113: 60. CrossRef - Profiling human blood serum metabolites by nuclear magnetic resonance spectroscopy: a comprehensive tool for the evaluation of hemodialysis efficiency
Marika Kromke, Martina Palomino-Schätzlein, Horst Mayer, Stefan Pfeffer, Antonio Pineda-Lucena, Burkhard Luy, Martin Hausberg, Claudia Muhle-Goll
Translational Research.2016; 171: 71. CrossRef - Safety evaluation of the consumption of high dose milk fat globule membrane in healthy adults: a double-blind, randomized controlled trial with parallel group design
Sayaka Hari, Ryuji Ochiai, Yasushi Shioya, Yoshihisa Katsuragi
Bioscience, Biotechnology, and Biochemistry.2015; 79(7): 1172. CrossRef - Brief Review of Articles in 'Endocrinology and Metabolism' in 2013
Won-Young Lee
Endocrinology and Metabolism.2014; 29(3): 251. CrossRef

 KES
KES
 PubReader
PubReader Cite
Cite